Molenzavir
General Information about Molenzavir
However, like several new drug, there are nonetheless some unanswered questions and further research wanted to fully perceive its effectiveness and security. Additionally, the provision and affordability of Molenzavir could additionally be a challenge in some nations, particularly in developing nations, which may hinder its widespread use.
In a section 2/3 medical trial, Molenzavir confirmed promising ends in decreasing the risk of hospitalization and dying in sufferers with mild to reasonable COVID-19. The trial included over 1,four hundred participants who had examined optimistic for COVID-19 within 5 days of the onset of symptoms. Among those who obtained Molenzavir, there was a 50% reduction in the danger of hospitalization or death compared to those who acquired a placebo.
Another vital benefit of Molenzavir is that it has shown efficacy towards totally different variants of the virus, together with the Delta variant, which is known to be more transmissible and causes more extreme illness. This makes it a flexible treatment choice that can be used globally, even in nations where different variants of the virus are prevalent.
The development of Molenzavir is a major breakthrough within the fight against COVID-19. It has the potential to fill a crucial gap in the current remedy choices for the disease, especially for patients with mild to average signs. Furthermore, it could be used as a prophylactic remedy to stop COVID-19 infections among high-risk individuals, such as healthcare staff.
In conclusion, Molenzavir has proven great promise as an oral antiviral therapy for COVID-19. It has the potential to improve patient outcomes and cut back the burden on healthcare systems by stopping hospitalizations. As we continue to battle the worldwide pandemic, Molenzavir presents hope for a more effective and handy treatment possibility that would assist deliver an finish to the COVID-19 crisis. However, it is essential to continue following public well being measures corresponding to sporting masks and getting vaccinated to stop the unfold of the virus.
Molenzavir works by concentrating on the RNA polymerase enzyme of the SARS-CoV-2 virus, which is answerable for replicating the virus. By inhibiting this enzyme, the drug interferes with the virus's ability to copy and spread within the body. This helps to reduce the severity of COVID-19 symptoms and shorten the length of the sickness.
The security profile of Molenzavir also seems to be favorable, with the most typical side effects being delicate and self-limiting, similar to headache, nausea, and diarrhea. This makes it an appropriate remedy choice for a variety of sufferers, including those with pre-existing situations.
Molenzavir, also referred to as Molnupiravir, is a promising new oral antiviral therapy for COVID-19. Developed by the pharmaceutical companies Merck and Ridgeback Biotherapeutics, this drug has shown promising leads to clinical trials and has the potential to be a game-changer within the struggle in opposition to the ongoing pandemic.
One of the principle advantages of Molenzavir is that it might be taken orally, making it much more convenient and accessible than other COVID-19 therapies that require hospitalization or intravenous administration. This signifies that it can be administered within the early levels of the disease, even earlier than the patient requires hospitalization. This is essential in controlling the unfold of the virus and preventing severe sickness and hospitalizations.
Reversible Cerebral Vasoconstriction Syndrome the major categories of diseases that can mimic vasculitis are displayed in Table 254-6 hiv infection inflammation immunosenescence and aging buy molenzavir 200mg with visa. First, most cases of vasculitis do not begin suddenly but rather unfold subacutely during weeks or months. Second, pain is usually a prominent feature of vasculitis, resulting from arthritis or arthralgias, myalgias, headaches, neuropathy, testicular infarction, digital ischemia, sinusitis, otalgia, back pain (caused by aortic inflammation), postprandial abdominal pain (caused by mesenteric vasculitis), or other disease manifestations. Third, signs of inflammation such as fever, rash, weight loss, and elevated acute phase reactants are highly characteristic. The diagnosis of vasculitis should be established through biopsy of an involved organ whenever possible. Angiographic findings that are "consistent with vasculitis" must be interpreted in the proper context. A diverse array of other diseases, ranging from atherosclerosis to vasospasm to pheochromocytoma, may mimic the angiographic