Methotrexate
General Information about Methotrexate
Side Effects
Dosage and Administration
Methotrexate, also recognized as MTX or amethopterin, is a medication generally used within the treatment of most cancers. It falls into the category of antimetabolites, that are medications that intrude with the expansion and reproduction of cancer cells. Methotrexate has been in use for the reason that Forties and stays a broadly used and efficient remedy for numerous kinds of most cancers.
Methotrexate is commonly used in the therapy of cancers that affect the blood, bone marrow, and certain solid tumors. These embody leukemia, lymphoma, and breast, lung, and head and neck cancers. It can additionally be used within the treatment of non-cancerous circumstances corresponding to rheumatoid arthritis, psoriasis, and extreme eczema.
What forms of most cancers can Methotrexate treat?
What is Methotrexate?
Methotrexate is a sort of folic acid antagonist, which means it works by blocking the action of an important vitamin known as folic acid. Folic acid is crucial for the manufacturing and restore of DNA, the genetic material in our cells. Cancer cells have the next demand for folic acid than healthy cells and for this reason they're significantly weak to methotrexate.
Like some other medication, methotrexate could cause unwanted aspect effects. However, these normally subside as the body gets used to the medicine. Common unwanted effects embody nausea, vomiting, hair loss, mouth sores, and fatigue. It can even reduce the number of white blood cells, which might increase the chance of an infection. To decrease unwanted effects, patients are advised to take folic acid supplements, stay hydrated, and avoid alcohol whereas on the medication.
Methotrexate has been a priceless and effective remedy choice for most cancers for many years. Its capacity to target and inhibit speedy cell progress has made it an essential weapon within the battle towards cancer. While it could have some unwanted effects and dangers, cautious monitoring and following the prescribed dosage can reduce these issues. Researchers proceed to study this medication and have discovered new ways to make use of it together with other remedies to enhance its effectiveness. Methotrexate has undoubtedly played a major function in bettering the prognosis for lots of sufferers with most cancers and will continue to be an necessary treatment possibility for years to come.
How does it work?
Risks and Precautions
Methotrexate works by targeting cells which are quickly dividing and rising in quantity, such as most cancers cells. It acts by binding to and inhibiting an enzyme called dihydrofolate reductase (DHFR), which is involved in the synthesis of folic acid. By blocking this enzyme, methotrexate prevents the manufacturing of recent DNA, thereby slowing down the expansion and spread of cancer cells.
The dosage of methotrexate varies depending on the sort and stage of cancer being handled, as properly as the patient’s overall well being. It may be administered in numerous methods, together with as a tablet, injection, or infusion. The treatment is usually given as soon as every week, but the frequency and duration of treatment may be adjusted based mostly on the patient’s response.
Methotrexate can have severe unwanted effects in uncommon cases. These embrace liver and kidney harm, lung issues, and decreased bone marrow operate. It shouldn't be used in sufferers with liver or kidney illness and in pregnant ladies, as it could possibly hurt the developing baby. Patients with a historical past of blood disorders, stomach ulcers, or who are taking certain drugs must also train warning when using methotrexate.
