Nifedipine
General Information about Nifedipine
Nifedipine works by blocking the movement of calcium into the muscle cells of the center and blood vessels. This causes the blood vessels to loosen up and widen, reducing the pressure towards the artery walls. As a result, blood can flow more simply and effectively through the physique, decreasing blood strain and relieving angina symptoms.
In addition to its major uses, nifedipine has additionally been discovered to be useful in treating different conditions, corresponding to Raynaud's phenomenon (a situation that causes numbness and ache in the fingers and toes) and high altitude pulmonary edema (fluid accumulation in the lungs attributable to high altitudes).
Nifedipine is available in two forms, immediate-release and extended-release. The immediate-release type is taken three times a day, whereas the extended-release type is taken as soon as a day. It is necessary to take nifedipine exactly as prescribed by a healthcare skilled, as it's a sensitive medicine and the dose should be rigorously monitored.
Nifedipine is a highly effective medicine for treating hypertension and angina. Studies have shown that it could considerably decrease blood stress and decrease the frequency and severity of angina assaults. It may help stop heart assaults and strokes in individuals with hypertension.
The most common side effect of nifedipine is a headache, which could be relieved by taking a non-steroidal anti-inflammatory drug (NSAID) like ibuprofen. Other attainable unwanted facet effects include nausea, dizziness, and flushing of the face. In uncommon cases, nifedipine can cause extra severe unwanted facet effects, corresponding to allergic reactions, irregular heartbeat, and swelling of the arms and feet. If any of these symptoms occur, it is essential to seek medical attention immediately.
It is necessary to notice that nifedipine shouldn't be taken by individuals who've a history of heart failure, liver issues, or low blood stress. It can also work together with certain medicines, such as beta blockers, anti-seizure medicine, and antibiotics, so it's essential to inform the physician of some other drugs being taken.
Hypertension is a condition the place the drive of blood in opposition to the artery partitions is just too excessive and can result in critical health issues, such as heart attack, stroke, or kidney disease. Angina is a sort of chest pain that happens when there is a lack of blood flow to the center, often brought on by a blockage in the arteries.
In conclusion, nifedipine, also known as Adalat, is a commonly prescribed treatment for hypertension and angina. It works by relaxing the blood vessels and growing blood flow, successfully lowering blood strain and relieving chest pain. It is necessary to take nifedipine as prescribed and to concentrate on potential unwanted effects. With correct use, nifedipine can significantly improve the well being and well-being of those dwelling with hypertension and angina.
Nifedipine, commonly recognized by its brand name Adalat, is a drugs used to treat hypertension (high blood pressure) and angina (chest pain). It belongs to a class of medicine called calcium channel blockers, which work by relaxing the blood vessels and rising blood move.
This is followed by Achilles tenotomy in the majority of patients and 3 further weeks of casting arrhythmia can occur when 20 mg nifedipine order. Children are then placed into a foot abduction orthosis full-time for a period of 3 months, and then part time, while sleeping, until approximately age 4 years. Torsional deformities of the lower extremities rarely come to the attention of the physician before the child reaches walking age. Occasionally a neonate demonstrates bowing of the legs, or genu varum, of a sufficient degree to concern parents or grandparents. The true incidence of genu varum is unknown, but based on our experience, it is extremely common. The overwhelming majority of cases of genu varum resolve spontaneously, with a small minority of affected children manifesting a pathologic condition. This results from a combination of an external rotation contracture of the hips and internal tibial torsion. The apex anterior bowing of the femora in conjunction with the external rotation contractures of both hips allow the femoral bowing to be seen tangentially when the baby is viewed from the front. Internal tibial torsion is nearly universal in neonates and spontaneously resolves between 2 and 3 years of age. When tibial bowing is viewed in combination with the apparent femoral bowing, a striking amount of leg bowing may be present. Salenius and Vankka (1975) documented the tibiofemoral angles both clinically and roentgenographically in 979 children on the basis of 1408 examinations between birth and 16 years of age. They noted that newborns demonstrate a mean varus alignment of 15 degrees, which increases and becomes maximal at 6 months of age and then decreases to neutral at approximately 18 months. Genu varum with angulation greater than 30 degrees has been shown to correct spontaneously with growth (Heath and Staheli, 1993). Physical examination should include