appearance of vasculitis. Systemic vasculitis can also be mimicked by two or more common medical problems or treatment complications occurring simultaneously in the same patient. Finally, high on the differential diagnosis of any individual form of vasculitis are other forms of vasculitis. For example, digital ischemia and splinter hemorrhages may be secondary to idiopathic polyarteritis nodosa. Because the appropriate interventions for these conditions vary widely, careful distinction among these potential etiologies is essential. The intensity of treatment in patients with vasculitis must be guided by the degree of disease activity. Specifically, the treatment of vasculitis should be predicated not only on abnormal laboratory test results but also on clear evidence of active disease. In addition, the intensity of treatment must be adapted to the type of vasculitis. In contrast, despite the dramatic fashion in which they sometimes present, most cases of IgA vasculitis and cutaneous leukocytoclastic angiitis require no immunosuppressive treatment at all. Conventional therapies such as glucocorticoids, immunomodulating agents, and cytotoxic drugs induce remissions and control vasculitis in most cases. Moreover, in some cases-a variable percentage, depending on the type of vasculitis-the disease is curable. Prophylaxis against opportunistic infections, particularly Pneumocystis pneumonia (Chapter 321), is an important part of many vasculitis treatment regimens. During the tapering of immunosuppressive medications, disease flares are common in many forms of vasculitis. A common error is treating patients with high doses of immunosuppressive agents for too long. The most appropriate use of medications such as cyclophosphamide and glucocorticoids is to induce remission as quickly as possible with early, aggressive treatment regimens, and then to convert patients to safer treatments for the maintenance of remission. Assuming that the diagnosis is made before the patient has become catastrophically ill, the prognosis in systemic vasculitis is determined largely by the answers to four questions: 1. Was the diagnosis established before the occurrence of major irreversible organ damage Was there careful monitoring during treatment, and were specific steps taken to avoid drug-induced toxicity. Were the potentially toxic medications that induced remission stopped at an appropriate juncture and replaced with less dangerous medications (or was treatment stopped altogether) For most forms of vasculitis, the factors that determine long-term drug-free remissions remain poorly understood. The likelihood of achieving sustained remissions after discontinuation of all medications (or cures) varies according to the specific type of vasculitis. Important strides have been made in the description of cytokine and chemokine pathways that are operative in vascular inflammation, but relevant anticytokine interventions remain to be defined for clinical therapies. B-cell depletion is emerging rapidly as the treatment of choice for some forms of severe vasculitis. Additional studies are required to define the full spectrum of clinical utility of these and other biologic agents. Long-term outcomes and prognostic factors of complications in Takayasu arteritis: a multicenter study of 318 patients. Polyarteritis nodosa revisited: a review of historical approaches, subphenotypes and a research agenda. State-of-the-art acute phase management of Kawasaki disease after 2017 scientific statement from the American Heart Association. Pathogenetic and clinical aspects of anti-neutrophil cytoplasmic autoantibody-associated vasculitides. Pharmacokinetics of rituximab and clinical outcomes in patients with anti-neutrophil cytoplasmic antibody associated vasculitis. Improved survival with renal transplantation for end-stage renal disease due to granulomatosis with polyangiitis: data from the United States Renal Data System. Cogan syndrome: characteristics, outcome and treatment in a French nationwide retrospective study and literature review. This is negative for an intracranial bleed, and the headache resolves after approximately 24 hours, during which time it was profoundly disabling. Approximately 18 hours later, the headache returns, again rising to a crescendo within several minutes of onset. The headache improves following round-the-clock narcotic treatment but then worsens again on the third postpartum day. A magnetic resonance imaging study is negative for hemorrhage, cerebral infarctions, and masses, but a four-vessel cerebral angiogram shows alternating areas of vascular narrowing and dilation (beading) in multiple vascular distributions.
