Nexium
General Information about Nexium
In conclusion, Nexium has been confirmed to be an effective medicine for the treatment of extreme abdomen acid and related circumstances. With its capability to decrease acid manufacturing and promote healing, it has provided relief to millions of individuals affected by GERD, ulcers, and other associated conditions. However, you will need to use Nexium as directed and to seek the advice of with a healthcare skilled if any regarding side effects occur.
The main function of Nexium is to deal with symptoms of gastroesophageal reflux disease (GERD), a continual disorder the place stomach acid flows again into the esophagus, causing a burning sensation within the chest (heartburn). This is a quite common situation, with about 20% of individuals experiencing it no much less than once a week.
Nexium is available in both over-the-counter (OTC) and prescription types. The OTC model is usually used for short-term remedy of heartburn and acid reflux. It is meant to be taken for as much as 14 days and shouldn't be used as a long-term solution. The prescription version, then again, can be used for long-term upkeep remedy for situations corresponding to GERD and Zollinger-Ellison syndrome.
Aside from H. pylori, another cause of gastric ulcers is using nonsteroidal anti-inflammatory drugs (NSAIDs) corresponding to aspirin, ibuprofen, and naproxen. These drugs can irritate the lining of the stomach, resulting in the development of ulcers. Nexium may be given to patients who need long-term use of NSAIDs to stop the development of ulcers.
Like any medication, Nexium does include potential unwanted effects. The most common ones include headache, diarrhea, nausea, and stomach pain. Rare but severe unwanted aspect effects embody allergic reactions and low magnesium ranges. Patients with pre-existing situations corresponding to kidney disease or osteoporosis should consult with their physician earlier than starting to use Nexium.
Another widespread use of Nexium is to advertise healing of erosive esophagitis. This is a condition the place the liner of the esophagus is broken by abdomen acid, causing irritation and irritation. It can result in issue swallowing and even scarring if left untreated for an extended time. Nexium helps to scale back the acidity of the stomach, allowing the esophagus to heal.
Nexium has additionally been approved for prevention of gastric ulcers attributable to infection with helicobacter pylori (H. pylori). This bacteria is a typical reason for stomach ulcers and can be handled with antibiotics. When used in mixture with sure antibiotics, Nexium helps to scale back the quantity of stomach acid, making a extra favorable surroundings for therapeutic.
Nexium is a medicine that has turn into a household name for these who suffer from excessive abdomen acid. It is a brand name for the generic drug esomeprazole, which is a proton pump inhibitor (PPI). PPIs are commonly used to lower the quantity of acid produced within the abdomen.
In addition to GERD, Nexium can be used to deal with other conditions involving extreme stomach acid, such as Zollinger-Ellison syndrome. This is a rare condition where the abdomen produces an excessive amount of acid, resulting in severe ulcers in the digestive system. Left untreated, it could trigger severe complications similar to bleeding and perforation of the stomach or intestines.
