Nizagara
General Information about Nizagara
Nizagara is also known for its fast onset of action. Unlike some other ED medication that will take as much as an hour to start working, Nizagara begins working in simply 30 minutes to 1 hour. This allows for extra spontaneity and flexibility in the timing of sexual exercise. The effects of Nizagara can last for about 4 hours, giving males enough time to engage in sexual exercise without the need for repeated doses.
In conclusion, Nizagara is a protected and effective oral treatment for the treatment of male impotence. It has a proven observe document, minimal unwanted effects, and quick onset of motion. It is a well-liked selection amongst males with ED and has helped countless males regain their confidence and improve their sexual relationships. However, it is crucial to take it as prescribed and beneath the supervision of a healthcare skilled to ensure the best results.
One of the biggest advantages of Nizagara is its security monitor report. It has been on the market for over a decade and has been used by tens of millions of men worldwide. It has undergone rigorous testing and has been approved by the Food and Drug Administration (FDA). Nizagara is manufactured by a reputable pharmaceutical company, ensuring high-quality and constant results.
Another good factor about Nizagara is its minimal side effects. Some males might experience gentle headaches, dizziness, or flushing after taking the treatment, but these unwanted aspect effects are sometimes short-lived and not severe. Nizagara has been proven to be well-tolerated by most males and does not trigger any long-term harm to the physique.
Male impotence, also called erectile dysfunction, is a typical issue faced by many men around the world. It is the inability to realize or maintain an erection throughout sexual exercise. This can result in frustration, embarrassment, and might greatly have an effect on a man's vanity and relationships. Fortunately, there are oral medications like Nizagara that may help with this drawback.
It is essential to notice that Nizagara is just effective in the presence of sexual stimulation. It is not an aphrodisiac and won't increase a person's intercourse drive. It can be not a remedy for ED, however rather a temporary answer to assist males achieve and preserve an erection during sexual exercise.
In addition to treating male impotence, Nizagara has additionally been found to be effective in treating other circumstances corresponding to pulmonary arterial hypertension and altitude sickness. This makes it a versatile drug with a quantity of uses.
As with any medicine, it is important to seek the guidance of with a doctor before taking Nizagara. It may work together with certain drugs or medical situations, so it is important to disclose one's full medical historical past.
Nizagara is a prescription drug used for the remedy of male impotence. It belongs to a category of drugs referred to as phosphodiesterase sort 5 (PDE5) inhibitors. It works by rising blood flow to the penis, thus bettering a man's ability to get and preserve an erection. Nizagara accommodates the active ingredient sildenafil citrate, the same ingredient found within the popular ED drug Viagra.
Distinguishing serous cystadenomas from multiple cysts may sometimes be difficult erectile dysfunction levitra generic nizagara 100 mg fast delivery, which is, however, not clinically important unless they cause symptoms. Axial computed tomography images through the head (A) and body-tail (B) of the pancreas reveal multiple thin-walled cystic lesions in the pancreas (arrows) and kidneys (arrowheads). Incidental note is made of a complex cystic lesion in the right kidney (large arrow, A), which was proved at biopsy to be renal cell carcinoma. Contrast-enhanced axial T1- (A) and T2-weighted fat-suppressed (B) gradient recalled echo magnetic resonance imaging reveals multiple cysts in the pancreas (arrows) and kidneys (arrowheads). Abdominal ultrasonography, although an attractive screening tool owing to low cost and the absence of ionizing radiation, is insensitive for isolated pancreatic cysts and small renal and pancreatic tumors. Classic Signs: Von Hippel-Lindau Disease · Multiple cysts in pancreas and kidneys · Solid lesions of pancreas and kidneys What the Referring Physician Needs to Know: Von Hippel-Lindau Disease · Early screening can result in timely recognition of life-threatening manifestations. Fischer G, Spengler U, Neubrand M, et al: Isolated tuberculosis