Motrin
General Information about Motrin
In conclusion, Motrin is a extensively used medicine that gives aid from ache and irritation. However, like several medication, it ought to be used with caution and underneath the steering of a doctor. It can also be essential to follow the beneficial dosage and keep away from long-term use to prevent potential unwanted side effects. With its effectiveness in treating varied kinds of pain and inflammation, Motrin remains a preferred selection for many people seeking aid from discomfort.
One of the primary methods by which Motrin works is by inhibiting the manufacturing of prostaglandins, that are hormone-like substances concerned within the inflammatory response. By decreasing the levels of prostaglandins, Motrin can help cut back pain and irritation within the affected space. It additionally helps to decrease fever and has anticoagulant properties, making it an effective medicine for lowering the risk of blood clots.
It can be very important to understand that Motrin can interact with other medicines, corresponding to blood thinners, diuretics, and certain antidepressants. Therefore, it's essential to inform your physician about another medicines you are taking earlier than starting Motrin to keep away from potential drug interactions.
Motrin, also called ibuprofen, is a commonly used medicine for the therapy of pain and irritation. It belongs to a category of medication known as nonsteroidal anti-inflammatory drugs (NSAIDs) and is broadly obtainable in various varieties, corresponding to tablets, capsules, and liquid suspension. Motrin was first launched in the Sixties and has since become a go-to medicine for tens of millions of people worldwide.
Motrin is primarily used for the therapy of rheumatism and arthritis, which are chronic inflammatory conditions that affect the joints and cause ache, stiffness, and swelling. It is also generally used to alleviate widespread kinds of ache, similar to complications, menstrual cramps, toothaches, and backaches. It is an effective treatment for gentle to reasonable pain, making it a well-liked selection for people looking for reduction from varied sorts of discomfort.
The dosage of Motrin might vary depending on the purpose and severity of the condition being handled. For mild pain and fever, a lower dose is usually recommended, while greater doses could additionally be prescribed for extra severe conditions similar to arthritis. It is necessary to observe the prescribed dosage and not exceed the beneficial amount, as this could increase the chance of side effects.
Motrin is generally well-tolerated, however like any medicine, it can have some unwanted effects. The most common unwanted effects of Motrin include abdomen upset, heartburn, and nausea. In some circumstances, it might also cause dizziness, complications, and constipation. These unwanted aspect effects are often delicate and resolve on their own, but when they persist or turn out to be extreme, it is essential to consult a well being care provider.
However, in some uncommon instances, Motrin can also trigger extra extreme unwanted effects such as gastrointestinal bleeding, allergic reactions, and liver or kidney damage. Therefore, it is crucial to observe the recommended dosage and not take it for extended durations with out consulting a physician. Motrin should also not be taken by people who are allergic to aspirin or different NSAIDs, as this will result in severe allergic reactions.