The use of cyclophosphamide in systemic sclerosis needs to be balanced against its potential for side effects symptoms of hiv infection mayo clinic molenzavir 200 mg cheap, including bone marrow suppression, opportunistic infections, hemorrhagic cystitis, bladder cancer, and premature ovarian failure. A2 In small clinical trials, methotrexate was associated with a modest improvement in skin involvement. Mycophenolate mofetil was shown to improve skin involvement and stabilize lung disease as well as cyclophosphamide, and it was well tolerated in a randomized controlled clinical trial. A3 There is some support in the literature for the use of immunomodulatory agents including, tocilizumab, intravenous immunoglobulin, and extracorporeal photopheresis for the treatment of systemic sclerosis. Recent reports suggest that rituximab might be effective in ameliorating skin and lung involvement. In patients with severe systemic sclerosis who fail to respond to other treatments (Chapter 168), autologous hematopoietic stem cell transplantation improves long-term, event-free survival despite an increased treatment-related mortality in the first year. A4 More recently, adults with severe systemic sclerosis were randomized to undergo myeloablative autologous hematopoietic stem cell transplantation (36 patients) or to receive cyclophosphamide immunosuppression by means of 12 monthly infusions (39 patients). The rate of event-free survival at 54 months was 79% in the transplantation group and 50% in the cyclophosphamide group (P = 0. Treatment-related mortality in the transplantation group was 3% at 54 months and 6% at 72 months, compared with 0% in the cyclophosphamide group. A5 Because of potential morbidity and mortality and its substantial cost, hematopoietic stem cell transplantation is presently considered only for carefully selected systemic sclerosis patients with aggressive or treatment-unresponsive disease. Because tissue fibrosis causes progressive and irreversible organ damage, drugs that block or slow the fibrotic process represent a rational approach to therapy. However, in a randomized controlled clinical trial, there was no difference in the extent of skin involvement between patients treated with standard-dose (750 mg/day) or very low-dose (125 mg every other day) D-penicillamine. Minocycline, bosentan, relaxin, interferon-, and inhibitors of tumor necrosis factor are putative antifibrotic agents that have failed to show meaningful benefit in systemic sclerosis clinical trials. Patients with severe Raynaud phenomenon require 1-adrenergic receptor blockers. Low-dose aspirin and dipyridamole prevent platelet activation and may have a role as adjunctive agents but must be used with caution in light of the risk of bleeding from gastric vascular ectasia lesions. The endothelin-1 receptor antagonist bosentan reduces development of new ischemic ulcers, A6 and sildenafil may promote ulcer healing. A7 Patients with ischemic digital ulcerations may require surgical débridement, especially if necrotic tissue is present. Empirical long-term therapy with statins and antioxidants may slow the progression of vascular damage. Pulmonary arterial Hypertension All patients with systemic sclerosis should be screened for pulmonary hypertension at initial evaluation, and those at high risk on a yearly basis. Treatment for symptomatic pulmonary hypertension should be started with an endothelin-1 receptor antagonist or a 5-phosphodiesterase inhibitor. Diuretics, oral anticoagulation, and digoxin, and supplemental oxygen, may be used when appropriate. If clinical response is inadequate, 5-phosphodiesterase inhibitors may be used in combination with endothelin-1 receptor antagonists. Prostacyclin analogs can be administered intravenously, by continuous subcutaneous infusion, or by frequent inhalations. Lung transplantation remains an option for selected patients with systemic sclerosisassociated pulmonary hypertension or interstitial lung disease who fail medical therapy. Because patients with early-stage systemic sclerosis and progressive skin involvement are at highest risk, they should be instructed to monitor their blood pressure daily and report significant alterations immediately. Corticosteroids should be used only when absolutely necessary and at the lowest possible doses. Although up to two thirds of patients who develop renal crisis require dialysis, delayed recovery of renal function can occur. Kidney transplantation is appropriate for patients unable to discontinue dialysis after 2 years. Survival with renal transplantation in systemic sclerosis is comparable to that in other connective tissue diseases, and recurrence of scleroderma renal crisis in the kidney graft is rare. Skin involvement in early systemic sclerosis is inflammatory and may respond to systemic antihistamines or short-term low-dose corticosteroids. Because of the increased risk for scleroderma renal crisis, blood pressure should be carefully monitored. Cyclophosphamide, methotrexate, D-penicillamine, and mycophenolate have been associated with modest improvement in skin induration in early-stage systemic sclerosis. Fingertip ulcerations should be protected by occlusive dressing to promote healing and prevent infection. Infected skin ulcers are treated with topical or oral antibiotics and may necessitate surgical débridement. No medical therapy has been shown to be effective in preventing soft tissue calcification or in promoting its dissolution, and surgical therapy and lithotripsy are only occasionally effective. Skin Care Treatment of Organ-Specific Complications Gastrointestinal complications Because significant gastroesophageal reflux may be asymptomatic, all patients with systemic sclerosis should be treated for this complication. Proton pump inhibitors may need to be given in relatively high doses and for prolonged periods, and patients should be instructed to elevate the head of the bed and eat frequent small meals. Recurrent gastrointestinal bleeding due to gastric vascular ectasia can be treated with laser or argon plasma photocoagulation. Bacterial overgrowth due to small bowel hypomotility causes bloating and diarrhea and may lead to malabsorption, weight loss, and malnutrition. Treatment with short courses of rotating broad-spectrum antibiotics such as metronidazole, erythromycin, and tetracycline can sometimes eradicate bacterial overgrowth.
