Minocin
General Information about Minocin
Another frequent use of minocin is for treating urinary tract infections (UTIs). These kinds of infections are attributable to bacteria entering the urinary tract and can cause discomfort and pain. Minocin is often prescribed to treat UTIs as a outcome of it could attain excessive concentrations in the urine, making it simpler at killing the micro organism causing the infection. This medicine is also used to deal with other forms of infections corresponding to tick fever, chlamydia, gonorrhea, and respiratory infections.
In conclusion, minocin is a highly effective antibiotic that has been used for many years to deal with numerous bacterial infections. Its broad spectrum of protection and comparatively low probability of resistance make it a most well-liked selection for docs and patients alike. However, it's important to make use of this medicine responsibly and cling to the beneficial dosage and duration of therapy to avoid any potential unwanted effects. If you may be experiencing symptoms of a bacterial an infection, seek the guidance of with your physician to determine if minocin is the best remedy choice for you.
Minocin is out there in each oral and injectable types, making it handy for sufferers who have issue swallowing tablets. The dosage and period of treatment will vary relying on the sort and severity of the infection. It is essential to take the treatment as prescribed and complete the full course of remedy to make sure the infection is totally eradicated. If a affected person stops taking minocin too soon, the infection is in all probability not absolutely treated, and the micro organism can turn out to be proof against the treatment.
Minocin is usually thought-about protected for most individuals, but there are specific precautions that have to be taken when using this medication. Those with kidney or liver illness, as well as pregnant or breastfeeding ladies, should consult with their physician before taking minocin. It is also important to keep away from prolonged exposure to daylight or tanning beds whereas taking minocin, as it could possibly make the skin extra delicate to UV rays, resulting in sunburns.
Minocin, also referred to as minocycline, is a robust antibiotic that has been in use for over 50 years. Originally developed as a broad-spectrum antibiotic to deal with a wide selection of infections, minocin has proven to be effective in treating a wide range of bacterial infections. From urinary tract infections to extreme zits, minocin has been a go-to treatment for many docs and patients alike.
Minocin belongs to a class of antibiotics often recognized as tetracyclines. These antibiotics work by stopping bacteria from producing important proteins wanted for his or her progress, thus stopping the bacterial an infection in its tracks. Unlike most antibiotics, minocin can successfully deal with both gram-positive and gram-negative micro organism, making it a flexible drug for treating different types of infections.
One of the commonest makes use of of minocin is for the remedy of pimples. Acne is a skin situation that affects millions of individuals worldwide, and it is caused by an overgrowth of micro organism on the pores and skin. Minocin might help to reduce back the number of acne-causing bacteria on the skin, in the end resulting in clearer skin. In addition to its antibacterial properties, minocin additionally has anti-inflammatory results that may assist to reduce back the redness and swelling related to zits.
Like any medication, minocin does have some potential unwanted effects, though they're comparatively rare. Common unwanted effects include nausea, vomiting, diarrhea, and dizziness. In some instances, more extreme side effects such as liver or kidney injury, allergic reactions, and a condition called intracranial hypertension might happen. It is essential to tell your doctor when you expertise any of those unwanted effects whereas taking minocin.