Flakes of fibrin appear and cause loops of intestine to become adherent to each other and to the parietes gastritis symptoms shortness breath generic nexium 20 mg free shipping. There is an outpouring of serous inflammatory exudate rich in leukocytes and plasma proteins that soon becomes turbid; if localisation occurs, the turbid fluid becomes frank pus. Peristalsis is retarded in affected bowel and this helps to prevent distribution of the infection. The greater omentum, by enveloping and becoming adherent to inflamed structures, often forms a substantial barrier to the spread of infection (see below). These organisms lead to a thinning of cervical mucus and allow bacteria from the vagina into the uterus and oviducts, causing infection and inflammation. Klebsiella pneumoniae Other sources Chlamydia trachomatis Neisseria gonorrhoeae Haemolytic streptococci Staphylococci Streptococcus pneumoniae Mycobacterium tuberculosis and other species Fungal infections Speed of peritoneal contamination is a prime factor. If an inflamed appendix or other hollow viscus perforates before localisation has taken place, there will be an efflux of contents into the peritoneal cavity, which may spread over a large area almost instantaneously. Perforation proximal to an obstruction or from sudden anastomotic separation is associated with severe generalised peritonitis and a high mortality rate. Stimulation of peristalsis by the ingestion of food or even water hinders localisation. Violent peristalsis occasioned by the administration of a purgative or an enema may cause the widespread distribution of an infection that would otherwise have remained localised. The virulence of the infecting organism may be so great as to render the localisation of infection difficult or impossible. Named after the two physicians, Thomas Fitz-Hugh, Jr and Arthur Hale Curtis who first reported this condition in 1934 and 1930, respectively. With appropriate treatment, localised peritonitis usually resolves; in about 20% of cases, an abscess follows. Conversely, in favourable circumstances, diffuse peritonitis can become localised, most frequently in the pelvis or at multiple sites within the abdominal cavity. When the peritoneum becomes inflamed, abdominal pain will worsen and in general temperature and pulse rate will rise. In cases of pelvic peritonitis arising from an inflamed appendix in the pelvic position or from salpingitis, the abdominal signs are often slight; there may be deep tenderness of one or both lower quadrants alone, but a rectal or vaginal examination reveals marked tenderness of the pelvic peritoneum. With early diagnosis and adequate treatment, this condition is rarely seen in modern surgical practice. It is first experienced at the site of the original lesion and spreads outwards from this point. Tenderness and generalised guarding are found on palpation, when the peritonitis affects the anterior abdominal wall. Infrequent bowel sounds may still be heard for a few hours but they cease with the onset of paralytic ileus. Serum amylase estimation may establish the diagnosis of acute pancreatitis provided that it is remembered that moderately raised values are frequently found following other abdominal catastrophes and operations. A supine radiograph of the abdomen may confirm the presence of dilated gas-filled loops of bowel (consistent with a paralytic ileus), and occasionally show other gasfilled structures that may aid diagnosis. There is an abundance of recent published evidence to support its use in managing acute abdominal pain. Ultrasonography has undoubted value in certain situations such as pelvic peritonitis in women and localised right upper quadrant peritonism. Management (b) General care of the patient the care of critically ill surgical patients is described in detail in Chapters 2, 17 and 20. Nutritional support is covered in Chapter 19, and anaesthesia and pain relief in Chapter 18. Depending on degree (localised/generalised), duration and severity, patients will require some or all of the following. Special measures may be needed for cardiac, pulmonary and renal support, especially if septic shock is present (see Chapter 2), including central venous pressure monitoring in patients with concurrent disease. A nasogastric tube is commonly passed to allow drainage ± aspiration until paralytic ileus has resolved. If appropriate expertise is available, epidural infusion may provide excellent analgesia. Freedom from pain allows early mobilisation and adequate physiotherapy in the postoperative period, which helps to prevent basal pulmonary collapse, deep vein thrombosis and pulmonary embolism. The use of a large volume of saline (typically 3 litres) containing dissolved antiseptic or antibiotic has been shown to be effective. Prognosis and complications With modern treatment, diffuse peritonitis carries a mortality rate of about 10%, reflecting the degree and duration of peritoneal contamination, age and fitness of the patient, and the nature of the underlying cause. Paralytic ileus is covered in detail in Chapter 71, and abscess formation and adhesions are covered below. This rule is particularly true for previously healthy patients and those with postoperative peritonitis. More caution is of course required in patients at high operative risk because of comorbidity or advanced age. In those patients with a preoperative diagnosis, if the cause of peritonitis is amenable to surgery, an operation must be carried out as soon as the patient is fit. In peritonitis caused by pancreatitis or salpingitis, or in cases of primary peritonitis of streptococcal or pneumococcal origin, non-surgical treatment is preferred, provided that the diagnosis can be made with confidence. It is beyond the remit of this chapter to cover specific causes of peritonitis and their treatment, be it by an open or a laparoscopic approach. However, in general, surgery is directed to removing (or diverting) the cause and subsequent adequate peritoneal lavage ± drainage. Unless the bile has extravasated slowly and the collection becomes shut off from the general peritoneal cavity, there are symptoms (often severe pain) and signs of diffuse peritonitis.
