Naltrexone
General Information about Naltrexone
Naltrexone is a medicine that has been hailed as a revolutionary remedy for those fighting narcotic drug or alcohol addiction. Developed within the Sixties and accredited by the Food and Drug Administration (FDA) in 1984, naltrexone has proven to be a game changer in the field of habit remedy.
Naltrexone is an opioid antagonist, that means it blocks the consequences of opioid medication corresponding to heroin, morphine, and oxycodone. It works by attaching to and blocking the opioid receptors within the brain, stopping the opioids from producing their desired results. This helps to reduce back cravings and forestall the particular person from experiencing the euphoric results of opioids.
In conclusion, naltrexone has been a groundbreaking treatment in the remedy of alcohol and opioid habit. Its capacity to dam the effects of opioids and scale back cravings has been instrumental in helping people overcome their habit. While it will not be the proper therapy possibility for everyone, it has confirmed to be a priceless tool in the struggle in opposition to habit. If you or a loved one is battling addiction, speak to a healthcare skilled about whether or not naltrexone could additionally be an appropriate treatment possibility. Recovery is feasible, and naltrexone can play an essential role in achieving and sustaining a sober life.
Naltrexone is primarily used to deal with alcohol and opioid dependence. When used for alcohol dependence, it really works by decreasing the euphoric effects of alcohol, making it much less interesting to people struggling with habit. It additionally helps to decrease the severity of alcohol cravings, making it simpler for individuals to withstand the temptation to drink.
When used for opioid dependence, naltrexone is usually used after an individual has undergone detoxing and is within the early stages of recovery. It helps to prevent relapse by blocking the results of opioids if the person had been to make use of them once more. This allows people to focus on their recovery without the fixed distraction of cravings and withdrawal signs.
Naltrexone is best when used as part of a complete treatment plan that includes therapy, assist groups, and lifestyle adjustments. It just isn't a treatment for dependancy however rather a device to help people of their recovery journey. With the best support and treatment, naltrexone could be a key consider helping individuals keep sober and keep their sobriety long-term.
One of the main benefits of naltrexone is that it's non-addictive, making it a secure option for individuals in restoration. It also has a protracted half-life, meaning it stays within the physique for a longer time period, making it more practical in stopping relapse. It can be administered in a quantity of varieties, including a tablet, a monthly injection, or an implant that lasts for a number of months.
However, like all treatment, naltrexone does include potential unwanted effects. These could embody nausea, headache, dizziness, fatigue, and insomnia. Some people may experience more critical unwanted effects similar to liver damage, so it's important for individuals taking naltrexone to frequently see their doctor for check-ups and blood tests to observe their liver perform.
Another example of patchy disease distribution occurs in cases of fulminant hepatic failure associated with submassive hepatic necrosis symptoms meaning order naltrexone canada. Both images from a single block of liver obtained at transplantation from a patient with primary biliary cirrhosis/cholangitis. B, In adjacent area, there is preservation of normal vascular relationships with no evidence of fibrosis. The main indications for a pretransplant frozen section are to determine the nature of unexplained focal liver areas of nodular regeneration in which there is often pronounced cholestasis. A liver biopsy taken from an area of panacinar necrosis may overestimate the severity of disease present in the liver as a whole, whereas a biopsy taken from a cholestatic regeneration nodule may provide no clues to either the nature or the severity of liver injury present. For some liver diseases the removal of the whole liver allows the study of larger biliary or vascular structures, which would not normally be sampled in needle biopsy specimens. The vacuoles in microvesicular steatosis are smaller than the nucleus, and the nucleus remains central. Steatosis is graded as mild (530%), moderate (3060%) or severe (>60%), according to the estimated percentage of liver parenchyma affected. Because macroscopic appearances may not be reliable in assessing the severity of steatosis, a frozen section of the donor liver is often obtained in cases where fatty change is suspected clinically. The use of specific fat stains such as Oil Red O