of the pancreas masquerading as a pancreatic mass. Takhtani D, Gupta S, Suman K, et al: Radiology of pancreatic tuberculosis: a report of three cases. Itaba S, Yoshinaga S, Nakamura K, et al: Endoscopic ultrasound-guided fine-needle aspiration for the diagnosis of peripancreatic tuberculous lymphadenitis. Iwai T, Kida M, Kida Y, et al: Biliary tuberculosis causing cicatricial stenosis after oral antituberculosis therapy. Nishimura R, Takakuwa T, Hoshida Y, et al: Primary pancreatic lymphoma: clinicopathological analysis of 19 cases from Japan and review of the literature. Arcari A, Anselmi E, Bernuzzi P, et al: Primary pancreatic lymphoma: a report of five cases. Matsueda K, Yamamoto H, Doi I: An autopsy case of granulocytic sarcoma of the porta hepatis causing obstructive jaundice. Ramanathan S, Prakash M, Khandelwal N: Concurrent pancreatic and renal leukemic cell infiltration. Muranaka T, Teshima K, Honda H, et al: Computed tomography and histologic appearance of pancreatic metastases from distant sources. Swensen T, Osnes M, Serck-Hanssen A: Endoscopic retrograde cholangiopancreatography in primary and secondary tumours of the pancreas. Aynsley-Green A, Hussain K, Hall J, et al: Practical management of hyperinsulinism in infancy. Ferrario C, Stoll D, Boubaker A, et al: Diffuse nesidioblastosis with hypoglycemia mimicking an insulinoma: a case report. Elli L, Buscarini E, Portugalli V, et al: Pancreatic involvement in von Hippel-Lindau disease: report of two cases and review of the literature. The role of imaging is to identify a bile duct obstruction and define its level and cause. Cholangiographic and cross-sectional modalities provide complementary information, and both are required to investigate biliary dilatation. The pattern of biliary dilatation depends on the cause and level of abnormality within the biliary tree. The biliary tract may be involved diffusely or focally, or dilatation may be multifocal. Peripheral cholangiocarcinoma may cause segmental dilatation of the intrahepatic bile ducts. Malignant and benign neoplasms that can cause bile duct dilatation and choledochal cysts are discussed separately. In Western society, cholesterol stones are the most common type; in Southeast Asia, pigment stones are more common. This precipitates hepatolithiasis and can be complicated by recurrent pyogenic cholangitis. The most common malignant cause of bile duct dilatation is pancreatic adenocarcinoma, followed by cholangiocarcinoma. The incidence of cholangiocarcinoma is at least four times less than pancreatic carcinoma. Thus, malignant and benign causes of biliary dilatation may coexist and differentiating one from the other may be problematic. Clinical Presentation All causes of bile duct dilatation lead to cholestatic symptoms once obstruction becomes severe enough. The classic symptoms and signs are jaundice, pruritus, pale stools, and dark urine. Typically, choledocholithiasis is associated with acute intermittent right upper quadrant pain and transient jaundice. Malignant causes of bile duct obstruction, such as carcinoma of the head of the pancreas, are often initially painless or manifest as dull pain, and jaundice is progressive. Occasionally, patients with bile duct strictures may develop manifestations of chronic cholestasis: xanthomas, anorexia, nausea, vomiting, weight loss, and deficiencies of calcium and fat-soluble vitamins. Patients with biliary obstruction typically have elevated serum alkaline phosphatase and gamma-glutamyl transpeptidase levels. In more severe cases of biliary obstruction, total and conjugated bilirubin values are increased. A, magnetic resonance cholangiopancreatography (maximal intensity projection) image demonstrates marked intrahepatic and extrahepatic duct dilatation to the level of the pancreas, which shows as high T2 signal intensity and is amorphous. B, Postcontrast axial T1-weighted image shows a nonenhancing necrotic mass replacing most of the pancreas and compressing the common bile duct (arrow). A 66-year-old woman presented with weight loss and elevated alkaline phosphatase level. A and B, Coronal reformatted computed tomography images show mild compression of the bile duct (arrows) by a 4. Coronal single-shot fast spin echo (A), postcontrast axial flexible appearance modeling environment (B), and axial T2-weighted fast spin echo (C) magnetic resonance images show a large cystic lesion with enhancing papillary projections (arrows, A and B), causing mild intrahepatic bile duct dilatation (arrow, C).
