Nitrofurantoin
General Information about Nitrofurantoin
One of the biggest benefits of nitrofurantoin is that it is efficient in opposition to each Gram-positive and Gram-negative bacteria, that are the main culprits of UTIs. This makes it a suitable choice for patients who may not know which bacteria is causing their an infection, as it covers a broad spectrum of pathogens. Additionally, nitrofurantoin is relatively affordable and has a low chance of causing antibiotic resistance, making it a cost-effective and secure selection for treating and stopping UTIs.
In abstract, nitrofurantoin is a well-established and effective treatment for treating and preventing UTIs. It is a broad-spectrum antibiotic that's relatively secure and reasonably priced. However, it is crucial to observe the prescribed dosage and period of remedy to make sure that the an infection is fully eradicated and to reduce the danger of potential side effects. If you experience any sudden symptoms while taking nitrofurantoin, do not hesitate to contact your physician. With correct use, this treatment might help alleviate the discomfort and inconvenience of UTIs and enhance the standard of life for those affected by this frequent health issue.
One important concern with nitrofurantoin is its potential to trigger birth defects if taken through the first trimester of being pregnant. It is, due to this fact, not beneficial to be used in pregnant girls. It can be not appropriate for use in infants beneath one month of age, as their still-developing kidneys may not be ready to deal with the medication.
Urinary tract infections (UTIs) are a standard and uncomfortable well being problem that affects millions of individuals every year. One of the most generally used antibiotics for treating and preventing UTIs is nitrofurantoin. This treatment has been in use for over 60 years and is still a popular alternative for healthcare providers because of its effectiveness and comparatively low unwanted side effects. In this article, we are going to focus on every thing you have to know about nitrofurantoin, from its mechanism of motion to its advantages and potential risks.
Nitrofurantoin is available in both immediate-release and sustained-release varieties. The immediate-release form is often prescribed for acute UTIs and must be taken 4 times a day for seven days. On the opposite hand, the sustained-release form only requires once-daily dosing, making it extra convenient for sufferers who want ongoing therapy or prophylaxis for recurrent UTIs. It is important to observe the prescribed dosage and course of remedy to make sure the best likelihood of fully eliminating the infection.
Nitrofurantoin is an antibiotic that belongs to the class of drugs called nitrofuran derivatives. It was first discovered within the 1950s and has since been used to deal with and stop urinary tract infections attributable to certain kinds of bacteria, corresponding to E. coli, Enterococcus, and Staphylococcus saprophyticus. It works by interfering with the bacteria's capability to provide proteins, finally resulting in their demise.
As with all medications, nitrofurantoin does have some potential unwanted effects. The commonest ones reported are gastrointestinal symptoms, such as nausea, vomiting, and diarrhea. These are often mild and may be managed by taking the treatment with meals. However, in rare circumstances, critical unwanted effects similar to lung or liver toxicity might occur. Patients with a historical past of liver illness ought to be cautious and notify their healthcare provider if they experience any unusual signs while taking nitrofurantoin.