generally increases the amount of fat visualized, but these methods are prone to considerable technical variation. There is often a discrepancy between the severity of steatosis determined on frozen section and that seen in subsequent paraffin histology, but this discrepancy appears to have little clinical impact. Donor grafts with up to 30% macrovesicular steatosis can be safely used68,77 and represent 97% of all steatotic grafts transplanted in the United States. Hepatocytes distended with large fat droplets can obstruct the sinusoidal microvasculature, resulting in problems with perfusion of the donor liver at retrieval and subsequent reperfusion in the recipient. However, electron microscopic analysis has shown that the free lipid is extrasinusoidal, with only more severe cases resulting in rupture into the sinusoidal space. Although microvesicular steatosis is well recognized as a rare cause of liver failure in the nontransplanted liver. Reye syndrome), its presence in donor livers, even to a marked degree, is not generally associated with poor graft function. Although donors are generally in good health, the diagnostic pretransplant workup aims to detect occult hepatic or extrahepatic disease. Most centres do not routinely biopsy all potential donors, but guidelines on when to biopsy are lacking. In studies where biopsies have been obtained from potential living donors (some routinely, others after progressing beyond initial screening process), <50% are normal. About 1530% have either moderate or severe steatosis, and 115% have steatohepatitis. As with cadaveric liver grafts, mild degrees of steatosis are tolerated, but donors are excluded if macrovesicular steatosis is >25%104 or 33%,103,107 because of the risk to both donor and recipient of compromised regeneration. These include episodes of hypotension (leading to ischaemic graft injury), poor nutritional state (resulting in depletion of hepatic glycogen stores) and endotoxaemia, possibly related to mucosal injury of the gut. The initial source is from Kupffer cells, which are activated within 15 min of reperfusion, with subsequent amplification from neutrophils as they are recruited. Centrilobular fat microcysts are surrounded by macrophages in this biopsy specimen taken 10 days following insertion of a steatotic donor liver. Subsequent biopsy specimens have shown resorption of the fat with only minimal residual perisinusoidal fibrosis. Particularly over 60 years of age, these have an increased risk of graft loss that is most evident after transplantation for hepatitis C,111 but there is also an increased risk of primary nonfunction, hepatic artery thrombosis, preservation/reperfusion injury and biliary complications. A recent study found that time zero biopsy grading could be performed reproducibly, after 4560 min of reperfusion. Moderate injury showed clustered neutrophils and some hepatocyte necrosis or apoptosis, and severe injury had zonal (usually centrilobular) hepatocyte necrosis, neutrophilic infiltrates in these areas and clustered neutrophils in more distant sinusoids. This liver biopsy specimen, obtained 7 days after transplantation, shows severe cholestasis and ballooning affecting centrilobular and midzonal hepatocytes. These changes are frequently seen in the absence of rejection and can be ascribed to preservation/reperfusion injury. If ballooning persists beyond the first 2 weeks after transplant, other possible causes should be considered, particularly when associated with centrilobular necrosis. Although fatty change is mainly considered to be a pre-existing donor lesion, some evidence suggests that graft ischaemia and reperfusion injury may lead to the development of steatosis in the early post-transplant period79 and may be microvesicular in type. These terms should not be used to describe patients with other peri- or postoperative factors, such as vascular occlusion or antibody-mediated rejection, which can also result in graft dysfunction or failure in the immediate post-transplant period. There are problems with establishing precise diagnostic criteria for these three syndromes, accounting for the wide variation intheirreportedfrequency. It has been suggested that time zero biopsies may be of prognostic value in predicting subsequent poor graft function when certain changes (apart from significant steatosis as already discussed) are present. Recent studies suggest that the use of alternative methods such as metabolomics and genomic profiling to analyse pre- and postimplantation donor liver biopsies may also be helpful in predicting early allograft dysfunction. A cadaveric graft can be split to provide two grafts, often to a paediatric and an adult recipient. Reduced-size grafts aim to provide a graft with at least 3040% of the expected liver volume or a graft/recipient weight ratio of >0.
