Minomycin
General Information about Minomycin
Dosage and Administration
Minomycin works by inhibiting the expansion and copy of bacteria. It does this by interfering with the manufacturing of important proteins that are essential for the bacteria to outlive. This ultimately results in the death of the micro organism, thus eliminating the an infection.
Minomycin is not beneficial for pregnant or breastfeeding ladies as it could have an effect on fetal improvement and will cross into breast milk. It is also not really helpful for youngsters under the age of eight, as it may possibly have an effect on the event of their teeth and bones.
Before starting Minomycin, it could be very important inform your doctor if you have any underlying medical circumstances, such as liver or kidney disease. It can also be essential to let your physician find out about any other drugs you are taking, including over-the-counter and natural dietary supplements, as they could interact with Minomycin.
Minomycin is mostly well-tolerated, however like another treatment, it may possibly have some unwanted effects. Common unwanted side effects of Minomycin include nausea, vomiting, abdomen upset, and diarrhea. These can normally be managed by taking the capsules with meals. Less frequent unwanted effects embrace headache, dizziness, and pores and skin rash. In some rare cases, Minomycin may cause severe allergic reactions, which require quick medical consideration.
Minomycin is a broad-spectrum antibiotic that's used for treating a variety of bacterial infections. It belongs to the tetracycline household and is on the market in capsule form. Minomycin capsules are primarily used to treat infections in the respiratory tract, urinary tract, pores and skin, and intestinal system. It can be efficient in treating acne and certain sexually transmitted infections.
Minomycin capsules are available in strengths of 50 mg, one hundred mg, and 200 mg. The dosage and length of therapy rely upon the severity and sort of an infection being handled. The capsules are often taken orally, with or without food, and must be swallowed complete with a full glass of water.
Precautions and Side effects
Minomycin is the brand name for the generic drug minocycline. It was first developed within the 1960s and has since been used extensively to treat a variety of infections. Its effectiveness in opposition to a broad range of bacteria makes it a well-liked selection among physicians.
It is essential to complete the total course of remedy, even when the symptoms enhance, as stopping the medicine prematurely can lead to a recurrence of the an infection or antibiotic resistance.
How does Minomycin work?
Minomycin is effective against a variety of bacteria, together with staphylococcus, streptococcus, and mycoplasma. It can also be effective in opposition to some strains of drug-resistant micro organism.
Minomycin is a extremely effective and broadly used antibiotic for treating a selection of bacterial infections. Its versatility and effectiveness make it a preferred choice amongst physicians. However, like any other treatment, it is very important use Minomycin as prescribed and to tell your doctor of any side effects or potential interactions with other medications.
Conclusion
If you're experiencing symptoms of a bacterial infection, don't hesitate to consult a well being care provider who could prescribe Minomycin for therapy. With proper usage, Minomycin can effectively get rid of the infection and allow you to get back to your wholesome self very quickly.