Crypts of Lieberkühn bacteria helicobacter pylori sintomas cheap generic minocin canada, or intestinal glands, are simple tubular glands that increase the intestinal surface area. The crypts are formed by invaginations of the mucosa between adjacent intestinal villi. The muscularis consists of inner circular smooth muscle and outer longitudinal smooth muscle. A thin layer of loose connective tissue is covered by the visceral peritoneum, a serosa layer lined by a simple squamous epithelium, or mesothelium. Branches of the submucosal plexus supply capillaries to the muscularis and intestinal mucosa. Arterioles derived from the submucosal plexus enter the mucosa of the small intestine and give rise to two capillary plexuses: 1. Intestinal motility: Muscular contraction patterns Segmentation Intestinal contents are mixed within an intestinal segment. Orad region Peristalsis Contents advance along the intestine when proximal contraction is coordinated with relaxation below. This is accomplished when muscular contraction activity is not coordinated and the intestine becomes transiently divided into segments. To propel the intestinal contents when there is a proximal (orad) contraction coordinated with a distal (aborad; Latin ab, from; os, mouth; away from the mouth) relaxation. When coordinated contraction-relaxation occurs sequentially, the intestinal contents are propelled in an aborad direction. Histologic differences between the duodenum, jejunum, and ileum Aborad relaxation Aborad propulsion Caudad region villus and upper portion of the crypts of Lieberkühn. The pericryptal capillary plexus supplies the lower half of the crypts of Lieberkühn. A single blind-ending central lymphatic capillary, the lacteal, is present in the core or lamina propria of a villus. The lacteal is the initiation of a lymphatic vessel that, just above the muscularis mucosae, forms a lymphatic plexus whose branches surround a lymphoid nodule in the mucosa-submucosa. Efferent lymphatic vessels of the lymphoid nodule anastomose with the lacteal and leave the digestive tube through the mesentery, together with the blood vessels. Innervation and motility of the small intestine Motility of the small intestine is controlled by the autonomic nervous system. Neurons of the plexuses receive intrinsic input from the mucosa and muscle wall of the small intestine and extrinsic input from the central nervous system through the parasympathetic (vagus nerve) and sympathetic nerve trunks. The duodenum extends from the pyloric region of the stomach to the junction with the jejunum and has the following characteristics: 1. The duodenum is surrounded by an incomplete serosa and an extensive adventitia rather than a serosa. The duodenum collects bile and pancreatic secretions transported by the common bile duct and pancreatic duct, respectively. The sphincter of Oddi is present at the terminal ampullary portion of the two converging ducts. It has long finger-like villi and a well-developed lacteal in the core of the villus. As in the jejunum, Paneth cells are found at the base of the crypts of Lieberkühn. Epithelial cells of the villus and crypt of Lieberkühn Brush border Enterocyte Capillary villus plexus Goblet cell Lacteal Lumen of the crypt Villus Intestinal gland or crypt cross-linked by an intestinal isoform of spectrin to an adjacent rootlet. The end portion of the rootlet attaches to cytokeratin-containing intermediate filaments. The terminal web is responsible for maintaining the upright position and shape of the microvillus and anchoring the actin rootlets. A surface coat or glycocalyx, consisting of glycoproteins as integral components of the plasma membrane, covers each microvillus. We discuss Paneth cells within the context of the protection mechanisms of the small intestine. Enterocytes: Absorptive cells the absorptive intestinal cell or enterocyte has an apical domain with a prominent brush border (also called a striated border), ending on a zone, called the terminal web, which contains transverse cytoskeletal filaments. The brush border of each absorptive cell contains about 3000 closely packed microvilli, which increase the surface luminal area 30-fold. The actin bundle core is anchored to the plasma membrane by formin (protein of the cap), myosin I, and the calcium-binding protein calmodulin. Each actin bundle projects into the apical portion of the cell as a rootlet, which is 504 16. These oligosaccharides reduce carbohydrates to monosaccharides, which can be transported into the enterocyte by carrier proteins. Fructose (derived, together with glucose, from the breakdown of sucrose) enters and leaves the enterocyte by passive diffusion. A genetic defect in lactase prevents the absorption of lactose-rich milk, causing diarrhea (lactose intolerance). Lactose is converted by intestinal bacteria to lactic acid, methane, and H2 gas causing an osmotic diarrhea by drawing water into the intestinal lumen. Therefore, the brush border not only increases the absorptive surface of enterocytes but is also the site where enzymes are involved in the terminal digestion of carbohydrates and proteins. Final breakdown of oligopeptides, initiated by the action of gastric pepsin, is extended by pancreatic trypsin, chymotrypsin, elastase, and carboxypeptidases A and B. Enterokinase and aminopeptidase, localized in the microvilli, degrade oligopeptides into dipeptides, tripeptides, and amino acids before entering the enterocyte across symporter channels together with Na+.