Conclusion
Nutritional practices and their relationship to clinical outcomes in critically ill childrenan international multicenter cohort study* medicine 2 times a day order methotrexate with paypal. Early enteral nutrition is associated with lower mortality in critically ill children. Use of a feeding protocol to improve nutritional support through early, aggressive, enteral nutrition in the pediatric intensive care unit. Intraoperative transfusionrelated acute lung injury in a child during calvarial vault remodeling. Transfusion-related acute lung injury after transfusion of maternal blood: a case-control study. Transfusion-related acute lung injury management in a pediatric intensive care unit. Blood product transfusions and clinical outcomes in pediatric patients with acute lung injury. Red blood cell transfusion threshold in postsurgical pediatric intensive care patients: a randomized clinical trial. Disseminated intravascular coagulation score is associated with mortality for children with shock. Towards definition, clinical and laboratory criteria, and a scoring system for disseminated intravascular coagulation. Prevention of a first stroke by transfusions in children with sickle cell anemia and abnormal results on transcranial Doppler ultrasonography. Current controversies in the management of idiopathic thrombocytopenic purpura during childhood. Continuous renal replacement therapy in children post-hematopoietic stem cell transplantation: the present and the future. Impact of continuous renal replacement therapy on oxygenation in children with acute lung injury after allogeneic hematopoietic stem cell transplantation. Outcomes of hematopoietic stem cell transplant patients who received continuous renal replacement therapy in a pediatric oncology intensive care unit. The morbidity and mortality of pediatric oncology patients presenting to the intensive care unit with septic shock. Improved outcomes of children with malignancy admitted to a pediatric intensive care unit. Intensive care unit mortality trends in children after hematopoietic stem cell transplantation: a meta-regression analysis. Changes in outcomes (1996-2004) for pediatric oncology and hematopoietic stem cell transplant patients requiring invasive mechanical ventilation. Evaluation of six risk factors for the development of bacteremia in children with cancer and febrile neutropenia. The diagnostic value of C-reactive protein, interleukin-8, and monocyte chemotactic protein in risk stratification of febrile neutropenic children with hematologic malignancies. Frequency of early death in children with acute leukemia presenting with hyperleukocytosis. Ventilator-associated pneumonia in pediatric intensive care unit patients: risk factors and outcomes. Tailoring the Institute for Health Care Improvement 100,000 Lives Campaign to pediatric settings: the example of ventilator-associated pneumonia. Ventilator-associated pneumonia in the pediatric intensive care unit: characterizing the problem and implementing a sustainable solution. Effectiveness of a multidimensional approach to reduce ventilator-associated pneumonia in pediatric intensive care units of 5 developing countries: international Nosocomial Infection Control Consortium findings. Impact of bloodstream infection on the outcome of children undergoing cardiac surgery. Pediatric trauma: differences in pathophysiology, injury patterns and treatment compared with adult trauma. Selection and nonoperative management of pediatric blunt trauma patients: the role of quantitative crystalloid resuscitation and abdominal ultrasonography. The most frequent cause of airway obstruction in the immediate postoperative period is the loss of pharyngeal muscle tone in a sedated or obtunded patient. The ability to strongly oppose the incisor teeth against a tongue depressor is a reliable indicator of pharyngeal muscle tone. Respiratory failure in the immediate postoperative period is often due to transient and rapidly reversible conditions such as splinting from pain, diaphragmatic dysfunction, muscular weakness, and pharmacologically depressed respiratory drive. Aggressive hydration with a balanced crystalloid solution provides the single most effective protection against contrast nephropathy. Identified risk factors include young age, endoprosthetic surgery, and core hypothermia. Multiple studies across different surgical specialties in elective and emergency cases have shown that postoperative delirium is associated with worse surgical outcomes, increased hospital length of stay, functional decline, higher rates of institutionalization, higher mortality, and higher cost and resource utilization. Its location in close proximity to the operating rooms facilitates rapid access to anesthesiologists for consultation and assistance. Vital signs are recorded as often as necessary but at least every 15 minutes while the patient is in the unit. Specific requirements and recommendations for patient monitoring and therapeutic intervention can be found in the Practice Standards and Guidelines drafted by the American Society of Anesthesiologists. They are recommendations designed to assist the healthcare provider in clinical decision making.