Infantile periarteritis nodosa or mucocutaneous lymph node syndrome: a report on four cases and diagnostic considerations treatment junctional rhythm cheap naltrexone 50 mg amex. Coronary aneurysms in infants and young children with acute febrile mucocutaneous lymph node syndrome. Variant strain of Propionibacterium acnes: a clue to the aetiology of Kawasaki disease. A genome-wide association study identifies three new risk loci for Kawasaki disease. A familial syndrome of short stature associated with facial dysplasia and genital anomalies. Syndrome of extreme insulin resistance (Rabson-Mendenhall phenotype) with atrial septal defect: clinical presentation and treatment outcomes. Chediak-Higashi syndrome: cytologic and serum lipid observations in a case and family. Albinism associated with hemorrhagic diathesis and unusual pigmented reticular cells in the bone marrow: report of two cases with histochemical studies. Heterogeneity in storage pool deficiency: studies on granule-bound substances in 18 patients including variants deficient in alpha-granules, platelet factor 4, beta-thromboglobulin, and platelet-derived growth factor. Linkage disequilibrium mapping of the gene for Hermansky-Pudlak syndrome to chromosome 10q23. An autopsy case of Hermansky-Pudlak syndrome: a case report and review of the literature on treatment. Liver agenesis with omphalocele: a report of two human embryos using serial histological sections. Hypogenesis of right hepatic lobe accompanied by portal hypertension: case report and review of 31 Japanese cases. Biliary injury after laparoscopic cholecystectomy in a patient with right liver agenesis: case report and review of the literature. Hypoplastic right hepatic lobe with retrohepatic gallbladder complicated by hepatolithiasis and liver abscess: a case report. Hepatic pulmonary fusion: two cases with diaphragmatic hernia and one case with pentalogy of Cantrell. Partial eventration of the right diaphragm (congenital diaphragmatic herniation of the liver). Focal nodular hyperplasia on accessory lobe of the liver: preoperative diagnosis and management. Infantile hemangioendothelioma of heterotopic intrathoracic liver associated with diaphragmatic hernia. Heterotopic supradiaphragmatic liver formation in association with congenital cardiac anomalies. Propensity of ectopic liver to hepatocarcinogenesis: case reports and a review of the literature. Hypoglycemia from metastasizing insular carcinoma of aberrant pancreatic tissue in liver. Pathologic observations of intrahepatic peribiliary glands in 1000 consecutive autopsy livers. Intrahepatic splenic tissue without medical history of splenic injury or splenectomy. Radiological anatomy of the biliary tract: variations and congenital abnormalities. Atresia of the common hepatic duct with shunt via an accessory duct: report of a case. Anomalous insertion of the right hepatic duct into the cystic duct: report of a case diagnosed before laparoscopic cholecystectomy. Hepatolithiasis associated with anomalous biliary anatomy and a vascular compression. A new systematic classification of peripheral anatomy of the right hepatic duct: experience from adult live liver donor transplantation. Biliary cystadenoma and cystadenocarcinoma: report of 14 cases and review of the literature. Long accessory hepatic duct associated with congenital dilation of the common bile duct. Congenital bronchobiliary fistula associated with esophageal atresia and tracheo-esophageal fistula. Ciliated hepatic foregut cyst: a report of 6 cases and a review of the English literature. Ciliated hepatic foregut cyst: a mucus histochemical, immunohistochemical, and ultrastructural study in three cases in comparison with normal bronchi and intrahepatic bile ducts. The ciliated hepatic foregut cyst, an unusual bronchiolar foregut malformation: a histological, histochemical, and immunohistochemical study of 7 cases. Spontaneous perforation of the bile duct in infancy and childhood: a systematic review. Complex spontaneous bile duct perforation: an alternative approach to standard porta hepatis drainage therapy. Therefore since humans have not developed active mechanisms to dispose of excess iron, blood and tissue iron levels must be kept within a very narrow range through fine-tuned regulatory systemic and local mechanisms. Moreover, a number of plasma and tissue proteins have evolved to absorb, transport and store highly reactive iron (see next section). Based on these premises, it is no surprise that both iron deficiency and iron overload may represent serious threats to human health. A variety of abnormal states may arise from the disruption of iron homeostasis, ranging from iron deficiency anaemia to genetic iron overload, as typified by hereditary haemochromatosis. In recent years, there have been dramatic advances in understanding the handling of iron in the body and its homeostatic regulation.