evaluation of the torsional profile (Staheli, 1977), which includes measurements of internal and external rotation of the hips and the thigh-foot angle. Measurement of the thigh-foot angle is performed with the child in the prone position and is an indicator of tibial torsion. The examiner should look for evidence of rhizomelic shortening, and genu varum, which may herald a diagnosis of achondroplasia or other skeletal dysplasia. Finally, note is made of whether onset of the varus of the lower extremities is gradual or abrupt. If it was abrupt, can the deformity be localized to the distal femur, the proximal tibia, or the midportion of the tibia Considerations in the differential diagnosis of genu varum include focal fibrocartilage dysplasia, skeletal dysplasias such as achondroplasia, osteogenesis imperfecta, and metabolic bone disease such as vitamin Dresistant rickets, renal osteodystrophy, and tibia vara (infantile Blount disease). Blount disease does not occur before walking age, and most clinicians agree that this diagnosis cannot be made before 2 years of age. Radiographs are indicated only with asymmetric deformities, with short stature, or in infants with progressive deformities. Management of physiologic genu varum and tibial torsion consists of serial observation, reassurance, and parental education. Treatment with orthotics such as the Denis Browne splint is not indicated and in fact may be harmful to the ligaments of the knee. It was first reported in 1985 by Bell et al and continues to be recognized in scattered case reports. The pathophysiologic basis for the disease may be abnormal development of fibrocartilage at the insertion of the pes anserinus (sartorius, gracilis, and semitendinosus tendons). The radiographs demonstrate a lytic defect in the proximal medial metaphysis of the tibia with surrounding sclerosis. The natural history of the deformity is that of progression until 2 years of age, with subsequent resolution by 4 years of age. Surgery is indicated only in patients older than 4 years without evidence of spontaneous resolution (Zayer, 1980). Two major types of bowing can be identified according to the direction of the apex of the bow. Posteromedial bowing has been previously described in conjunction with calcaneovalgus foot position in the neonate. Its etiology is unknown, but numerous hypotheses have been proffered, including intrauterine fracture with malunion and in utero malpositioning with subsequent growth retardation and soft tissue contractures (Thompson, 2001). Other features include shortening of the tibia and a smaller calf circumference and smaller foot relative to the contralateral side. Radiographic examination of the entire extremity from hip to ankle should be performed. Other radiographic findings include a normal proximal tibia with thickening and sclerosis of the diaphyseal cortices on the compression side of the deformity with obliteration of the intramedullary canal. Posteromedial bowing tends to resolve with growth, so that much of the deformity resolves by 2 years of age, with continued gradual correction beyond that. The shortening of the tibia and fibula persists, however, and progressively worsens during growth. Early referral to and serial follow-up assessments by a pediatric orthopedist are necessary to appropriately time epiphysiodesis surgery of the normal longer leg to allow for equal leg lengths at skeletal maturity. It most frequently is associated with congenital pseudoarthrosis of the tibia but also can be associated with congenital longitudinal deficiency of the tibia or the fibula. It is arguably the most challenging congenital malformation to treat in orthopedics.
Patients with stage 1 and stage 2 neuroblastoma have a 96% to 100% survival rate with surgery alone (Perez et al blood pressure guidelines 2015 purchase discount nifedipine line, 2000). Infants with stage 3 and stage 4 disease have a poorer survival, even with aggressive chemotherapy, although the outcome, with better than 70% surviving overall, is far better than the 10% to 20% reported for older children with these stages (Schmidt et al, 2000). Infants with stage 4S disease have a very good prognosis, with a 5-year survival >90%, despite having disseminated disease. The unpredictable course of neuroblastoma, with its occasional spontaneous maturation or regression, not only makes this tumor unusual but also causes difficulty in planning therapy. Such patients should undergo surgical resection or partial resection, but they likely will not derive any additional benefits from postoperative chemotherapy or radiation therapy. An exception to this rule is in the case of spinal cord compression, in which prompt decompression with chemotherapy, laminectomy, or local irradiation may be used to preserve function. There is an increasing trend to use chemotherapy first, given the exquisite sensitivity of the tumor to chemotherapeutic agents, but a rapid deterioration in neurologic function should prompt alternative interventions. The combination of extensive laminectomy with postoperative irradiation should be avoided because later spinal deformity is almost inevitable. Infants with