It is essential to appreciate that the physiological crisis initiated in the immediate aftermath of trauma will continue to evolve and the risk of mortality is substantial unless the correct and timely interventions are performed chronic gastritis with intestinal metaplasia nexium 40 mg without a prescription. For instance, conditions such as airway obstruction, tension haemothorax and haemopericardium can progress very rapidly if left untreated and should be given priority in terms of our initial medical response to the injured patient. Thus, the seriousness and the immediate impact of a specific clinical condition should be prioritised and treated in a systematic approach (what kills first should be managed first). Evaluating and diagnosing a condition can be challenging, as the initial clinical signs may be non-specific. The clinical condition will continue to evolve as the time progresses, but by the time the diagnosis has been made it may be too late to prevent mortality. Surgical decompression can be organised speedily, reducing the risk of morbidity and mortality. Reducing the diagnosis time and response time of our interventions is dependent not only on the clinical staff but also on the availability of resources. Recently, the 24/7 availability of the trauma team and the designation of regional hospitals to operate as Level I Trauma Centres, with the availability of all disciplines and appropriate equipment on site, has provided the necessary foundation for the development of a unified trauma care system in England. Indeed, the first reports published on its effectiveness in saving lives have been very positive. Such a strategy may reduce the risk of having undiagnosed injuries and delays in their treatment. A number of studies have been published reporting on missed injuries and making some recommendations on how to avoid this. The timeline following an injury is continuous, and the accumulated documentation may become voluminous, complex and confusing. It is helpful periodically to make the effort to stand back and summarise the situation. The associations among these three factors are usually very clear, but can be hidden. For instance, a 50-year-old male restrained passenger in a car involved in a head-on collision with another vehicle may sustain rib fractures, a sternal fracture, thoracic spine fracture and possibly cardiac contusion. Abdominal injuries could also be suspected but, overall, the clinician, knowing the mechanism, can proceed quickly in making the diagnosis and initiating treatment. We will now analyse how the clinician can make best use of the information available. It can be seen that relying on obvious clinical signs gives insufficient time to respond effectively. The key issue, irrespective of the type of patient managed, with or without multiple injuries, is to reduce unnecessary delays in making the diagnosis and initiating appropriate treatment. Such a global approach would save lives, minimise morbidity and would make the healthcare system more efficient in terms of resource utilisation, as well as cost-effectiveness. Finally, it should not be forgotten that all clinical conditions are characterised by a dynamic process. This implies that our observations and analysis of the situation can change rapidly and to an extent that interventions would have to be modified accordingly. Ongoing evaluation of the patient is therefore essential in order to identify and respond to the changes noted in a timely fashion (as previously discussed). Ongoing monitoring of vital organ activity, ordering of the necessary biochemical and radiological investigations and recording of all the findings in a single place can allow easier evaluation Include the information formula: mechanism + patient = injury Look for both obvious and less obvious features Identify more reasons when the above formula does not make sense Mechanisms Mechanisms may be blunt, penetrating or even of a combined nature (Table 22. Blunt trauma can be categorised as direct or indirect, and continues to be the most common mechanism. For example, a direct kick to the medial aspect of the mid-shaft of the tibia in a footballer by an opponent will induce an isolated tibial fracture. Such an injury represents a direct mechanism with bruising and ecchymosis at the area of the force exertion. On the other hand, a fall from a height of 1 metre with a twisting moment as the foot hits the ground can lead to a spiral fracture of the distal tibia. In this case, other injuries should also be looked for, such as a fibular fracture or even an ipsilateral tibial plateau fracture, around the knee joint area. For instance, a minimally displaced tibial fracture that a footballer has sustained can be treated satisfactorily for some time after the moment of injury but, in contrast, a fracture of the acetabulum with a hip dislocation (as described above) represents an emergency owing to the potential development of neurovascular complications (damage to sciatic nerve; avascular necrosis of the femoral head). Moreover, it should be appreciated that the conduction of energy in an indirect mechanism, which is transferred via the soft tissues or fluid, can be difficult both to understand and to diagnose (accurately and promptly). For example, the rise in pressure secondary to a lower abdominal force could be passed to the vascular tree (aorta), leading to unexpected haemorrhage and death. All in all, one can argue that the effects of direct mechanisms are easier to comprehend than those of indirect ones. Penetrating mechanisms can be divided into those caused by sharp objects and those induced by firearms (see Chapter 30). With regard to injuries caused by sharp objects, it is necessary to take into account the length of the sharp object, its surface area and the size of the entry point. The sharp object, for example a pair of scissors, will cause damage to the underlying tissues that it contacts (skin, subcutaneous fat, fascia, etc. Local examination will confirm the extent of the injury and the need for wound exploration. Being familiar with the relevant anatomy of the area involved allows assessment of the peripheral nerve function, and tendon and muscle integrity. Knowledge of the anatomical structures at risk is essential to making the right decision in a timely fashion.