Less than 2% of patients with disseminated disease have laryngeal involvement treatment for uti medications buy nitrofurantoin 100 mg with amex, with such almost exclusively occurring in immunocompromised patients. Coccidioidomycosis is an uncommon fungal infection seen primarily in areas of California, Arizona, and northern Mexico where the Coccidioides immitis fungus is ubiquitous in soil and dust. Similar to the other fungal infections discussed above, inhalation of spores is the primary route of inoculation and most patients are asymptomatic (60%) with few (0. In the largest case series involving 12 patients with laryngeal coccidioidomycosis, seven were children and nine presented with airway compromise. Treatment consists of systemic antifungal medication primarily amphotericin B combined with an azole agent. Local debridement and tracheostomy may be necessary in patients with airway obstruction. Disseminated aspergillosis is a disease of immunocompromised individuals in almost all circumstances. Primary infection of the larynx or trachea is exceedingly rare, especially in immunocompetent patients with fewer than 20 adult cases reported. Laryngeal infection is usually invasive resulting in a granulomatous inflammatory response with resulting tissue necrosis; superficial aspergilloma has been reported as well. Sporothrix schenckii, a dimorphic fungus that grows as a mold in nature,i causes infection via traumatic inoculation of contaminated plant material into the skin, then spreads via the lymphatic system. There have been two case reports of laryngeal sporotrichosis, both in immunocompetent patients, and one occurring in a 19-monthold girl. Successful treatment of disseminated disease requires systemic antifungal medications including amphotericin B and itraconazole. Sarcoidosis is a multisystem inflammatory disease of unknown etiology that is manifested by non-caseating granulomas in the affected organ. It is a ubiquitous disease with an incidence that varies according to age, sex, race and geographic origin. Subglottic involvement also occurs in 20% of cases whereas glottic involvement is very rarer. Supportive but not pathognomonic findings on laboratory testing include elevated serum angiotensin converting enzyme, elevated erythrocyte sedimentation rate, and evidence of abnormal calcium metabolism. The diagnosis is made based on the combination of clinical and radiological presentation, evidence of noncaseating granulomas on biopsy, and exclusion of other granulomatous diseases. The treatment of isolated laryngeal sarcoidosis revolves around maintaining airway patency. Tracheostomy may be necessary in airway compromise, and laser resection and balloon dilation are useful endoscopic adjuncts. Oral or parenteral corticosteroids have been used with success in the past for patients with symptomatic laryngeal sarcoidosis. Intralesional corticosteroid injections may help resolve localized disease and prevent progression of airway obstruction. Wegener granulomatosis is characterized by necrotizing granulomatous inflammation and necrotizing vasculitis affecting small to medium sized vessels, with larger vessels rarely affected. Although usually a systemic disease, rare isolated airway manifestations do occur, and airway involvement is reported in 15 to 55%. Clinical history and physical examination may reveal evidence of other airway, lung and kidney manifestations that further support the diagnosis. Medical management includes corticosteroids for systemic disease as well as immunomodulating medications like cyclophosphamide, methotrexate, and rituximab. Endoscopic techniques including balloon airway dilation and laser debulking, as well as the adjuvant use of intralesional corticosteroids and topical mitomycin C, can help maintain airway patency. Open airway surgery (resection and reanastomosis) for isolated short-segment stenosis is a possibility if endoscopic treatment fails. It is the most common benign neoplasm of the larynx in children and tends to take a more aggressive disease course in this patient population. Children who are diagnosed at a younger age have a higher risk for disease progression compared with children diagnosed later in life. Fortunately, few children born to mothers with active genital lesionsdevelop papillomas. Therefore, other factors such as localized trauma, defects in cellular and humoral immunity, and extraesophageal reflux are likely important in the development and persistence of this disease. E4 is associated with viral release from infected cells, and E6 and E7 are probably associated with viral transformation. The L1 protein is the primary protein of the viral capsid (with some of L2 embedding deeply) and provides the dominant antigenic epitopes recognized by neutralizing antibodies. The prevalence of clinically apparent genital papilloma in the United States is approximately 1% of the population. The duration of symptoms until diagnosis ranges from less than one year to as long as eight years with a mean of two years. Histologically, papillomas demonstrate finger-like projections of nonkeratinized-stratified squamous epithelium supported by a core of highly vascularized connective tissue stroma. Childhood onset disease commonly persists until puberty but can extend into adulthood. A total of 26 patients were identified as having progressed to squamous cell carcinoma in the task force survey. The current standard is surgical therapy with a goal of maintaining an airway and doing no harm. A balance must be achieved between too frequent surgical intervention with its risk of stenosis, webbing, and anesthesia complications versus inadequate removal of tumor burden leading to airway obstruction and vocal disability. Overzealous surgical therapy can lead to significant scarring which can leave the patient with continued airway or vocal dysfunction once the disease goes into remission.