The interface between the capillary and mitochondrial compartments is a diffusion barrier, the exact position of which is not known with certainty, although it may be dominated by the capillary endothelium cordova pain treatment center memphis motrin 600 mg buy low cost. The numbers refer to normal oxygen tensions in mm Hg units calculated from the equations for capillary and venous oxygen tensions and for mitochondrial oxygen tension. The oxygen tension of the average tissue compartment or capillary-mitochondrial diffusion interface is a simple linear average. Note that the term capillary bed is used for the entire portion of the vascular bed that interacts with the tissue. Longintudinal gradients in periarteriolar oxygen tension: a possible mechanism for the participation of of oxygen in local regulation of blood flow. These relationships apply only to the steady state in which there are no changes in substrate concentrations in the brain and glucose and oxygen do not enter other pathways. The formulation of lactate efflux applies to the tissue as a whole, under the assumption that pyruvate and lactate as monocarboxylic acids are not subject to compartmentation. Thus, the accumulation of lactate is a simple function of the pyruvate concentration and lactate efflux through the blood-brain barrier. Under nonsteady-state circumstances, the glucose, glycogen, pyruvate, and lactate concentrations change in complex ways (see later). Enzymes and transporters are among the proteins that subserve the nonequilibrium and near-equilibrium reactions that could contribute to these mechanisms. Near-equilibrium reactions buffer minute changes in the relevant substrates, but fluxgenerating and flux-directing nonequilibrium reactions adjust the magnitude and direction of metabolism dictated by extrinsic regulators. Generally speaking, these processes are glycolysis, or the breakdown of glucose to pyruvate, and oxidative phosphorylation, or the breakdown of pyruvate to carbon dioxide and the reduction of oxygen to water. The majority of the hexokinase protein in brain tissue appears to be coupled to a complex consisting of the voltage-dependent anion channel, the adenine nucleotide translocator, and the mitochondrial benzodiazepine receptor complex spanning the two mitochondrial membranes. As little as 15% is present in soluble form in the cytosol, although the distribution is variable and depends on numerous factors that are not well understood. The functional significance of the soluble and bound forms of the enzyme is also uncertain. Because glucose is normally the preferred substrate for brain metabolism, control of glycolysis is integral to understanding how increased energy production and utilization are linked. This regulation also explains the circumstances in which brain metabolism in general or metabolism in a separate cellular compartment such as neurons or glial cells has a preference for ketone bodies, lactate, or acetate when these substrates are present in excess (lactation, starvation, physical exertion, and possibly neuronal excitation). The time constants dictate the half-times of change, that is, the times that it takes the system to reach the halfway point of a new steady state. It is apparent from Table 7-6 that glycolysis responds to change with time constants on the order of milliseconds whereas oxidative metabolism responds with time constants of seconds or minutes. Hence, oxidative metabolism responds to any stimulus with a certain delay when compared with glycolysis. A most important step in glycolysis is the reaction catalyzed by the triose phosphate dehydrogenase step. In turn, this determines the direction and net flux of the reaction between pyruvate and lactate and the competition between glucose and lactate as sources of pyruvate when lactate is available in excess. LactateSynthesis Pyruvate directly participates in at least three primary reactions in brain tissue. Kinetic parameters and lactate dehydrogenase isozyme activities support possible lactate utilization by neurons. This subsection presents the primary regulatory steps for oxidative metabolism in mitochondria. In total, per mole of glucose, 20 hydrogen ion equivalents are extruded from the mitochondrial matrix and join four hydrogen ion equivalents generated in the cytosol. The ratio between the concentrations of lactate and pyruvate is also the apparent ratio between their affinities. At steady state, the ratio must be the same everywhere, given the near-equilibrium and facilitated diffusion nature of the proton symporters of lactate and pyruvate. Increases in calcium concentration often occur as repeated spikes with steep upslopes and shallower downslopes that reach baseline during sustained excitation. Extrusion of protons from the matrix establishes a gradient of hydrogen ion concentration across the inner membrane. When dissipated by escape of hydrogen ion back into the matrix through several different channels, this gradient drives specific molecular interactions that depend on its magnitude. Released into the matrix, hydrogen ions form water in a key interaction when they combine with oxide ions. There is a simple Michaelis-Mententype relationship between mitochondrial oxygen tension and the kinetic properties of cytochrome oxidase. The kinetics of this relationship shows that the rate of oxygen consumption depends critically on the average capillary oxygen tension and that it fails to rise above a certain threshold despite increases in cytochrome oxidase activity unless the affinity or diffusibility of oxygen is simultaneously adjusted. The threshold is dictated by the mitochondrial oxygen tension and is reached when the tension declines below the level associated with sufficient oxygen saturation of cytochrome oxidase. There is a theoretical limit to the efficacy of this adjustment, particularly when the cytosolic energy charge is unchanged. In reality, it appears that the near-equilibrium hypothesis assigns the ultimate maintenance of oxygen consumption to the regulation of oxygen delivery, particularly in situations in which mitochondrial oxygen tension threatens to fall below a minimum threshold. As a result of the imbalance between oxygen delivery and cytochrome oxidase activity in these states, cytochrome c oxidase does not remain saturated when the mitochondrial oxygen tension declines relative to the average capillary oxygen tension.