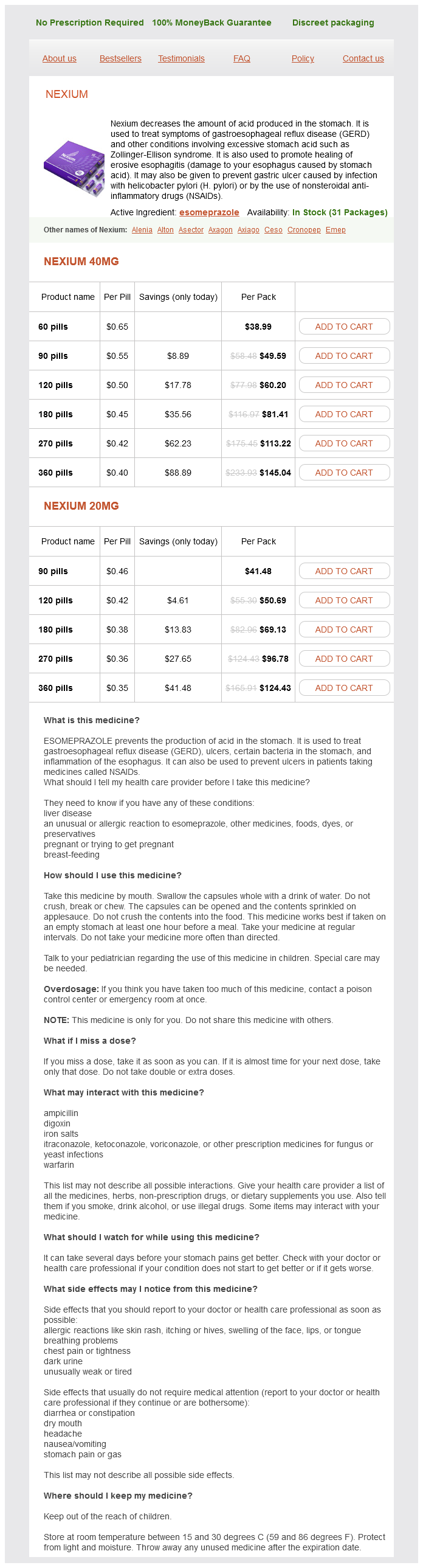
Nexium Dosage and Price
Nexium 40mg
- 60 pills - $38.99
- 90 pills - $49.59
- 120 pills - $60.20
- 180 pills - $81.41
- 270 pills - $113.22
- 360 pills - $145.04
Nexium 20mg
- 90 pills - $41.48
- 120 pills - $50.69
- 180 pills - $69.13
- 270 pills - $96.78
- 360 pills - $124.43
Release each artery in turn and observe the return of colour Tap over the nerve of interest gastritis diet ���� cheap nexium 40 mg fast delivery. Tingling may indicate nerve compression Place the wrist in maximum flexion with the elbows extended Ask the patient to grip a sheet of paper between the index finger and thumb of both hands. The scaphoid tubercle, pisiform and the hook of hamate are all palpable on the volar aspect of the wrist. A general screening assessment is to ask the patient to roll up their fingers from full extension to full flexion. Move the wrist can be moved into flexion and extension, and ulnar and radial deviation. Extensors and flexors Asking the patient to grip two of your fingers in their fist tests the power of the extensors of the wrist (radial nerve) because they are needed to brace the wrist. Asking the patient then to extend and spread their fingers apart against resistance tests the intrinsic muscles of the hand (mainly the ulnar nerve). If the test finger is able to flex, despite profundus being immobilised, then the superficialis tendon to that finger is working. Wrist flexion and extension, ulnar and radial deviation Hand thumb movements, metatarsophalangeal joints and small joints of the hand Abductor pollicis brevis. With the hand lying flat on a table with the palm facing upwards, ask the patient to raise the thumb towards the ceiling. Note that compression of the ulnar nerve at the elbow leads to wasting distally in the hypothenar eminence and intrinsic muscles of the hand assess the hand for the presence of clawing and wasting. This angle allows the elbow to be tucked into the waist depression above the iliac crest: cubitus varus (gun-stock deformity): the carrying angle is reversed, secondary to a malunited supracondylar fracture; cubitus valgus: the carrying angle is increased, caused by malunion of a distal humeral fracture; hyperextension: there is normally a physiological hyperextension of the elbow (5°). The ulnar nerve can be rolled under your fingers placed between the medial epicondyle and the olecranon. Test the distal sensation in the hand (especially in the distribution of the ulnar nerve) and assess the vascular status. The three palpation landmarks are the medial and lateral epicondyles and the apex of the olecranon. The more common anterior dislocation often presents with an anterior bulge and a squared-off shoulder. The medial epicondyle is the common origin of the forearm flexors and the pronator muscle. The diagnostic test is resisted wrist