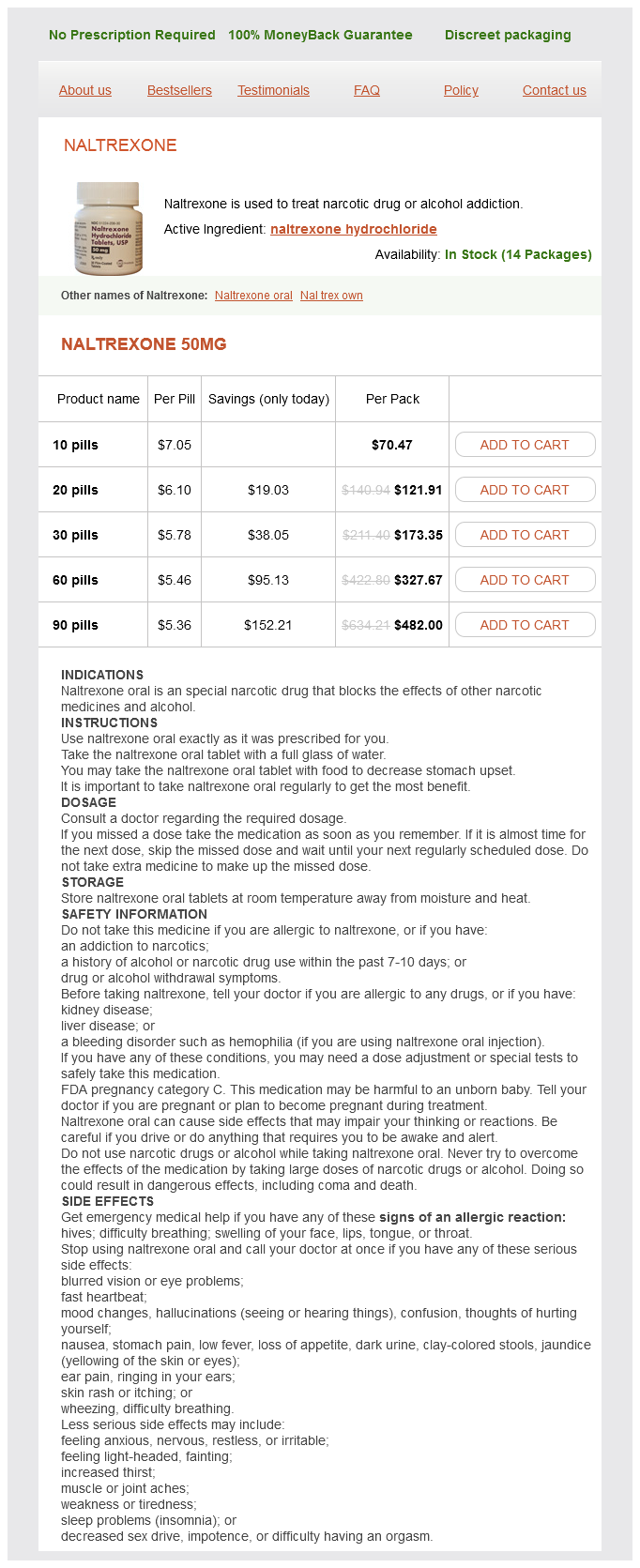
Naltrexone Dosage and Price
Naltrexone 50mg
- 10 pills - $70.47
- 20 pills - $121.91
- 30 pills - $173.35
- 60 pills - $327.67
- 90 pills - $482.00
In the wavelengths typically used for light microscopy treatment management company discount 50 mg naltrexone overnight delivery, light scattering attenuates light propagation in deep sections. An established approach for imaging deeply into tissue involves fluorescent nonlinear optical processes such as two-photon fluorescence excitation. This high-energy level excites fluorophores that emit a 104 Chapter 2 Cellular and Molecular Techniques single photon in the visible spectrum. Native fluorescent signatures present in tissues from normal physiology and pathophysiological processes can be recovered with high-quality imaging. Indeed, because it maintains cells and tissues in a healthy functional state under the microscope in the presence of synthetic fluorophores and fluorescent proteins, nonlinear microscopy is becoming the technique of choice for imaging live liver cells and tissues in cell biology research laboratories. Percutaneous biopsy in diffuse liver disease: increasing diagnostic yield and decreasing complication rate by routine ultrasound assessment of puncture site. Complications following percutaneous liver biopsy: a multicentre retrospective study on 68,276 biopsies. Indications, methods, and outcomes of percutaneous liver biopsy in England and Wales: an audit by the British Society of Gastroenterology and the Royal College of Physicians of London. The practice of percutaneous liver biopsy in a gastrohepatology day hospital: a retrospective study on 835 biopsies. Effect of needle gauge, level of anticoagulation, and target organ on bleeding associated with aspiration biopsy. Transvenous liver biopsy: an experience based on 1000 hepatic tissue samplings with this procedure. Transjugular liver biopsy: indications, adequacy, quality of specimens, and complications-a systematic review. Transjugular liver biopsy: how good is it for accurate histological interpretation Safety and feasibility of a new minimally invasive diagnostic laparoscopy technique. Biopsy diagnosis of cirrhosis: blind percutaneous versus guided direct vision techniques-a review. Fine-needle aspiration cytology guided by endoscopic ultrasonography: results in 141 patients. Value of rapid staining and assessment of ultrasound-guided fine needle aspiration