Muscle Pain Muscle Cramps Persistent muscle cramps in cancer patients are usually caused by an identifiable neural, muscular, or biochemical abnormality (Siegal 1991) neuropathic pain treatment guidelines iasp purchase discount motrin. In one series of 50 patients, 22 had peripheral neuropathy, 17 had root or plexus pathology (including 6 with leptomeningeal metastases), 2 had polymyositis, and 1 had hypomagnesemia. In this series, muscle cramps were the initial symptom of recognizable and previously unsuspected neurological dysfunction in 64% (27 of 42) of the identified causes (Steiner and Siegal 1989). Cramps have been reported as an adverse effect of imatinib (Breccia et al 2005), goserelin (Ernst et al 2004), and vincristine (Haim et al 1994). Skeletal Muscle Tumors Soft tissue sarcomas arising from fat, fibrous tissue, or skeletal muscle are the most common tumors involving the skeletal muscles. Skeletal muscle is one of the most unusual sites of metastasis from any malignancy (Cekinmez et al 2009). They occur disproportionally at sites of previous muscle trauma (Magee and Rosenthal 2002). Periosteitis and arthritis can produce pain, tenderness, and swelling in the knees, wrists, and ankles. The onset of symptoms is usually subacute, and it may precede discovery of the underlying neoplasm by several months. It is most commonly associated with nonsmall cell lung cancer with an incidence in this population of 15% (Ito et al 2010, Izumi et al 2010). Less commonly it may be associated with benign mesothelioma, pulmonary metastases from other sites, smooth muscle tumors of the esophagus, breast cancer, and metastatic nasopharyngeal cancer. Therapeutic approaches have recently been subjected Headache in cancer patients results from traction, inflammation, or infiltration of pain-sensitive structures in the head or neck. Early evaluation with appropriate imaging techniques may identify the lesion and allow prompt treatment, which may reduce pain and prevent the development of neurological deficits (Vecht et al 1992). Intracerebral Tumor the prevalence of headache in patients with brain metastases or primary brain tumors is 6090% (Kirby and Purdy 2007), and headache is frequently the first symptom of patients with brain tumors or metastases (Kirby and Purdy 2007) and is often associated with dizziness (Hird et al 2009). Among 183 patients with new-onset chronic headache as an isolated symptom, investigation revealed underlying tumor in 15 (Vazquez-Barquero et al 1994). The headache is presumably produced by traction on pain-sensitive vascular and dural 1050 Section Eight Clinical States/Cancer Pain enhancement of the basilar cisterns, parenchymal metastases, hydrocephalus without a mass lesion, or spinal subarachnoid masses or enhancement may all have therapeutic implications (Grossman and Krabak 1999). Ninety percent of patients ultimately show positive cytology, but multiple evaluations may be required. Tumor markers such as lactate dehydrogenase isoenzymes (Wasserstrom et al 1982), carcinoembryonic antigen (Liu et al 2009), 2-microglobulin (Twijnstra et al 1987), and tissue polypeptide antigen (Soletormos and Bach 2001) may help delineate the diagnosis. Untreated, leptomeningeal metastases cause progressive neurological dysfunction at multiple sites, followed by death in 46 weeks. Current treatment strategies, which include radiation therapy delivered to the area of symptomatic involvement, corticosteroids, and intraventricular or intrathecal chemotherapy or systemic chemotherapy, are of limited efficacy, and in general patient