flexion, which reproduces the pain over the medial epicondyle. Palpate for tenderness usually just distal (510 mm) to the epicondyle near the origin of the extensor carpi radialis brevis muscle. Referred pain may present from the cervical spine, heart, mediastinum and the diaphragm. At the side, the deltoid splitting approach and lateral arthroscopic portals may be seen. Wasting of the deltoid muscle is commonly seen after shoulder dislocation when there is a temporary loss of function of the axillary nerve that supplies it. The rotator cuff comprises four muscles: supraspinatus, infraspinatus, subscapularis and teres minor. Move Differentiate between movements of the shoulder joint and scapulothoracic movement of the scapula on the chest wall. Patients with a painful shoulder will commonly move from the scapulothoracic joint. Stabilise the scapula by placing the thumb over the coracoid process and the fingers of the same hand over the spine of the scapula. Ask the patient to raise their hands in front to touch the ceiling while keeping the elbows extended (0180°). Beyond this the scapula begins to rotate on the thorax and final movements are almost entirely scapulothoracic. Ask the patient to touch their back with the dorsum of the hand and to raise their hand up the back as high as possible (normal range is thoracic spine level T79). With the arms by the sides, bend the elbows to 90° and rotate the forearms to the mid-prone position. Special tests and diagnoses Impingement syndrome this is impairment of rotator cuff function within the subacromial bursa. Impingement is characterised by pain and weakness on abduction and internal rotation. Ask the patient to abduct the arm to 90° elevation in the scapular plane with full internal rotation (empty can position). Shoulder instability Instability may be defined as a shoulder that slips in and out of joint (dislocation) more than once or twice, or frequently slips partially out of joint and then returns on its own. With the patient supine or standing, flex the elbow to 90° and abduct the shoulder to 90°. Look at the posture of the limb and assess for adduction deformity; fixed adduction may be present in severe osteoarthritis and cerebral palsy, and makes the leg appear short because the pelvis is tilted (apparent shortening). Front asymmetry, deformity Side muscle wasting Back muscle wasting, scapula Feel Inspection of the supine patient Skin, scars, soft tissues, deformity Palpation of shoulder girdle (sternum to scapula) Movements Soft tissues. Tenderness overlying the greater trochanter may suggest trochanteric bursitis or an abductor enthesopathy. Typical clinical diseases of the hip that may be encountered in children and adults are shown in Table 31. A patient complaining of hip pain should undergo a careful examination of the spine, abdomen, pelvis, groin and thigh.