This diagnosis is suggested by fever with a known tick exposure during the preceding 3 weeks antibiotics for uti levaquin order minomycin online, thrombocytopenia and/or leukopenia, and increased serum aminotransferase levels. Retrospective serodiagnosis requires a consistent clinical picture and a fourfold increase in E. Although poorly studied, rifampin may be suitable when doxycycline is contraindicated. The use of protective clothing and tick repellents, careful postexposure tick searches, and prompt removal of attached ticks probably diminish infection risk. White-footed mice, squirrels, and white-tailed deer in the United States and red deer in Europe are natural reservoirs for A. A minority of patients develop nausea, vomiting, or diarrhea (2239%); cough (27%); or confusion (17%). Rash (6%) is almost invariably concurrent erythema migrans attributable to Lyme disease. Most patients develop thrombocytopenia (75%) and/or leukopenia (55%) with increased serum hepatic aminotransferase levels (83%). Severe complications occur most often in the elderly and include adult respiratory distress syndrome, a toxic shocklike syndrome, and life-threatening opportunistic infections. While co-infections with Borrelia burgdorferi and Babesia microti (transmitted by the same tick vector[s]) occur, there is little evidence of comorbidity or persistence. Peripheral-blood film examination for neutrophil morulae can yield a diagnosis in 2075% of infections. Since seroprevalence is high in some regions, a single acute-phase titer should not be used for diagnosis. Very few organisms and a strong cellular response are observed in patients with acute Q fever, while many organisms and a moderate cellular response occur in chronic Q fever. However, cats, rabbits, pigeons, and dogs also serve as sources for transmission of C. The wildlife reservoir is extensive and includes ticks, coyotes, gray foxes, skunks, raccoons, rabbits, deer, mice, bears, birds, and opossums. At the time of parturition, the bacteria are released into the air, and infection follows inhalation of aerosolized organisms by a susceptible host. An outbreak of Q fever at a horse-boarding ranch in Colorado in 2005 was due to spread of infection from two herds of goats that had been acquired by the owners. Of 138 persons who lived within 1 mile of the ranch and who were also tested, 11 (8%) had evidence of C. Persons at risk for Q fever include abattoir workers, veterinarians, farmers, and other individuals who have contact with infected animals (particularly newborn animals) or products of conception. The ingestion of contaminated milk in some geographic areas probably represents a major route of transmission to humans. A recent outbreak of Q fever associated with ingestion of raw milk confirms the oral route of transmission. In rare instances, person-to-person transmission follows labor and childbirth in an infected woman, autopsy of an infected individual, or blood transfusion. Crushing an infected tick between the fingers has resulted in Q fever; the implication is that percutaneous transmission can occur. The number of reported cases of Q fever in the United States ranges from 28 to 54 per year. More than 70% of these cases occur in males, and April, May, and June are the most common months for acquisition. Q fever continues to be common in Australia, with 30 cases per 1 million population per year. Cases among abattoir workers in Australia declined dramatically as a result of a vaccination program. An outbreak of Q fever began in the Netherlands in 2007, and by 2010 more than 4000 cases had been reported. The outbreak was due to a combination of high-density goat farming in areas abutting large urban populations and environmental factors. Farms where spread did not occur had high vegetation densities and lower groundwater concentrations. In the Netherlands outbreak, sequelae of infection in pregnant women were rare; this was not the case among pregnant women elsewhere. In a large outbreak in Switzerland, symptomatic infection occurred five times more often among persons >15 years of age than among younger individuals. In many outbreaks, men are affected more commonly than women; the proposed explanation is that female hormones are partially protective. Clinical Manifestations · acUte Q fever the symptoms of acute Q fever are nonspecific; common among them are fever, extreme fatigue, photophobia, and severe headache that is frequently retro-orbital. Other symptoms include chills, sweats, nausea, vomiting, and diarrhea, each occurring in 520% of cases. Thrombocytopenia occurs in ~25% of patients, and reactive thrombocytosis (with platelet counts exceeding 106/L) frequently develops during recovery. Chest radiography can show opacities similar to those seen in pneumonia caused by other pathogens, but multiple rounded opacities in patients in endemic areas suggest a diagnosis of Q fever pneumonia. In one series, it resulted in premature birth in 35% of cases and in abortion or neonatal death in 43%. Neonatal death (previous or current) and lower infant birth weight are three times more likely among women seropositive for C. Acalculous cholecystitis, pancreatitis, lymphadenopathy, spontaneous rupture of the spleen, transient hypoplastic anemia, bone marrow necrosis, hemolytic anemia, histiocytic hemophagocytosis, optic neuritis, and erythema nodosum were less common manifestations. Long-term persistence of a noninfective, nonbiodegraded complex of Coxiella cell components, with its antigens and specific lipopolysaccharide, has been detected in the affected persons.