outlook remains poor (Clarke et al 2010). Base of Skull Metastases Base of skull metastases are associated with well-described clinical syndromes (Greenberg et al 1981, Laigle-Donadey et al 2005) that are named according to the site of metastatic involvement: orbital, parasellar, middle fossa, jugular foramen, occipital condyle, clivus, and sphenoid sinus. Cancers of the breast, lung, and prostate are most commonly associated with this complication (Greenberg et al 1981, LaigleDonadey et al 2005), but any tumor type that metastasizes to bone may be responsible. Orbital Syndrome Orbital metastases usually cause progressive pain in the retro- and supraorbital area of the affected eye (Ahmad and Esmaeli 2007). Signs may include proptosis, chemosis of the involved eye, external ophthalmoparesis, ipsilateral papilledema, and decreased sensation in the ophthalmic division of the trigeminal nerve. Parasellar Syndrome Parasellar syndrome is typically manifested as unilateral supraorbital and frontal headache, which may be associated tissue. Patients with multiple metastases and those with posterior fossa metastases are more likely to report this symptom (Kirby and Purdy 2007). Headache has lateralizing value, especially in patients with supratentorial lesions (Suwanwela et al 1994, Argyriou et al 2006b, Kirby and Purdy 2007). The quality of the headache is usually throbbing or steady, and the intensity is generally mild to moderate (Suwanwela et al 1994, Argyriou et al 2006b). In children headache is the most common initial symptom of brain tumors (Wilne et al 2006). The headache is frequently worse in the morning and is exacerbated by stooping, sudden head movement, or Valsalva maneuvers (cough, sneeze, or strain) (Suwanwela et al 1994). Leptomeningeal Metastases Leptomeningeal metastases, which are characterized by diffuse or multifocal involvement of the subarachnoid space by metastatic tumor, occur in 18% of patients with systemic cancer (Grossman and Krabak 1999, Taillibert et al 2005). Of solid tumors, adenocarcinomas of the breast and small cell lung cancer predominate (Bruno and Raizer 2005). Leptomeningeal metastases are associated with focal or multifocal neurological symptoms or signs that may involve any level of the neuraxis. The most common initial symptoms are headache, cranial nerve palsies (Yamanaka et al 2011), and radicular pain in the low back region and buttocks (van Oostenbrugge and Twijnstra 1999). More than one-third of patients have evidence of cranial nerve damage, including double vision, hearing loss, facial numbness, and decreased vision (Wasserstrom et al 1982, Yamanaka et al 2011). Less common features include seizures, papilledema, hemiparesis, ataxic gait, and confusion (Balm and Hammack 1996). Pain that resembles cluster headache (DeAngelis and Payne 1987) or glossopharyngeal neuralgia with syncope (Sozzi et al 1987) has also been reported. Ophthalmoparesis (Besada et al 2007) or papilledema may be present, and formal visual field testing may demonstrate hemianopia or quadrantanopia. Middle Cranial Fossa Syndrome Middle cranial fossa syndrome is characterized by facial numbness, paresthesias, or pain, which is usually referred to the cheek or jaw (in the distribution of the second or third divisions of the trigeminal nerve) (Lossos and Siegal 1992). The pain is typically described as a dull continual ache, but it may also be paroxysmal or lancinating. On examination, patients may exhibit hypoesthesia in the trigeminal nerve distribution and signs of weakness in the ipsilateral muscles of mastication.