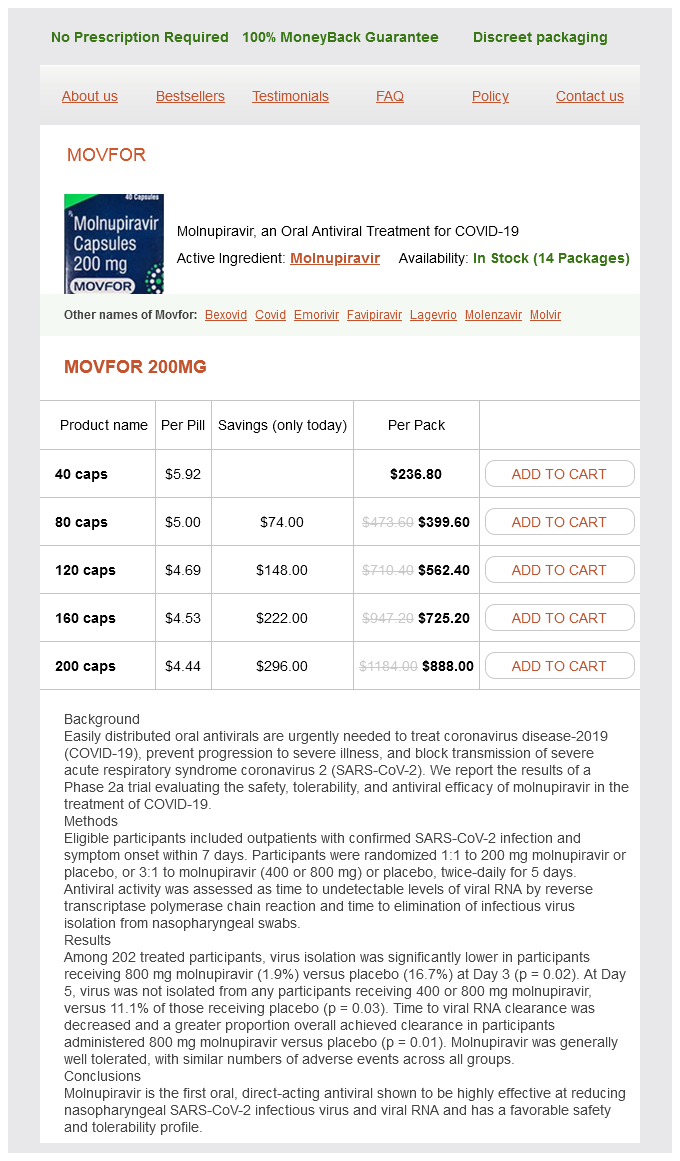
Molenzavir Dosage and Price
Movfor 200mg
- 40 caps - $236.80
- 80 caps - $399.60
- 120 caps - $562.40
- 160 caps - $725.20
- 200 caps - $888.00
Regarding renal outcome process of hiv infection and how it affects the body buy discount molenzavir 200 mg on line, an elevated level of serum creatinine at the time of diagnosis has been correlated with an adverse outcome. Recent studies of minority populations in the United States have indicated that predictors of high lupus disease activity include Hispanic Texan and African American ethnicities, lack of health insurance, and poor social support. Prognostic factors for an adverse fetal outcome in pregnant lupus mothers are maternal renal disease and hypertension. Safety of hormonal replacement therapy and oral contraceptives in systemic lupus erythematosus: a systematic review and meta-analysis. The 10-year follow-up data of the Euro-Lupus Nephritis Trial comparing low-dose and high-dose intravenous cyclophosphamide. Enteric-coated mycophenolate sodium versus azathioprine in patients with active systemic lupus erythematosus: a randomised clinical trial. Efficacy and safety of belimumab in patients with active systemic lupus erythematosus: a randomised, placebo-controlled, phase 3 trial. Anifrolumab, an anti-interferon- receptor monoclonal antibody, in moderate-to-severe systemic lupus erythematosus. Efficacy and safety of rituximab in patients with active proliferative lupus nephritis. The incidence and prevalence of systemic lupus erythematosus in San Francisco County, California: the California Lupus Surveillance Project. The incidence and prevalence of systemic lupus erythematosus in New York County (Manhattan), New York: the Manhattan Lupus Surveillance Program. Disease features and outcomes in United States lupus patients of Hispanic origin and their Mestizo counterparts in Latin America: a commentary. More than complementing Tolls: complement-Toll-like receptor synergy and crosstalk in innate immunity and inflammation. The study of interactions between genome and exposome in the development of systemic lupus erythematosus. Commensal orthologs of the human autoantigen Ro60 as triggers of autoimmunity in lupus. Endothelial progenitor cell phenotype and function are impaired in childhood-onset systemic lupus erythematosus. The pathogenesis and therapeutic implications of tubulointerstitial inflammation in human lupus nephritis. Revision of the International Society of Nephrology/ Renal Pathology Society classification for lupus nephritis: clarification of definitions, and modified National Institutes of Health activity and chronicity indices. Review: nervous system disease in systemic lupus erythematosus: current status and future directions. Progress in the pathogenesis and treatment of cardiac manifestations of neonatal lupus. Brief report: the Euro-Lupus low-dose intravenous cyclophosphamide regimen does not impact the ovarian reserve, as measured by serum levels of antiMüllerian hormone. Cyclophosphamide versus mycophenolate versus rituximab in lupus nephritis remission induction: a historical head-to-head comparative study. Sirolimus in patients