It was formerly thought that the majority of cases of ocular disease were due to congenital infection bacterial endospore minomycin 50 mg buy low cost. New ocular toxoplasmosis in immunocompetent individuals occurs more commonly than was previously appreciated and has been associated with outbreaks in Victoria (British Columbia) and in South America. Macular involvement occurs, with loss of central vision, and nystagmus is secondary to poor fixation. The ophthalmologic examination reveals yellow-white, cotton-like patches with indistinct margins of hyperemia. Lesions usually are located near the posterior pole of the retina; they may be single but are more commonly multiple. Congenital lesions may be unilateral or bilateral and show evidence of massive chorioretinal degeneration with extensive fibrosis. Histologic examination of lymph nodes may suggest the characteristic changes described above. Demonstration of tachyzoites in lymph nodes establishes the diagnosis of acute toxoplasmosis. Isolates can be genotyped and polymorphic sequences can be obtained, with consequent identification of the precise strain. Molecular epidemiologic studies with polymorphic markers have been useful in correlating clinical signs and symptoms of disease with different T. The Immunocompetent Adult or Child For the patient who presents with lymphadenopathy only, a positive IgM titer is an indication of acute infection-and an indication for therapy, if clinically warranted (see "Treatment," below). An elevation in the IgG titer without an increase in the IgM titer suggests that infection is present but is not acute. A therapeutic trial of anti-Toxoplasma medications is frequently used to assess the diagnosis. As in other conditions, the radiologic response may lag behind the clinical response. Antibody avidity increases with time and can be useful in difficult cases during pregnancy for establishing when infection may have occurred. Both assays are specific and sensitive, with fewer false-positive results than other commercial tests. Although a negative IgM result with a positive IgG titer indicates distant infection, IgM can persist for >1 year and should not necessarily be considered a reflection of acute disease. If acute toxoplasmosis is suspected, a more extensive panel of serologic tests can be performed. Congenital Infection the issue of concern when a pregnant woman has evidence of recent T. An increase in IgM beyond the first week of life is indicative of acute infection. Up to 25% of infected newborns may be seronegative and have normal routine physical examinations. Ocular Toxoplasmosis the serum antibody titer may not correlate with the presence of active lesions in the fundus, particularly in cases of congenital toxoplasmosis. If lesions are atypical and the serum antibody titer is in the low-positive range, the diagnosis is presumptive. Accordingly, the clinical diagnosis of ocular toxoplasmosis can be supported in 6090% of cases by laboratory tests, depending on the time of anterior chamber puncture and the panel of antibody analyses used. Prophylactic monotherapy with dapsone, pyrimethamine, azithromycin, clarithromycin, or aerosolized pentamidine is probably insufficient. If seroconversion has taken place, then the patient should be given prophylaxis as described above. Discontinuation of therapy reduces the pill burden; the potential for drug toxicity, drug interaction, or selection of drugresistant pathogens; and cost. Depending on the signs and symptoms, prednisone (1 mg/kg per day) may be used for congenital infection. Most experts use spiramycin to treat pregnant women who have acute toxoplasmosis early in pregnancy and use pyrimethamine/ sulfadiazine/folinic acid to treat women who seroconvert after 18 weeks of pregnancy or in cases of documented fetal infection. This treatment is somewhat controversial: clinical studies, which have included few untreated women, have not proven the efficacy of such therapy in preventing congenital toxoplasmosis. However, studies do suggest that treatment during pregnancy decreases the severity of infection. Many women who are infected in the first trimester elect termination of pregnancy. Those who do not terminate pregnancy are offered prenatal antibiotic therapy to reduce the frequency and severity of Toxoplasma infection in the infant. The optimal duration of treatment for a child with asymptomatic congenital toxoplasmosis is not clear, although most clinicians in the United States would treat the child for 1 year in light of cohort investigations conducted by the National Collaborative ChicagoBased, Congenital Toxoplasmosis Study. Patients with ocular toxoplasmosis are usually treated for 1 month with pyrimethamine plus either sulfadiazine or clindamycin and sometimes with prednisone. Treatment should be supervised by an ophthalmologist familiar with Toxoplasma disease. Ocular disease can be self-limited without treatment, but therapy is typically considered for lesions that are severe or close to the fovea or optic disc. Ingestion of raw shellfish is a risk factor for toxoplasmosis, given that the filter-feeding mechanism of clams and mussels concentrates oocysts. Litter boxes should be changed daily if possible, as freshly excreted oocysts will not have sporulated and will not be infectious.