Histologic organization of the adrenal cortex the adrenal glands (Latin ad antibiotic resistance kit order minocin 50 mg, near; ren, kidney) are associated with the superior poles of each kidney. Each gland consists of a yellowish outer cortex (80% to 90% of the gland) and a reddish inner medulla (10% to 20%). Each adrenal gland is surrounded by perinephritic fat and enclosed by the renal fascia. An arterial plexus, derived from three adrenal arteries, is located in the adrenal gland capsule. Zona glomerulosa During the early stage of gestation, the adrenal cortex synthesizes dehydroepiandrosterone, a precursor of the synthesis of estrogen by the placenta. The interaction between the fetal adrenal cortex and the placenta constitutes the fetoplacental unit (see Chapter 23, Fertilization, Placentation, and Lactation). Glucocorticoids, either of maternal origin or synthesized from placental progesterone by the fetus, are essential for three main developmental events: 1. Its cells aggregate into a glomerulus-like arrangement and have a moderate amount of lipid droplets in the cytoplasm. Aldosterone has a half-life of 20 to 30 minutes and acts directly on the distal convoluted tubule and collecting tubule, where it increases Na+ reabsorption and water (as a consequence of Na+ reabsorption) and excretion of K+and H+. During aldosterone action, aldosterone binds to intracellular receptor proteins to activate transcription Adrenal cortex 19. Histologic organization of the adrenal gland Capsule Capsule 1 Zona glomerulosa 1 Glomerulus Zona glomerulosa Zona fasciculata 2 Zona fasciculata 2 Capillary 3 Zona reticularis Spongiocyte Zona fasciculata 4 Medulla 3 1 the zona glomerulosa is a narrow subcapsular zone contiguous on its inner side with the zona fasciculata. The zona glomerulosa consists of concentrically arranged cells surrounded by a stroma containing capillaries. The cells contain a few lipid droplets and a well-developed smooth endoplasmic reticulum. It consists of polygonal cells arranged in vertical columns or fascicles perpendicular to the capsule. The cells contain a vacuolated cytoplasm reflecting the accumulation of lipid droplets containing cholesterol and its metabolites. It consists of anastomosing cells forming a reticulum or network surrounded by fenestrated capillaries. The cells contain a brown pigment (lipofuscin) contrasting with the lighter staining of the zona fasciculata. Catecholamines of the medulla generate a brown color when exposed to air or the oxidizing agent potassium dichromate (chromaffin reaction). Capillary Lipofuscin Zona reticularis 4 Venous sinusoid Medulla Catecholaminesecreting cell 594 19. Aldosterone-responsive cells do not respond to the glucocorticoid cortisol because cortisol is converted in the liver to cortisone by the enzyme 11 -hydroxysteroid dehydrogenase. Zona fasciculata the zona fasciculata (Latin fascis, bundle) makes up 75% of the cortex. It consists of cuboid cells, with the structural features of steroid-producing cells, arranged in longitudinal cords separated by cortical fenestrated capillaries, or sinusoids. When lipids are extracted during histologic preparation or are unstained by the standard hematoxylin-eosin (H&E) procedures, the cells of the zona fasciculata display a foamy appearance and are called spongiocytes. Well-developed smooth endoplasmic reticulum, also with enzymes involved in the synthesis of steroid hormones. In the liver, cortisol stimulates gluconeogenesis to increase the concentration of glucose in blood. It becomes useful to understand fluctuations in blood glucose levels in the diabetic patient. An anti-inflammatory effect: Cortisol suppresses tissue responses to injury and decreases cellular and humoral immunity. It is interesting to note that the female hormone estradiol derives from the male hormone testosterone, and that testosterone has the female hormone progesterone as a precursor. The adrenal gland is the major source of androgens in women; these androgens stimulate the growth of pubic and axillary hair during puberty. Adrenal medulla the zona reticularis (Latin rete, net) makes up 5% to 10% of the cortex. Cells of the zona reticularis form an anastomosing network of short cellular cords separated by fenestrated capillaries. The adrenal medulla contains chromaffin cells, so named because of their ability to acquire a brown coloration when exposed to an aqueous solution of potassium dichromate. This reaction is due to the oxidation of catecholamines by chrome salts to produce a brown pigment. The cytoplasm of chromaffin cells contains membrane-bound dense granules consisting in part of matrix proteins, called chromogranins, and one class of catecholamine, either epinephrine or norepinephrine (adrenaline or noradrenaline). Minimal secretion of dopamine also occurs, but the role of adrenal dopamine is not known. Catecholamines are secreted into the blood instead of being secreted into a synapse, as in postganglionic terminals. The adrenal medulla is innervated by sympathetic preganglionic fibers that release acetylcholine. These two cell populations can be distinguished at the electron microscope level by the morphology of the membranebound granules: 1. Note an important difference with cells of the adrenal cortex: cells from the adrenal cortex do not store their steroid hormones in granules. Fine structure of steroid-producing cells of the adrenal cortex (zona fasciculata) Spongiocyte of the zona fasciculata Fenestrated capillary Cluster of lipid droplets Spongiocytes the ultrastructure of cells of the zona fasciculata and their close relationship with capillaries lined by fenestrated endothelial cells demonstrate their participation in the synthesis of steroid hormones released into the blood vascular system. Like steroid-producing cells of the theca interna and corpus luteum of the ovaries and Leydig cells of the testes, cells of the zona fasciculata display three characteristic structural features representative of steroidogenesis: (1) lipid droplets containing cholesterol; (2) mitochondria with tubular cristae housing the enzymes involved in steroidogenesis; and (3) smooth endoplasmic reticulum, also containing membrane-associated enzymes involved in the production of steroids.