In patients with peptic ulcer disease impotence 25 years old nizagara 25 mg order otc, failure of gastroduodenal mucosal mechanisms secondary to Helicobacter pylori infection, nonsteroidal antiinflammatory drug use, and hypersecretory states, among others, results in a defect in the muscularis mucosa. In diverticulitis of the small bowel or colon, once the mucosalined outpouching through the bowel wall is obstructed, distention results secondary to ongoing secretion of mucus and bacterial overgrowth. Vascular compromise of these mucosal outpouchings may occur, leading to perforation. Similar to the pathophysiology of perforated diverticulitis, appendicitis results from obstruction of the appendiceal lumen with subsequent distention from mucosal secretions. Capillary perfusion pressures are outstripped, and venous and lymphatic drainage is obstructed. The influx of bacteria into the appendiceal wall as well as the decreasing arterial flow and tissue necrosis lead to appendiceal perforation. In patients with colonic perforation secondary to colorectal carcinoma, the perforation may occur proximal to the tumor, related to obstruction and distention, or occur directly at the site of the tumor. In cases of perforation related to obstruction, the pathophysiology is similar to that of the aforementioned examples of increasing luminal distention and decreasing venous return followed by decreasing arterial inflow, resulting in tissue necrosis and loss of mural integrity. In cases of perforation directly at the site of the tumor, transmural tumor invasion and necrosis are underlying mechanisms resulting in loss of mural integrity. B, Lateral chest radiograph reveals significant free intraperitoneal air, as evidenced by the lucency beneath the diaphragms (arrows). C, Axial computed tomography image confirms the presence of significant free intraperitoneal air (arrows). The patient was diagnosed with perforated diverticulitis at operative exploration. In cases of hollow viscus perforation resulting from gastrointestinal obstruction, the pathophysiology involves a component of ischemia. Therefore, in addition to extraluminal gas and dilated loops of bowel, secondary signs of ischemia may be seen. These include pneumatosis intestinalis, air within the portal and mesenteric veins, and decreased enhancement of the affected bowel. The patient was found to have a perforated gastric ulcer at operative exploration. Finally, in patients with malignancy as the underlying cause of the hollow viscus perforation, direct visualization of the mass lesion is typically achieved. The patient was successfully treated conservatively for perforated diverticulitis. If esophageal rupture is suspected, anteroposterior and lateral chest radiographs are commonly acquired. If an intra-abdominal perforation is suspected, supine and upright abdominal radiographs are acquired, possibly with an upright anteroposterior radiograph of the chest for the evaluation of pneumoperitoneum. If there is evidence of hollow viscus perforation based on the initial plain radiographic findings, depending on the clinical status of the patient, the surgical team may decide to proceed directly to operative exploration. However, in a subgroup of patients with perforated diverticulitis, when there is no evidence of gross free intraperitoneal air and fluid, conservative medical management, including intravenous antibiotics, may be indicated. Also, in selected patients with perforated appendicitis, medical management including intravenous antibiotics may be employed before definitive operative management. In patients