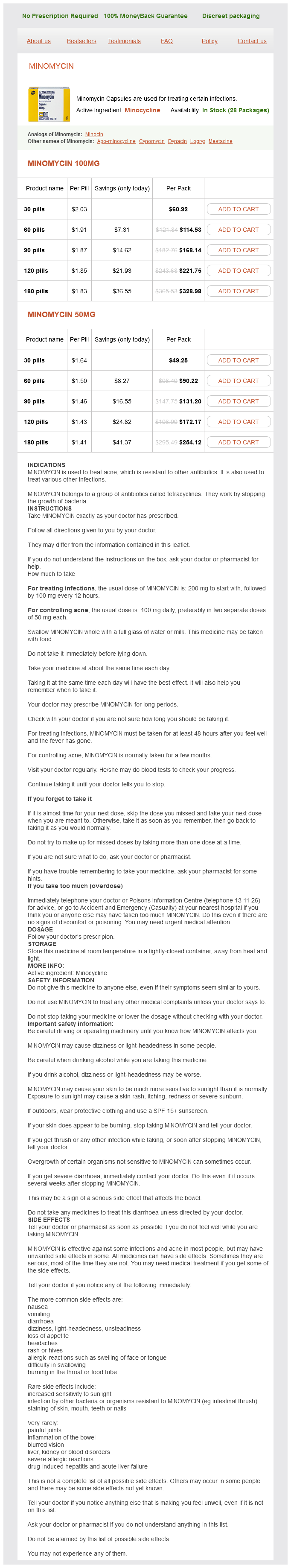
Minomycin Dosage and Price
Minomycin 100mg
- 30 pills - $60.92
- 60 pills - $114.53
- 90 pills - $168.14
- 120 pills - $221.75
- 180 pills - $328.98
Minomycin 50mg
- 30 pills - $49.25
- 60 pills - $90.22
- 90 pills - $131.20
- 120 pills - $172.17
- 180 pills - $254.12
This observation is consistent with an earlier report that the Fribourg-Blanc strain can cause experimental infection of humans antibiotics gut flora discount minomycin 100 mg with visa. Molecular analyses of additional samples from affected baboons suggests that the nonhuman primate samples diverge from the evolutionary tree prior to the clade that contains the human isolates, but uncertainty remains about the importance of the nonhuman primate reservoir for human infection. Primary and secondary stages are more frequently overlapping in yaws and endemic syphilis than in venereal syphilis, and the late manifestations of pinta are very mild relative to the destructive lesions of the other treponematoses. Because of the high degree of genetic relatedness among the organisms, there is little biological reason to think that T. The lack of recognized congenital infection may be due to the fact that childhood infections often reach the latent stage (low bacterial load) before girls reach sexual maturity. Yaws Also known as pian, framboesia, or bouba, yaws is characterized by the development of one or several primary lesions ("mother yaw") followed by multiple disseminated skin lesions. All early skin lesions are infectious and may persist for many months; cutaneous relapses are common during the first 5 years. Late manifestations, affecting ~10% of untreated persons, are destructive and can involve skin, bone, and joints. Regional lymphadenopathy develops, and the lesion usually heals within 6 months; dissemination is thought to occur during the early weeks of infection. Painful papillomatous lesions on the soles of the feet result in a crablike gait ("crab yaws"), and periostitis may result in nocturnal bone pain and polydactylitis. Late yaws is manifested by gummas of the skin and long bones, hyperkeratoses of the palms and soles, osteitis and periostitis, and hydrarthrosis. Destruction of the nose, maxilla, palate, and pharynx is termed gangosa and is similar to the destructive lesions seen in leprosy and leishmaniasis. Endemic Syphilis the early lesions of endemic syphilis (bejel, siti, dichuchwa, njovera, skerljevo) are localized primarily to mucocutaneous and mucosal surfaces. The infection is reportedly transmitted by direct contact, by kissing, by premastication of food, or by sharing of drinking and eating utensils. The initial lesion, usually an intraoral papule, often goes unrecognized and is followed by mucous patches. This eruption may last for months or even years, and treponemes can readily be demonstrated in early lesions. After a variable period of latency, late manifestations may appear, including osseous and cutaneous gummas. Destructive gummas, osteitis, and gangosa are more common in endemic syphilis than in yaws. Pinta Pinta (mal del pinto, carate, azul, purupuru) is the most benign of the treponemal infections. After one to many