The posterior lateral nasal artery supplies the majority of the mucosa on the lateral nasal wall antibiotics vitamin d best purchase for nitrofurantoin, with major branches to the middle turbinate, inferior turbinate, and nasal floor. The posterior septal branch travels along the anterior wall of the sphenoid sinus just inferior to the sphenoid sinus ostium. This branch occasionally provides blood supply to the superior turbinate en route to the posterior part of the septum. Although anatomical definitions exist, a functional definition of location may be more practical when considering management. Any bleeding source that can be visualized with anterior rhinoscopy is considered anterior epistaxis. This triangle of large, thin-walled vessels contains rich anastamoses between the anterior ethmoidal artery, the nasal septal branch of the superior labial artery, and the posterior septal branch of the sphenopalatine artery. Woodruff nasopharyngeal plexus is a commonly cited location, consisting of a venous plexus along the lateral nasal wall at the posterior aspect of the inferior meatus. If anterior rhinoscopy does not reveal the location, attention is then directed posteriorly. This is best tolerated following adequate topical anesthesia and vasoconstriction. If posterior bleeding is profuse, performing a greater palatine block can assist in better endoscopic visualization by creating tamponade and vasospasm of the sphenopalatine artery. The greater palatine foramen can be palpated medial to the second molar, with injection of 1 to 2 mL of local anesthetic with epinephrine through a fine gauge needle bent 2. Additionally, the anesthetic effects of this injection can decrease patient discomfort if nasal packing is ultimately required. Determination of hemoglobin and hematocrit levels are essential with massive hemorrhage or suspected chronic blood loss. Likewise coagulation studies are helpful in identification coagulation disorders and essential for patients receiving anticoagulants. Nonsurgical management includes anterior septal pressure, topical vasoconstriction, chemical cautery, topical hemostatic agents, and nasal packing. Surgical options include electrocautery, bipolar diathermy, arterial ligation, and embolization. Management typically progresses from least invasive to more invasive and from nonsurgical to surgical. The least invasive management involves the application of pressure on the anterior nasal septum for 10 to 15 minutes. Education is a key component for this step as many patients will apply pressure over the nasal bones instead of the anterior septum. A useful adjunct procedure is the application of topical oxymetazoline into the nasal cavity to promote vasoconstriction. The combination of these two steps resolves the bleeding for the majority of patients. More recent studies suggest that bilateral cautery at the same visit may be safe, however large studies are lacking at this time. Broad application can lead to a large area of mucosal injury without any particular advantage in terms of hemostasis. Anterior epistaxis refractory to silver nitrate cautery can be managed with various topical hemostatic materials. These materials are commonly utilized for posterior epistaxis as well, as they can be applied under endoscopic guidance at the bedside. The addition of thrombin to these products also facilitates clot formation by converting fibrinogen to fibrin. Floseal has demonstrated favorable efficacy and patient tolerance when compared to nasal packing. Although the product is initially more costly, the avoidance of hospital and surgical costs have been reported in 80 to 89% of patients. Formal anterior and posterior nasal packing have traditionally been performed with layered gauze. More novel and simpler forms of packing include inflatable premanufactured balloon devices and polyvinyl acetate nasal packs. Regardless of the packing utilized, packing often carries higher morbidity, risks, and failure rates when compared to surgical measures. Traditionally, patients with nasal packs have been considered to be at risk for toxic shock syndrome; however, recent studies question the necessity of prophylactic antibiotics for this indication. Whereas embolization can be efficacious and cost effective, serious complications have been reported during these endovascular procedures. These include carotid artery intimal injury, soft tissue necrosis, facial paralysis, myocardial infarction, blindness, and stroke. Initial surgical management for posterior epistaxis consists of endoscopic examination with electrical cautery under general anesthesia. This approach allows the surgeon to locate specific bleeding sites and selectively cauterize these areas with bipolar diathermy or monopolar suction cautery. This can be highly effective as it applies the same principles utilized for anterior cautery to the otherwise more challenging and refractory posterior bleeding sites. Bipolar diathermy is preferred over monopolar cautery when the bleeding site is adjacent to critical nerves or vessels. This traditionally involved ligation of the internal maxillary, anterior ethmoidal, and posterior ethmoidal arteries. More recently, the efficacy of sphenopalatine artery ligation has been demonstrated and it has become the mainstay procedure for refractory posterior epistaxis.