stage 3 and stage 4 disease usually are treated with combination chemotherapy and local surgery, with radiation therapy given only as necessary to eradicate residual disease. Active drugs that are most commonly used include cisplatin, etoposide, doxorubicin, cyclophosphamide, vincristine, and ifosfamide. In these high-risk patients, intensive chemotherapy followed by myeloablative therapy and stem cell support may offer additional benefit (Canete et al, 2009). In addition, the use of the differentiation agent cis-retinoic acid has been shown to improve survival in patients with advanced-stage, high-risk neuroblastoma (Matthay et al, 2009). Infants with stage 4S disease have a highly favorable prognosis and may require minimal or no therapy. Because many patients undergo spontaneous regression without chemotherapy and the overall disease-free survival rate is 85% to 90%, therapy should be directed toward supportive care, with use of chemotherapy and surgery restricted to relieving symptoms (De Bernardi et al, 2009). The main cause of death in these patients is massive hepatic involvement resulting in respiratory insufficiency or compromise of renal or gastrointestinal function. When there is a risk of organ impairment due to tumor bulk not responding to initial chemotherapy, low-dose radiotherapy can be administered (450 cGy given in three fractions). Prenatal Diagnosis Neuroblastoma is increasingly being detected prenatally by screening ultrasonography. Newborns with adrenal or other mass lesions detected prenatally should be evaluated with urine catecholamines and follow-up ultrasonography. Careful observation may be adequate for infants with localized tumors, which frequently regress. Newborn Screening Newborn screening for neuroblastoma by measuring urine catecholamines has been studied in Japan and a number of other countries (Hiyama et al, 2008). It was hoped that early diagnosis of neuroblastoma would reduce the frequency of cases with poor prognosis from advanced-stage disease. Screening, however, has shown no impact on survival; neuroblastomas detected by screening almost always have favorable biologic features (Schilling et al, 2002). Thus, routine screening of infants for neuroblastoma is not currently recommended. Two thirds of congenital leukemia cases arise from the myeloid lineage, in contrast to older infants and children in whom acute lymphoblastic leukemia predominates. Congenital leukemia is associated with a high mortality with an overall survival at 24 months of only 23% (Bresters et al, 2002); this is due to the aggressive biology of these leukemias and to treatment complications. In infants and older children, a number of factors are associated with the development of leukemia; these include genetic factors, environmental influences, viral infections, and immunodeficiency. Leukemia-associated gene rearrangements have been retrospectively identified in archived newborn blood spots of children who subsequently developed leukemia (Hjalgrim et al, 2002; Taub et al, 2002; Wiemels et al, 2002). Intrauterine exposure to topoisomerase 2 inhibitors may be responsible for some cases of infant leukemia (Pui and Evans, 1999; Ross, 2000). Nucleotides involved in the breakpoint of the 11q23 locus may be particularly susceptible to topoisomerase 2induced breaks (Strick et al, 2000). Clinical Manifestations Clinical signs of leukemia may be evident at birth and include hepatosplenomegaly, petechiae, and ecchymoses. Patients typically have multiple nodules that are freely movable over the subcutaneous tissue (Resnik and Brod, 1993). There is usually a greenish-blue discoloration of the overlying skin due to the abundance of myeloperoxidase-hence the name chloroma. It is important to perform cytogenetic studies, in addition to flow cytometry, on the skin biopsy specimen; infants found to have an 11q23 rearrangement have a poor prognosis even in the absence of marrow involvement and should be treated aggressively (Zhang et al, 2006). When chloromas are present on the head or neck, imaging studies should be obtained to assess for the presence of intracranial or skull involvement. At birth, many infants have respiratory distress from leukemic infiltration in the lungs. Severe respiratory difficulty may develop soon after birth from pulmonary hemorrhage secondary to thrombocytopenia. In those infants in whom signs of the disease develop within the 1st month but in whom no detectable signs of leukemia were noted at birth, presenting symptoms and signs are nonspecific, including lethargy, diarrhea, hepatomegaly, and poor feeding with failure to gain weight. In addition, affected infants can present with fever due to bacterial infections or hemorrhagic manifestations due to thrombocytopenia. Laboratory Manifestations Hemoglobin levels may be normal initially, but anemia soon develops as the normal postnatal decrease in red cell production is combined with the expansion of the leukemic clone in the marrow. Total white blood cell count may be normal or decreased, but leukocytosis is more often present. White blood cell counts of 150,000 to 250,000/mm3 or higher are common, and counts as high as 1.