with hollow viscus perforation managed conservatively, radiology may be a critical facet of nonoperative management via the use of image-guided percutaneous placement of drainage catheters to manage intra-abdominal fluid collections. The preferred treatment in patients with esophageal perforation has traditionally been surgical intervention, although less invasive interventions are evolving. Finally, in patients with perforation secondary to underlying malignancy, surgical intervention with resection of the underlying mass lesion is performed. Differential Diagnosis the clinical signs and symptoms of hollow viscus perforation can be nonspecific. Differential diagnostic considerations include other causes of peritonitis, such as spontaneous bacterial peritonitis; systemic infections involving the peritoneum, such as tuberculosis; and sterile irritants of the peritoneal cavity, such as blood, bile, and pancreatic secretions. In addition to perforation of a hollow viscus, other causes of extraluminal air include iatrogenic causes such as recent surgery. Dissection of air from the thorax in cases of pneumothorax or pneumomediastinum are differential considerations in cases of extraluminal, intra-abdominal gas. In cases of pneumoperitoneum related to prior surgery, one should expect appropriate resolution during the postoperative period. Marincek B: Nontraumatic abdominal emergencies: acute abdominal pain-diagnostic strategies. Espinoza R, Rodríguez A: Traumatic and nontraumatic perforation of hollow viscera. Mäkelä J, Kiviniemi H, Laitinen S: Prevalence of perforated sigmoid diverticulitis is increasing. De Lutio di Castelguidone E, Pinto A, Merola S, et al: Role of spiral and multislice computed tomography in the evaluation of traumatic and spontaneous oesophageal perforation: our experience. Kirshtein B, Bayme M, Mayer T, et al: Laparoscopic treatment of gastroduodenal perforations: comparison with conventional surgery. Pathophysiology the pathophysiology of gastrointestinal hemorrhage depends on the underlying cause. Peptic ulcer disease results in a defect in the gastroduodenal mucosa with eventual exposure and damage to the underlying arteries, including arteritis, aneurysmal dilatation, and eventual rupture and hemorrhage. In patients with varices, increasing hepatic venous pressure results in enlarged varices and the increased risk for rupture and hemorrhage. Diverticular hemorrhage results from rupture of the vasa recta at the dome of the diverticulum. Angiodysplasia is typically located within the lower gastrointestinal tract, specifically the right colon. Although the pathophysiology is incompletely understood, angiodysplastic lesions are thought to be acquired degenerative lesions.
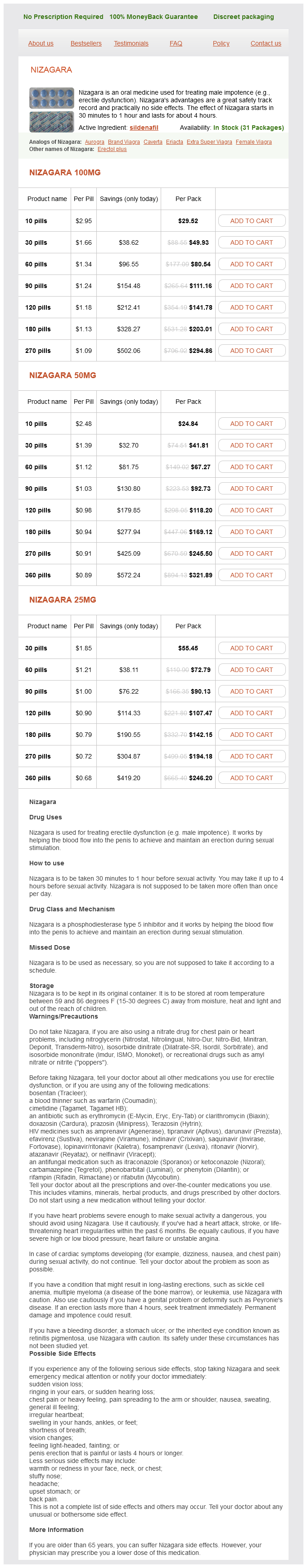
Nizagara Dosage and Price
Nizagara 100mg
- 10 pills - $29.52
- 30 pills - $49.93
- 60 pills - $80.54
- 90 pills - $111.16
- 120 pills - $141.78
- 180 pills - $203.01
- 270 pills - $294.86
Nizagara 50mg
- 10 pills - $24.84
- 30 pills - $41.81
- 60 pills - $67.27
- 90 pills - $92.73
- 120 pills - $118.20
- 180 pills - $169.12
- 270 pills - $245.50
- 360 pills - $321.89
Nizagara 25mg
- 30 pills - $55.45
- 60 pills - $72.79
- 90 pills - $90.13
- 120 pills - $107.47
- 180 pills - $142.15
- 270 pills - $194.18
- 360 pills - $246.20