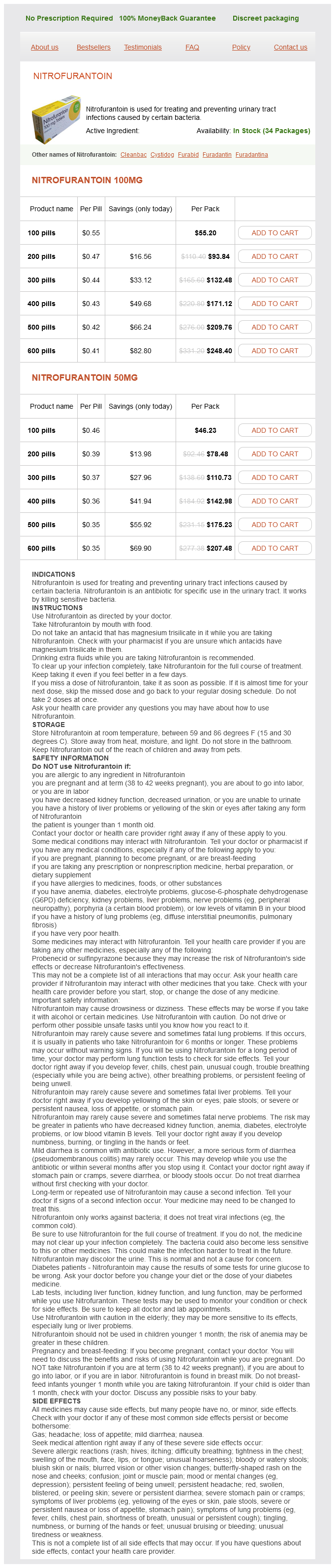
Nitrofurantoin Dosage and Price
Nitrofurantoin 100mg
- 100 pills - $55.20
- 200 pills - $93.84
- 300 pills - $132.48
- 400 pills - $171.12
- 500 pills - $209.76
- 600 pills - $248.40
Nitrofurantoin 50mg
- 100 pills - $46.23
- 200 pills - $78.48
- 300 pills - $110.73
- 400 pills - $142.98
- 500 pills - $175.23
- 600 pills - $207.48
Specifically should you take antibiotics for sinus infection order discount nitrofurantoin, they demonstrated that nose blowing (not sneezing or coughing) results in intranasal pressures that might be transiently elevated to 60 to 80 mm Hg. Furthermore, contrast material from the nasopharynx was propelled into the paranasal sinuses by this mechanism. In addition, the exudates in these patients may be harder to clear both due to increased viscosity and mucociliary dysfunction. In addition, viruses also have a substantial impact on neutrophil, macrophage, and lymphocyte function resulting in vulnerability to bacterial overgrowth by pathogens know to reside in the nose and nasopharynx as noted above. This constellation of symptoms is highly predictive of acute sinusitis of either viral or bacterial etiology. Onset with severe symptoms or signs of high fever (39¼C or 102¼F) and purulent nasal discharge or facial pain lasting for at least 3-4 consecutive days at the beginning of illness 3. Worsening symptoms or signs characterized by the new onset of fever, headache, or increase in nasal discharge following a typical viral upper respiratory infection that lasted five to six days and were initially improving ("double sickening")16 In patients with duration of symptoms longer than 10 days, only 60% will have a confirmed bacterial cause on sinus aspiration. The goal of therapy is to alleviate symptoms, shorten the duration of the illness, and prevent recurrence or sequelae of infection. The 2007 American Academy of OtolaryngologyHead and Neck Surgery Foundation Guidelines suggest that observation may be appropriate in a select population of patients who present with milder symptoms (mild pain and temperature <38. Failure to improve by seven days after diagnosis or worsening at any time is an indication to initiate antimicrobial therapy. Amoxicillin-clavulanate (500 mg/125 mg orally three times daily or 875 mg/125 mg orally twice daily) is recommended as empiric antimicrobial therapy in children and adults. Penicillinallergic patients may be treated with doxycycline (adults only) or a respiratory fluoroquinolone (children and adults). Patients with risk factors for increased microbial resistance should be treated with high-dose amoxicillin-clavulanate (2 g orally twice daily or 90 mg/kg/day orally twice daily). These risk factors include the following: geographic regions with high endemic rates (10%) of invasive penicillin-nonsusceptible S. Patients who fail to improve clinically after three to five days or worsen after 72 hours of empiric antimicrobial therapy should be evaluated for resistant pathogens, a noninfectious cause, structural abnormality, or other causes for treatment failure. It is important to note that these groups do not necessarily represent a rigid chronology of disease progression since they may be present in combination or evolve from one another. This classification system does, however, explain the signs and symptoms and helps to organize treatment plans as well as stratify outcomes. Signs of postseptal orbital involvement such as proptosis, visual impairment, and