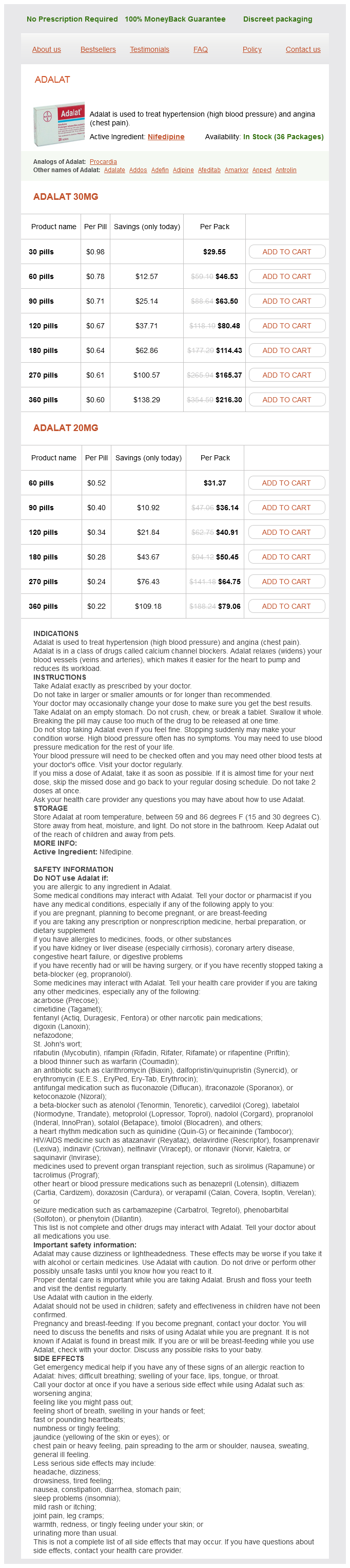
Nifedipine Dosage and Price
Adalat 30mg
- 30 pills - $29.55
- 60 pills - $46.53
- 90 pills - $63.50
- 120 pills - $80.48
- 180 pills - $114.43
- 270 pills - $165.37
- 360 pills - $216.30
Adalat 20mg
- 60 pills - $31.37
- 90 pills - $36.14
- 120 pills - $40.91
- 180 pills - $50.45
- 270 pills - $64.75
- 360 pills - $79.06
In the first edition of this textbook arteria infraorbitalis cheap 20 mg nifedipine with amex, limited attention was devoted to neonatal neurology. Beginning with the eighth edition, the book now features a comprehensive neurology section that, in addition to this introductory chapter, includes chapters devoted to neonatal neuroimaging; malformations and deformations of the developing brain; brain injury and neuroprotection; neuromuscular disorders; neonatal seizures; and finally, risk assessment and neurodevelopmental outcomes. The blood-brain barrier is essentially a collection of capillaryendothelial cell tight junctions and develops under the influence of astrocytes. Cerebral vascular development, particularly in the periventricular region, is clinically relevant because the immature infant is susceptible to ischemic injury in the white matter around the ventricles and to hemorrhage in the germinal matrix region (part of the ventricular zone) and into the ventricles (Takashima and Tanaka, 1978a, 1978b). Perforating arteries branch from leptomeningeal arteries, penetrate the cerebral cortex, and terminate as capillary beds adjacent to the ventricles. Branches of choroidal and striate arteries project toward the lateral ventricles and then deviate away from the ventricle toward their final termination in vascular capillary beds in the periventricular white matter. It has been proposed that these vascular beds collectively form vascular end zones and border zones that render the periventricular white matter particularly susceptible to ischemia. However, the existence of these border zones remains controversial (Mayer and Kier, 1991; Nelson et al, 1991; Takashima et al, 2009; Volpe, 2008). Recent studies in the preterm fetal sheep measured blood flow in histopathologically defined regions of injury in cerebral cortex and white matter (McClure et al, 2008). Although white matter blood flow is lower than cerebral gray matter, there was no evidence for pathologically significant gradients of fetal blood flow within the periventricular white matter under conditions of ischemia or reperfusion. White matter lesions did not localize to regions susceptible to greater ischemia, nor did less vulnerable regions of cerebral white matter have greater flow during ischemia. An alternative explanation for the topography of cerebral white matter lesions is the distribution of susceptible cell types, particularly late oligodendrocyte progenitors, that are particularly susceptible to hypoxiaischemia (Back et al, 2005; Riddle et al, 2006). A current limitation to our understanding of human cerebral vascular development is the lack of approaches that precisely measure regional blood flow in real time in the preterm or term neonate. Preterm survivors studied longitudinally up to 18 months of age demonstrated a persistent reduced tortuosity of proximal segments of all major cerebral arteries (Malamentiniou et al, 2006). They observed "a high prevalence of variant types of the circle of Willis" with corresponding variations in flow in the internal carotid and basilar artery. The significance of this finding with regard to regional blood flow, brain injury, brain development, or vulnerability to injury later in life is not known. Cortical and subcortical veins drain in the meningeal direction from cortex and superficial white matter, whereas medullary veins drain in the ventricular direction from the deep white matter. Characteristics of the developing vasculature, such as the fact that the medullary veins in the deeper cerebral white matter are more developed than the veins in the subcortical white matter, may predispose the