Enteroc-coated capsule containing cationic nanoparticles from oral insulin delivery medications you can take when pregnant order methotrexate 2.5 mg with visa. Treating inflammation and inflammatory pain inmocusa using mucosal-prolonged release bioadhesive therapeutic carriers. Mucus penetrating particles with high molecular weight and dense coatings cross-reference, United Stated of America. Nanocrystals, compositions, and methods that aid particle transport in mucus, vol. Mucus-penetrating budesonide nanosuspension enema for local treatment of inflammatory bowel disease, vol. Compressed granulated mucosal bioadhesive slow release carrier for delivering active principles. Controlled release formulations of enzymers, microorganisms, and antibodies with mucoadhesive polymers. Microparticulated vaccines for the oral or nasal vaccination and boostering of animals including fish. Mucoadhesive particulate formulation for inducing antigen-specific immune tolerance. Reverse thermal hydrogel preparations for use in the treatment of disorders of teurothelium. Ophtalmic formulations of reversed liquid crystalline phase materials and methods of using. Biodegradable thermoresponside 3-arm polyehtylene glycol poly(lactide-co-glycolide) co-polymer for ginseng administration. Hyaluronic acid based mucoadhesive threrapeutic compostion for the prevention and treatment of epithelial and mucosal lesions of the human body. Bioadhesive polymer-based controlled-release systems, production process and clinical uses thereof. Mucoadhesive xyloglucancontaining formulations useful in medical devices and in pharmaceutical fromulations. Methods for improving lid margin and tear film function and treatment of lid margin disease using tetracycline family antibiotics. Platelet lysate and bioadhesive compositions thereof for the treatment of mucositis. Introduction to nanomedicine for oral drug delivery Oral drug delivery is most preferred route of administration owing to its high patient compliance [1]. The most popular dosage forms for oral delivery include coated/uncoated tablets and capsules [2]. The potential delivery of these dosage forms depends on standard compression processes and coating ingredients, along with the use of various excipients. In addition, after administration, the transport of the active constituent is governed by the rate of hydration of the dosage form, which is directly influenced by their size distribution, shape and porosity [2], and that also defines the disintegration of the formulation [2, 3]. These formulations also face significant challenges because of their physiochemical instability (crystal growth or aggregation of sub-micron sized particles) and purity. Especially, newly developed macromolecules are either degraded by pH or enzymes in the gut or cannot permeate across the gut wall, leading to poor bioavailability. In this context, nano-sized drug carriers have attracted considerable attention due to their high surface area and precisely tuneable morphological and surface characteristics [48]. Over the past few decades, the advancement in the field of nano drug delivery played a significant role to achieve target specificity of therapeutics [915]. The materials used in the nanocomposites offer a range of size and shapes, varying in physicochemical and biological properties. In addition, these properties have been comprehensively investigated for their potential application in the biomedical field [4, 1620]. Apart from the size, dissolution and solubility of a drug and its carrier, there are the other challenges leading to poor bioavailability of the drugs. This article focuses on the effect of size, shape and surface charge of the nanoparticle carriers for efficient delivery of therapeutics via the oral route. However, challenges are even more prominent when it comes to the delivery of macromolecules such as peptides, monoclonal antibodies and recombinant proteins, due to their size, weak enzymatic stability and poor bioavailability across the intestinal epithelial tissue [22]. Additionally, the gastric emptying, the presence of food, and the microbiome make it one of the most complex sites to understand how nanomaterials behave after being orally delivered. These factors affect the stability and absorption of the drug into the systemic circulation [23]. Factors influencing cargo/drug integrity and absorption include the average length and area of the intestinal segment, pH and thickness of the mucosal layers, retention time, and bacterial and enzymatic diversity [27]. In the literature, various pH-sensitive hydrogels were documented to tackle the acidic and enzymatic environment. Then, the pH varies in the duodenum and small intestine, and thus, unwanted release of the active component can be prevented by regulating the pKa of the delivery system. Size, shape and surface charge considerations 145 the next extracellular biological obstacle faced by oral delivery systems are the presence of tight junctions between the epithelial cells. The transport across this barrier majorly depends on the size, shape and chemistry of the delivery systems. Other mechanisms involved in intestinal drug transport include receptor-mediated endocytosis. For example, intestinal membrane lectin could potentially bind to various drug loaded polymeric matrices, thus resulting in slow diffusion of the drug. The next barrier is the mucus layer, which obstructs the interaction of the cargo with the epithelial layer. Under homeostatic conditions in the gut, the mucus layer is thick and poses a physical barrier to prevent the epithelium damage, which may lead to activation of innate and adaptive immune responses [3840]. In addition to mucins, the mucus layer also contains water, various salts, carbohydrates, gut bacteria and many other key components that have specific roles in maintaining gut homeostasis.