chemosis of the conjunctiva are not observed. Visual acuity, pupillary reaction, extraocular motility, and intraocular pressure are normal. Preseptal cellulitis is usually managed medically with systemic antibiotics and careful clinical observation. Sinusitis is the major cause of orbital cellulitis, with studies reporting 96 to 100% of hospitalized patients with orbital cellulitis having concurrent sinusitis. In addition to these signs, patients with orbital cellulitis often have more systemic toxicity, such as fever, leukocytosis, and elevated levels of C-reactive protein than patients with preseptal cellulitis. All patients with suspected orbital cellulitis should be imaged and treated with intravenous antibiotic therapy and nasal decongestants. Patients who develop a decrease in visual acuity, an afferent pupillary defect, worsening extraocular muscle function, or failure to improve in 48 to 72 hours should undergo surgical sinus drainage with culture. The patient underwent left endoscopic sinus surgery and left anterior orbitotomy via inferior transconjunctival and medial transcaruncular approaches to drain the abscesses. The abscess develops when infection breaks through the lamina papyracea or through the foramina of the anterior or posterior ethmoidal neurovascular bundles. The periorbita is loosely adherent along the medial orbital wall, which may permit abscess contents to migrate superiorly, inferiorly, or posteriorly within the subperiosteal space. Several studies have reported good response to medical management alone in select cases. Orbital apex syndrome, consists of unilateral ptosis, proptosis, vision loss, internal and external ophthalmoplegia (ie, palsy of the pupillary and extraocular muscles), and cranial nerve V1 anesthesia, is also indicative of orbital abscess. The clinical presentation may vary depending upon the size and location of the orbital abscess, duration of the infection, virulence of the microorganisms, and host factors. Therefore, any clinical sign or symptom suggestive of orbital abscess warrants immediate imaging and intensive antibiotic therapy. Early surgical intervention is necessary when the presence of an orbital abscess is confirmed. Patel and colleagues reported a nine-year-old boy with lacrimal gland abscess thought to be caused by spread of infection from the paranasal sinuses. Further surgical exploration of the orbit revealed an abscess of the lacrimal gland, which was incised and drained, resulting in complete recovery. Subsequent incision and drainage of the lacrimal gland abscess led to a complete resolution of the infection. Although abscess formation of the lacrimal gland rarely complicates rhinosinusitis, it should be included in the differential diagnosis when the symptoms fail to resolve after appropriate therapy, especially when there is associated enlargement and tenderness of the lacrimal gland and predominant swelling of the lateral part of the upper eyelid. Each cavernous sinus is broken up by trabeculae into many venous cavernous spaces through which the third and fourth cranial nerves and the first two divisions of the fifth cranial nerve, sixth cranial nerve, and internal carotid artery pass. It is connected by an extensive valveless venous system to the nose, adjacent face, nasopharynx, pharynx, orbit, and paranasal sinuses allowing retrograde spread of infection from any of these areas. Cavernous sinus thrombosis carries a serious morbidity, often with bilateral blindness and mortality.