developing deep white matter to certain types of injury, particularly periventricular venous infarction that occurs in association with intraventricular hemorrhage (Volpe, 2008). Despite the potential benefits of short-term treatment with antiangiogenesis factors, the potential of these agents to cause hypoxia to the germinal matrix or other tissues remains unclear. When blood flow regulatory limits and oxygen extraction capabilities of the brain are exceeded, the brain sustains tissue hypoxia. In most clinical situations, both hypoxia and ischemia occur, although one may predominate. It should be emphasized that even under conditions of significant hypoxia-ischemia, cerebral injury is often selective rather than diffuse. For example, under conditions of prolonged global cerebral ischemia, the cerebral cortex is relatively spared in the preterm fetal sheep, whereas panlaminar cortical necrosis occurs in the term animal (Reddy et al, 1998; Riddle et al, 2006). In a fetal rabbit model of placental insufficiency, significant global fetal hypoxia-ischemia caused minimal preterm cerebral white matter injury, but a similar insult three days later in gestation causes pronounced white matter injury (Buser et al, 2010). The timing of appearance of susceptible oligodendroglial progenitors defined the relative susceptibility of the white matter at these two developmental ages. Hence, the extent of the susceptibility to hypoxia-ischemia is related to both the timing and the regional expression of cellular-molecular factors. Although the germinal matrix is considerably more vascular than the cerebral cortex or white matter, the increased risk for hemorrhage is related to developmental immaturity of the vasculature and the cellular and extracellular matrix elements that make up the blood-brain barrier. In recent years, the relative contributions of several of the key molecular components of the blood-brain barrier to germinal matrix hemorrhage have been studied. The barrier is composed of astrocytic endfeet, pericytes, basement membrane, and endothelial tight junctions. Pericytes are involved in both the initiation of angiogenesis and the later stabilization of blood vessels via the synthesis of components of the extracellular matrix and regulation of endothelial differentiation. Perivascular coverage by astrocytic endfeet and pericytes is reduced in human preterm germinal matrix relative to other brain regions (Braun et al, 2007; El-Khoury et al, 2006). Studies of the ultrastructural features of the blood-brain barrier in an animal model initially suggested that postnatal endothelial basal lamina deposition occurs before tight junction formation and glial investiture and that basal lamina induction influences the latter two processes (Ment et al, 1995). Various candidate molecules have been proposed to contribute to the stabilization of the matrix vasculature in the first days of life, including laminin, collagen V (Ment et al, 1991), and fibronectin (Xu et al, 2008), all of which increase significantly with advancing age after birth. Enhanced expression of these molecules in the germinal eminence was promoted by indomethacin (Ment et al, 1991) or low-dose prenatal betamethasone (Xu et al, 2008), suggesting that these agents might stabilize the germinal matrix vasculature. The biology of vascular maturation is an active research area that raises an alternative strategy for prevention of intraventricular hemorrhage. Endothelial proliferation declines in the 1st week of life in human germinal matrix, which supports the notion that angiogenesis is in an active phase around the time of birth (Ballabh et al, 2007). Cerebral autoregulation has been demonstrated in several species and across developmental stages, but the mechanism of this important phenomenon remains elusive. In late fetal lambs, the range is lower and narrower (40 to 80 mm Hg), but more importantly, normal blood pressure is at most 5 to 10 mm Hg above the lower limit of the autoregulatory curve (Papile et al, 1985).