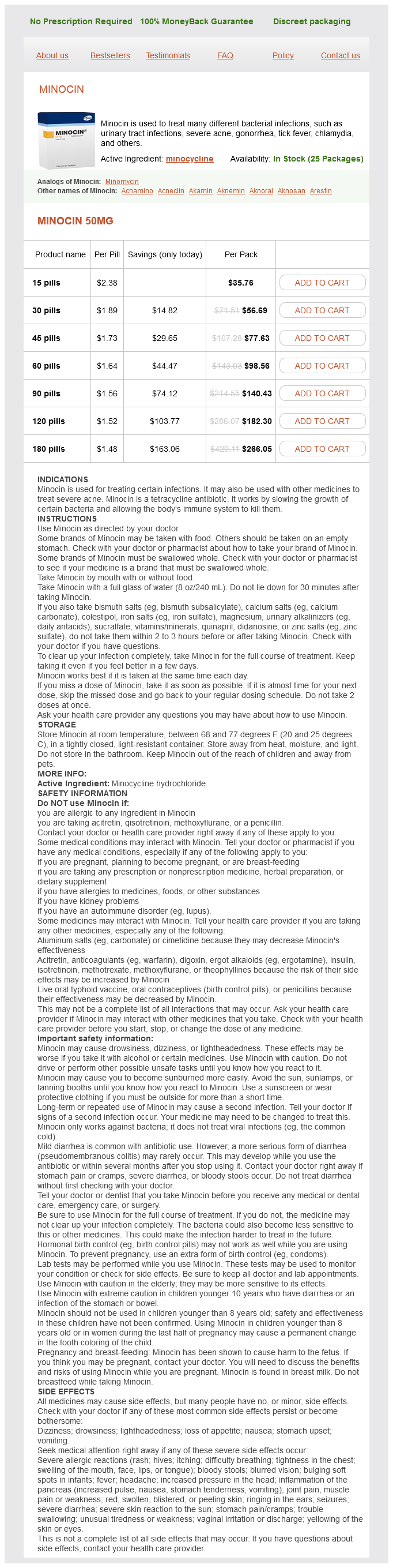
Minocin Dosage and Price
Minocin 50mg
- 15 pills - $35.76
- 30 pills - $56.69
- 45 pills - $77.63
- 60 pills - $98.56
- 90 pills - $140.43
- 120 pills - $182.30
- 180 pills - $266.05
Migratory pathways of bulge stem cells Interfollicular epidermis Differentiated epidermal cell (stratum corneum) Bulge stem cells in the bulge region (located at the external root sheath of the hair follicle) can follow independent cell migration pathways: 1 In the bulge stem cellepidermis pathway antibiotic 3 pack purchase minocin cheap online, bulge stem cells migrate upward into the interfollicular epidermis along the basal lamina. Bulge stem cells proliferate within the stratum basale and differentiate vertically into the keratin-rich cells of the stratum corneum. Squamous cell carcinoma, basal cell carcinoma, and hair-follicle tumors can originate from cells exiting the bulge following activation of specific genetic pathways. Regulatory factors (bone morphogenetic proteins and Wnt/ -catenin signaling) released by cells of the dermal papilla and neighboring adipose cells, are essential for maintaining the proliferative potential of the matrix and their differentiation into the various hair cell lineages. Basal lamina Epidermis External root sheath Internal root sheath Bulge stem cell Bulge Hair shaft 2 1 Bulge stem cell epidermis pathway Arrector pili muscle Bulge stem cell sebaceous gland pathway Sebaceous gland 3 Bulge stem cell hair pathway Internal root sheath Matrix cells Adipose cells Dermal papilla Connective tissue sheath vascular dilation and plasma leakage, thereby causing edema in the injury surrounding area. In summary, the nociceptive receptors (the pain detectors) are found near the skin surface. Merkel disks and Meissner corpuscles, fine mechanoreceptor, are located at the epidermal-dermal junction so they can detect gentle touch. Pacinian corpuscles and Ruffini endings, the large encapsulated mechanoreceptors, are found in the deep dermis and hypodermis and respond to transient deeper touch. The lepromatous reaction, characterized by numerous macrophages in the dermis with intracellular acid-fast bacilli. The tuberculoid reaction, identified by noncaseating granulomas consisting of macrophages, multinucleated giant cells, and lymphocytes (T cells). Hypodermis (superficial fascia) Leprosy (lepra) is a chronic infection of the skin, nasal mucosa, and peripheral nerves. It is caused by Mycobacterium leprae, an intracellular bacillus found in Schwann cells, endothelial cells and macrophages of the skin. There are two histologic types of leprosy: the hypodermis, or subcutaneous layer of the skin, is a deeper continuation of the dermis. It consists of loose connective tissue and adipose cells forming a layer of variable thickness depending on its location in the body. The hypodermis facilitates mobility of the skin, and the adipose tissue contributes to thermal insulation and storage of metabolic energy and acts as a shock absorber. No adipose tissue is found in the subcutaneous portion of the eyelids, clitoris, or penis. Epidermal derivatives: Hair (pilosebaceous unit) Scattered in the epidermis are the hair follicles. Structure of the hair follicle Hair follicle Hair shaft Hair follicle (cross section) Epidermis Dermis Hair bulb 3 2 Hypodermis 1 Medulla Hair shaft Cortex Cuticle External root sheath (epidermis downgrowth) Internal root sheath (formed in the hair bulb) Connective tissue sheath Hair follicle Connective External root