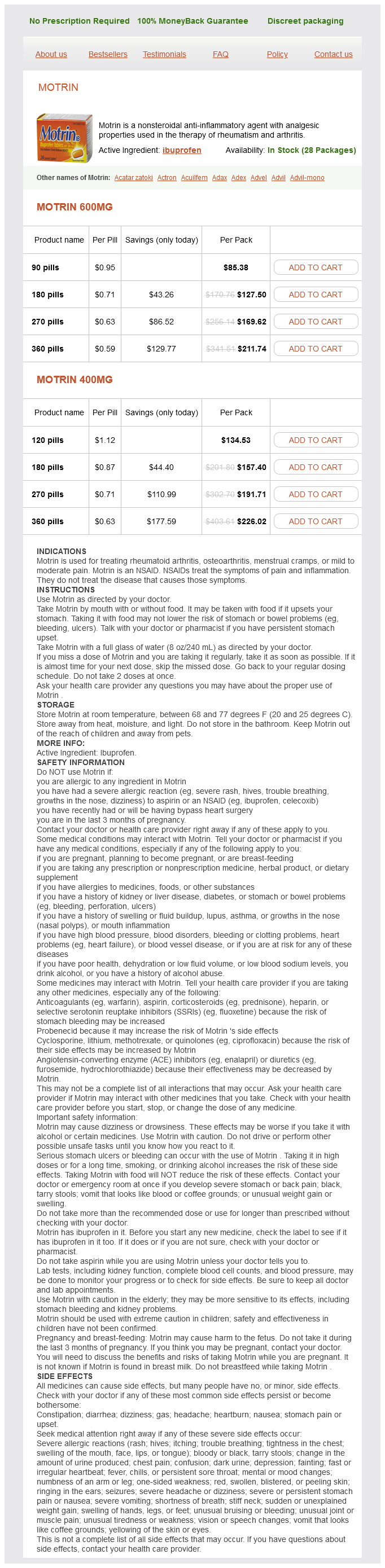
Motrin Dosage and Price
Motrin 600mg
- 90 pills - $85.38
- 180 pills - $127.50
- 270 pills - $169.62
- 360 pills - $211.74
Motrin 400mg
- 120 pills - $134.53
- 180 pills - $157.40
- 270 pills - $191.71
- 360 pills - $226.02
Great Vessels In addition to the specialized baro- and chemoreceptors of the aortic arch with afferent pathways in the vagus, the aorta contains afferent sympathetic nerve fibers that render it sensitive to dilatation and chemical stimulation of the adventitia (Uchida 1975, Wooley et al 1998) treatment guidelines for neuropathic pain buy discount motrin. The clinical correlate of these experimental observations is the pain experienced during balloon angioplasty performed for aortic coarctation (Erbel et al 1990). The afferent sympathetic nerve fibers conveying these sensations pass through the cardiac plexus to the sympathetic chain, primarily on the left side and, eventually travel to the upper thoracic segments of the spinal cord (Mizeres 1963). Mechanical, thermal, and chemical stimuli applied to the proximal pulmonary artery will activate sympathetic fibers of the cardiac plexus (Nishi et al 1977). However, vena cava stretch at the junction of the atria produces tachycardia through a vagally mediated afferent limb (Kaufman et al 1981). Although this demonstrates the presence of stretch receptors in portions of the vena cava, this particular observation may be more related to homeostasis than to nociception. Stretch receptors in the lung (Manning et al 1992) and muscle spindles of the chest wall (Edo et al 1998) signal the adequacy of inspiratory effort. The pathways by which the foregoing signals ascend and are integrated to generate the sensation of dyspnea are not well understood (Burki and Lee 2010, Nishino 2011). However, as with many other unpleasant sensations, functional imaging reveals activation of the anterior cingulate cortex and insular cortex when dyspnea is experienced (Herigstad et al 2011). Hiccups are another unpleasant symptom that originate in the thorax and can be triggered by afferent input from the phrenic or vagus nerve, particularly with stimulation at the diaphragm, mediastinum, or distal portion of the esophagus, as well as by central mechanisms (Marinella 2009). Apart from the discomfort that they produce, hiccups may be significant because mechanical or chemical stimuli that would otherwise be perceived as pain at other locations are instead manifested as hiccups through irritation of afferent components of the aforementioned nerves. Moreover, stimuli usually noxious in character may not produce pain but could be manifested as alterations in respiratory or cardiovascular behavior. In other instances, pain will also be accompanied by changes in essential physiological processes. Cough, dyspnea, and hiccups are symptoms of thoracic origin that may herald the presence of thoracic pathology and can be sufficiently unpleasant, particularly when chronic, to become the primary motivation for medical consultation. An overwhelming array of oncological, vascular, inflammatory, infectious, traumatic, congenital, idiopathic, and iatrogenic disorders, not necessarily of thoracic location, can produce thoracic pain or other unpleasant sensations of thoracic origin (Box 52-1). The differential diagnosis and treatment of these many conditions are similarly overwhelming and will not be attempted here. Instead, this list provides opportunities to achieve a more refined appreciation of the initiation of thoracic pain in its various forms, particularly those that will come to the attention of pain specialists. Additional interpretation will be provided by the context of age, genetic and psychological factors, co-existing disease, and other painful conditions. Esophagus Like the heart and pericardium, the esophagus is innervated by both vagal and sympathetic afferents. Sympathetic fibers supplying the