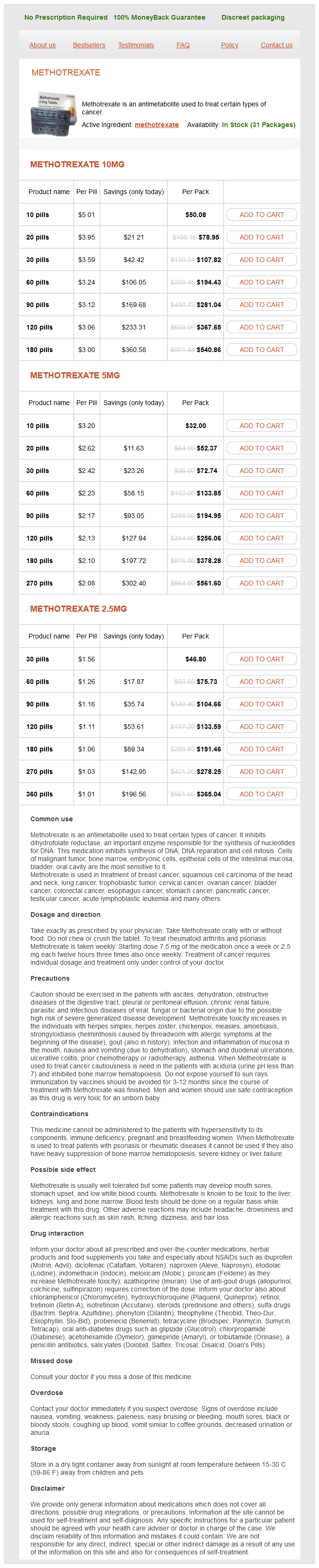
Methotrexate Dosage and Price
Methotrexate 10mg
- 10 pills - $50.08
- 20 pills - $78.95
- 30 pills - $107.82
- 60 pills - $194.43
- 90 pills - $281.04
- 120 pills - $367.65
- 180 pills - $540.86
Methotrexate 5mg
- 10 pills - $32.00
- 20 pills - $52.37
- 30 pills - $72.74
- 60 pills - $133.85
- 90 pills - $194.95
- 120 pills - $256.06
- 180 pills - $378.28
- 270 pills - $561.60
Methotrexate 2.5mg
- 30 pills - $46.80
- 60 pills - $75.73
- 90 pills - $104.66
- 120 pills - $133.59
- 180 pills - $191.46
- 270 pills - $278.25
- 360 pills - $365.04
Particular attention should be given to monitoring oxygenation treatment 3rd degree av block order methotrexate with paypal, ventilation, circulation, level of consciousness, and temperature. During recovery from all anesthetics, a quantitative method of assessing oxygenation such as pulse oximetry shall be employed in the initial phase of recovery. Nausea and vomiting, the need for upper airway support, and hypotension were the most frequent individual complications. In 2002, airway/respiratory problems (183, 43%) and cardiovascular events (99, 24%) accounted for the majority of 419 recovery room incidents reported to the Australian Incident Monitoring Study database (Table 80. In an awake patient, opening of the upper airway is facilitated by the contraction of the pharyngeal muscles at the same time that negative inspiratory pressure is generated by the diaphragm. As a result, the tongue and soft palate are pulled forward, tenting the airway open during inspiration. This pharyngeal muscle activity is depressed during sleep, and the resulting decrease in tone can promote airway obstruction. A vicious cycle then ensues wherein the collapse of compliant pharyngeal tissue during inspiration produces a reflex compensatory increase in respiratory effort and negative inspiratory pressure that promotes further airway obstruction. Collapse of the chest wall and protrusion of the abdomen with inspiratory effort produces a rocking motion that becomes more prominent with increasing airway obstruction. Support of the airway is needed until the patient has adequately recovered from the effects of drugs administered during anesthesia. In selected patients, placement of an oral or nasal airway, laryngeal mask airway, or endotracheal tube may be required. With an endotracheal tube in place, end-tidal carbon dioxide concentrations and tidal volumes may indicate adequate ventilation while the ability to maintain a patent upper airway and clear upper airway secretions remains compromised. A decline in this ratio may not be appreciated until it reaches a value less than 0. Clinical evaluation includes grip strength, tongue protrusion, the ability to lift the legs off the bed, and the ability to lift the head off the bed for a full 5 seconds. However, studies have shown that the 5-second head lift is remarkably insensitive and should not routinely be used to assess recovery from neuromuscular blockade. The ability to strongly oppose the incisor teeth against a tongue depressor is a more reliable indicator of pharyngeal muscle tone. Common factors include respiratory acidosis and hypothermia, alone or in combination. Simple measures such as warming the patient, airway support, and correction of electrolyte abnormalities can facilitate recovery from neuromuscular blockade. It typically occurs in the transitional period when the extubated patient is emerging from general anesthesia yet not fully awake. If these maneuvers fail, one