Internal root tissue sheath sheath Cortex sheath Cuticle Medulla 1. Cuticle of the Hair shaft inner root sheath Connective tissue sheath External root sheath Internal root sheath Hair cortex (tangential section) Cells with trichohyalin granules Duct of sebaceous gland Keratogenous zone, where maturing cells of the hair follicle accumulate hard keratin (keratinization) Epithelial cells covering the apex of the dermal papilla give rise to the medulla of the hair. Hair bulb Matrix cells Dermal papilla Zone of dividing cells of the hair matrix, comparable to the stratum basale of the epidermis. This zone contains melanocytes that give color to the hair by passing melanin to the matrix cells. Patients with Griscelli syndrome have silvery hair because of a mutation in the myosin Va gene involved in the transport of melanin-containing melanosomes. A hair follicle primordium (called the hair germ) forms as a cell aggregate in the basal layer of the epidermis, induced by signaling molecules derived from fibroblasts of the dermal mesoderm. As basal epidermal cell clusters extend into the dermis, dermal fibroblasts form a small nodule (called a dermal papilla) under the hair germ. The dermal papilla pushes into the core of the hair germ, whose cells divide and differentiate to form the keratinized hair shaft. The first adult hair follicle cycle starts once morphogenesis is completed about 18 days after birth, the first hair in the human embryo is thin, unpigmented, and spaced, and is called lanugo. Terminal hair replaces vellus, which remains in the so-called hairless parts of the skin (such as the forehead of the adult and armpits of infants). Hair follicles are tubular invaginations of the epidermis responsible for the growth of hair. During the first 28 days of the telogen phase, hair follicles become quiescent because of growth inhibitory signals from the dermis (mainly from bone morphogenetic proteins). Increased Wnt/ -catenin signaling promotes stem cell activation to initiate the growth of new hair during the transition from telogen to anagen. Anagen, catagen and telogen will sequentially continue during the life of the individual. The hair shaft is a filamentous keratinized structure present almost all over the body surface, except on the thick skin of the palms and soles, the sides of the fingers and toes, the nipples, and the glans penis and the clitoris, among others. A cross section of the hair shaft of thick hair reveals three concentric zones containing keratinized cells: 1. A vascularized connective tissue core (dermal papilla) projects into the hair bulb, in close proximity to matrix cells. The keratinization of the hair and internal root sheath occurs in a region called the keratogenous zone, the transition zone between maturing epidermal cells and hard keratin. The autonomic nervous system controls the arrector pili muscle, which contracts during fear, strong emotions, and cold temperature. The hairs stand up and the attachment site of the muscle bundle at the epidermis forms a small groove, the so called goose flesh. The hair follicle is associated with sebaceous glands with their excretory duct connected to the lumen of the hair follicle. When the arrector pili muscle contracts and the hair stands up, sebum is forced out of the sebaceous gland into the lumen of the hair follicle. The color of the hair depends on the amount and distribution of melanin in the hair shaft. Red hair has a chemically distinct melanin, and melanosomes are round rather than ellipsoid.