months of infection, numerous disseminated secondary lesions (pintides) appear. These lesions are initially red but become deeply pigmented, ultimately turning a dark slate blue. Although several targets have been evaluated for specific serodiagnosis, to date there is no antibody test that can discriminate among the different infections. The nonvenereal treponemal infections should be considered in the evaluation of a reactive syphilis serology in any person who has emigrated from an endemic area. Solely on the basis of experience with venereal syphilis, it is thought that doxycycline or tetracycline (at doses appropriate for syphilis; Chap. Enthusiasm is high; several planning meetings have been held to develop country-specific plans of action; and resources are being sought. Some caution is warranted: the possible animal reservoir will need to be evaluated. There may be only a window of time during which countries can successfully use azithromycin for yaws eradication before resistance begins to appear in yaws organisms. Given the ongoing lower-dose azithromycin mass treatment campaigns against trachoma, often in populations also at high risk for yaws, development of macrolide resistance is likely at some point. Complete drug coverage and continued careful surveillance by health centers (the weak link in prior control efforts) will be essential for success. Wagenaar Leptospirosis is a globally important zoonotic disease whose apparent reemergence is illustrated by recent outbreaks on virtually all continents. The disease is caused by pathogenic Leptospira species and is characterized by a broad spectrum of clinical manifestations, varying from asymptomatic infection to fulminant, fatal disease. In its mild form, leptospirosis may present as nonspecific symptoms such as fever, headache, and myalgia. With or without jaundice, severe pulmonary hemorrhage is increasingly recognized as an important presentation of severe disease. Twenty-two Leptospira species with pathogenic (10 species), intermediate (5 species), and nonpathogenic (7 species) status have now been described on the basis of phylogenetic and virulence 95 Leptospira kirschneri 40 48 Leptospira interrogans Leptospira kmetyi 59 Leptospira alstonii 54 Leptospira noguchii Leptospira borgpetersenii Leptospira borgpetersenii Leptospira weilii Leptospira alexanderi Leptospira santarosai 99 Leptospira licerasiae Leptospira wolffii 91 69 93 Leptospira fainei Leptospira broomii Leptospira inadai Leptospira idonii Leptospira vanthielii 100 Saprophytic Leptospira wolbachii 94 Leptospira biflexa 87 34 60 Leptospira terpstrae Leptospira meyeri 82 Leptospira yanagawae Leptonema illini 0. However, classification based on serologic differences better serves clinical, diagnostic, and epidemiologic purposes. Pathogenic Leptospira species are divided into serovars according to their antigenic composition. Leptospires are coiled, thin, highly motile organisms that have hooked ends and two periplasmic flagella, with polar extrusions from the cytoplasmic membrane that are responsible for motility. Leptospires require special media and conditions for growth; it may take weeks to months for cultures to become positive.