should proceed with a full dose of an induction agent and intubating dose of a muscle relaxant to enable the practitioner to perform an emergent tracheal intubation; attempting to pass a tracheal tube forcibly through a glottis that is closed because of laryngospasm is not acceptable. Although facial and scleral edema is an important physical sign that can alert the clinician to the presence of airway edema, visible external signs may not accompany significant edema of pharyngeal tissue (see also Chapter 44). Patients who have had a difficult intraoperative intubation and/or airway instrumentation may also have increased airway edema from direct injury. With occlusion of the proximal end of the endotracheal tube, the patient is then asked to breathe around the tube. An alternative method involves measuring the intrathoracic pressure required to produce a leak around the endotracheal tube with the cuff deflated. This method was originally used to evaluate pediatric patients with croup before extubation. Lastly, 80 · the Postanesthesia Care Unit 2591 when ventilating patients in the volume control mode, one can measure the exhaled tidal volume before and after cuff deflation. In order to facilitate the reduction of airway edema, one may sit the patient upright to ensure adequate venous drainage, and consider administering a diuretic and intravenous dexamethasone (4-8 mg every 6 hours for 24 hours), which may help decrease airway swelling. External airway compression is most often caused by hematomas following thyroid, parathyroid, or carotid surgical procedures. Patients may complain of pain and/or pressure, dysphagia, and can demonstrate signs of respiratory distress as the pressure from the expanding hematoma within the tissue can disrupt both venous and lymphatic drainage, both of which can further exacerbate airway swelling. Mask ventilation may not be possible in a patient with severe upper airway obstruction resulting from edema or hematoma. In the case of a hematoma, an attempt can be made to decompress the airway by releasing the clips or sutures on the wound and evacuating the hematoma. This maneuver is recommended as a temporizing measure, but it will not effectively decompress the airway if a significant amount of fluid or blood (or both) has infiltrated the tissue planes of the pharyngeal wall. If emergency tracheal intubation is required, then ready access to difficult airway equipment and surgical backup to perform an emergency tracheostomy are crucial, as one should assume increased difficulty secondary to laryngeal and airway edema, possible tracheal deviation, and a compressed tracheal lumen. If the patient is able to move adequate air via spontaneous ventilation, then an awake technique is often preferred as visualization of the cords by direct laryngoscopy may not be possible. One may also employ the use of ketamine, dexmedetomidine, and clonidine, all of which can also decrease postoperative opioid requirements. In addition, the use of goal-directed fluid strategies should be utilized with consideration of lower salt-containing substances, as these patients are more prone to fluid shifts, which can worsen airway edema. Management of Upper Airway Obstruction An obstructed upper airway requires immediate attention. Efforts to open the airway by noninvasive measures should be attempted before reintubation of the trachea. After successfully opening the upper airway and ensuring adequate ventilation, the cause of the upper airway obstruction should be identified and treated.