with clinically active systemic lupus erythematosus resistant to , or intolerant of, conventional medications: a single-arm, open-label, phase 1/2 trial. Intravenous pulse glucocorticoid therapy and cyclophosphamide are appropriate for induction therapy but should not be used as a chronic maintenance therapy for lupus nephritis. Azathioprine is appropriate as a maintenance therapy but is inferior to other options as induction therapy. Rituximab has not shown efficacy in randomized controlled clinical trials for lupus nephritis but nonetheless is sometimes used in that clinical setting if other therapies are not successful. Adiponectin is a product of adipocytes and has not been described as having a role in lupus susceptibility. Hemolysis Answer: C Procainamide is an antihypertensive agent that has been associated with induction of lupus. Regulatory T cells contribute to protection from autoimmune disease rather than induction of autoimmune disease. Damage to podocytes might be one mechanism of renal damage but has not been associated with drug-induced lupus. Increased proteinuria and hemolysis are clinical manifestations of lupus but do not represent mechanisms that account for drug-induced lupus. All of the above Answer: E the clinical manifestations of lupus are protean and can affect any organ system. It should be noted that premature atherosclerotic cardiovascular disease is frequent among lupus patients and can contribute to increased mortality. The disease shows marked clinical heterogeneity, has protean clinical manifestations, and may follow a stable, indolent, or rapidly progressive course. In the earliest stages of the disease, evidence of inflammation, autoimmunity, and altered microvascular function are prominent. Over time, progressive and irreversible structural alterations in small blood vessels and fibrosis in multiple organs ensue. Nonetheless, current treatment strategies are frequently effective in controlling symptoms, slowing disease progression, improving quality of life, and prolonging survival. The presence of scleroderma (hard skin) distinguishes systemic sclerosis from other autoimmune and rheumatic diseases, but skin induration also features prominently in localized forms of scleroderma, as well as scleroderma-like conditions, paraneoplastic syndromes, and diverse unrelated disorders (Table 251-1). In patients with limited cutaneous systemic sclerosis, Raynaud phenomenon commonly precedes other disease manifestations, and skin involvement is indolent and limited. In contrast to limited cutaneous systemic sclerosis, diffuse cutaneous systemic sclerosis is generally rapidly progressive and may be complicated by early pulmonary fibrosis, accelerated hypertension, and acute renal failure. Raynaud phenomenon and other clinical and laboratory findings characteristic of systemic sclerosis in the absence of obvious skin thickening is the hallmark of systemic sclerosis sine scleroderma. Mixed Connective Tissue Disorder Classification Systemic Sclerosis A widely used classification for systemic sclerosis divides patients into two subsets: diffuse cutaneous systemic sclerosis and limited cutaneous systemic sclerosis.