biopsies. Fine needle aspiration biopsy of the liver: algorithmic approach and current issues in the diagnosis of hepatocellular carcinoma. The diagnostic value of on-site cytopathological evaluation and cell block preparation in fine-needle aspiration cytology of liver masses. Ultrasound-guided fine-needle biopsy of focal liver lesions: techniques, diagnostic accuracy and complications. Ultrasonically guided fineneedle aspiration biopsy: a highly diagnostic procedure for hepatic tumors. Fine needle aspiration biopsy for improving the diagnostic accuracy of cut needle biopsy of focal liver lesions. Neoplastic seeding complicating percutaneous ethanol injection for treatment of hepatocellular carcinoma. Needle-tract implantation from hepatocellular cancer: is needle biopsy of the liver always necessary Lack of tumor seeding of hepatocellular carcinoma after percutaneous needle biopsy using coaxial cutting needle technique. Impact of preoperative fine-needle aspiration cytologic examination on clinical outcome in patients with hepatocellular carcinoma in a tertiary referral center. Indication and contraindication for hepatic resection for liver tumors without fine-needle biopsy: validation and extension of an Eastern approach in a Western community hospital. Observer error and sampling variability tested in evaluation of hepatitis and cirrhosis by liver biopsy. Sampling variability and its influence on the diagnostic yield of percutaneous needle biopsy of the liver. Percutaneous needle biopsy specimens: sampling variability in patients with chronic hepatitis and cirrhosis. Impact of liver biopsy size on histological evaluation of chronic viral hepatitis: the smaller the sample, the milder the disease. Interobserver study of liver histopathology using the Ishak score in patients with chronic hepatitis C virus infection. Diagnosing fibrosis in hepatitis C: is the pendulum swinging from biopsy to blood tests Role of gamma-glutamyl transpeptidase activity in the diagnosis of hepatobiliary disease. The ratio of aspartate aminotransferase to alanine aminotransferase: potential value in differentiating nonalcoholic steatohepatitis from alcoholic liver disease. Biochemical markers of liver fibrosis in patients with hepatitis C virus infection: a prospective study. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Serum proteome to predict virologic response in patients with hepatitis C treated by pegylated interferon plus ribavirin.