upper portion of the esophagus travel with those innervating the heart and pericardium. Both vagal and sympathetic afferents are sensitive to mechanical and chemical stimuli, although the sympathetic system is thought to encode the majority of noxious input. The sympathetic afferents enter the spinal cord in the region of C26, T24, and T812; synapse with fibers of the spinothalamic tract and posterior columns; and project to the thalamus, sensory cortex, prefrontal cortex, insula, and anterior cingulate cortex (Hobson and Aziz 2004). Pain can be generated by acid exposure, distention, and sustained muscle contraction (Drewes et al 2006, Gregersen et al 2007, Holzer 2011). Overview of Thoracic Pain the prevalence and spectrum of thoracic pain depend very much on the patient population and setting, with considerable differences among the emergency department, outpatient clinic, and chronic pain clinic. In the adult emergency department, 5% of patients have a chief complaint of chest pain (McCaig and Nawar 2006), whereas no more than 1% do so in the outpatient setting (Slusarcick and McCaig 2000, Middleton et al 2007). The cause of the pain varies considerably with the setting (Table 52-1), with life-threatening conditions being diagnosed more frequently in the emergency department (Buntinx et al 2001). The cause of this pain is distributed somewhat differently from that in adults (Table 52-2) (Selbst et al 1988), and even in those evaluated in the cardiology clinic, a diagnosis of cardiac disease is assigned to only 7% (Massin et al 2004). Formal (Cohen et al 2005) and informal (van Kleef et al 1995, Lou and Gauci 2002) estimates of the prevalence of thoracic pain in those seen in a pain clinic are about 5%, although such estimates may be a function of the population served and the focus of the clinic. The majority of these patients receive diagnoses related to the spine (Bonica and Sola 1990, van Kleef et al 1995). Regardless of where a patient is evaluated, the initial focus should be on avoiding misdiagnosis of an acute life-threatening disease, including coronary artery disease in its various forms Breast and Chest Wall Cutaneous innervation of the breast is provided by the anterior (T16) and medial (T27) branches of the intercostal nerves. Supply to the nippleareola complex is derived primarily from the anterior and medial branches of the fourth intercostal nerve with varying contributions from the third and fifth intercostal nerves (Jaspars et al 1997). Innervation of the chest wall is provided by the intercostal nerves of the corresponding dermatome with supplementation by the nerves above and below. Some additional input is provided to the two upper thoracic dermatomes by the third and fourth cervical nerve roots. In addition, sensation to portions of the upper extremities is supplied by the first two thoracic nerves (Gray 1989b). Its upper branch provides sensation to the breast and anterior aspect of the chest, and its two lower branches supply sensation to the axilla and arm. Mosby-Elsevier, Philadelphia, p 317324; and Thull-Freedman J 2010 Evaluation of chest pain in the pediatric patient. No organic etiology and without psychological factors present to explain the pain. From Buntinx F, Knockaert D, Bruyninckx R, et al 2001 Chest pain in general practice or in the hospital emergency department: is it the same Family Practice 18:586589 from stable to unstable angina, myocardial infarction, pulmonary embolism, aortic dissection, esophageal rupture, pneumonia, and pericarditis (Cayley 2005, Winters and Katzen 2006, Yelland et al 2010). Modern imaging technology is making it possible to simultaneously examine the coronary and pulmonary arteries, as well as the thoracic aorta, to perform a "triple rule-out" of coronary artery disease, pulmonary embolism, and aortic dissection, in addition to obtaining other relevant diagnostic information (Frauenfelder et al 2009).