Multiple antiviral medications impotence at age 70 cheap 100 mg nizagara with mastercard, such as zidovudine, efavirenz, didanosine, and protease inhibitors are known to cause acute and chronic pancreatitis, some by inducing hyperlipidemia. Pancreatic involvement may vary from asymptomatic to fulminant pancreatitis and is most commonly part of a disseminated disease process. The involved gland is hypointense on T1-weighted images, hyperintense on T2-weighted images, and indistinguishable from that of other forms of pancreatitis. Classic Signs: Acquired Immunodeficiency Syndrome · Enlarged boggy pancreas with cytomegalovirus infection · Hemorrhagic necrosis with herpes simplex infection Treatment Medical management includes supportive therapy and treatment of the underlying disease process and inciting cause. Because of the absence of a capsule, adjacent lymph node involvement may be difficult to distinguish from pancreatic infiltration. Special stains for mycobacteria, fungi, and viral inclusions after biopsy and serologic tests are required for diagnosis. The pancreas is diffusely swollen and hypodense (arrows) on this axial computed tomography image. Imaging the morphologic manifestation of pancreatic lymphoma on imaging may be in the form of a localized, well-circumscribed Document téléchargé de ClinicalKey. Primary pancreatic lymphoma may sometimes be indistinguishable from primary pancreatic adenocarcinoma and further evaluation with biopsy is warranted. On ultrasonography, pancreatic involvement, whether focal or diffuse, appears homogeneously hypoechoic. Typically, peripancreatic vasculature is engulfed by pancreatic lymphoma and patency can be evaluated using color Doppler imaging. On endoscopic ultrasonography, the wall of the common bile duct appears hyperechoic, contrasting to the adjacent hypoechoic pancreatic parenchyma. The lesions reveal poor homogeneous enhancement and occasional heterogeneous enhancement may be seen after contrast administration. However, clinical presentation is never similar to acute pancreatitis and is disproportionate to the extensive pancreatic involvement, even in the presence of abnormal laboratory parameters. Invasion of the retroperitoneum, upper abdominal organs, and gastrointestinal tract and the presence of mesenteric or retroperitoneal lymphadenopathy extending below the renal veins are also signs favoring lymphoma. Often used as a problemsolving tool, the diffusely involved gland appears hypointense on T1-weighted imaging and hypointense or hyperintense on T2-weighted imaging, with mild to moderate homogeneous enhancement. Peripancreatic lymphadenopathy has signal intensity similar to that of the pancreas. This is in contrast to carcinoma, which causes stenosis with moderate to severe upstream dilatation. Although biliary obstruction may be seen, jaundice occurs in fewer than half of the cases of pancreatic lymphoma. Classic Signs: Lymphoma · · · · · · Abdominal pain and mass without associated jaundice Predominantly homogeneous Infiltration of peripancreatic fat Lack of pancreatic ductal dilatation Lack of calcification and necrosis in untreated cases Retroperitoneal lymphadenopathy extending below renal veins · Engulfment rather than stenosis of vessels Differential Diagnosis Clinical presentation can be overlapping with other pancreatic neoplasms, but absence of jaundice is an important diagnostic clue to differentiate lymphoma from carcinoma. Pancreatic lymphoma also can manifest with diffuse enlargement of the gland with peripancreatic fat stranding, findings indistinguishable from those of acute pancreatitis. Imaging plays an important role in the diagnosis and staging of pancreatic lymphoma. Treatment and prognosis of lymphoma significantly differ from those of pancreatic carcinoma, which is the main differential diagnosis. Surgery is reserved for cases in which the diagnosis cannot be established by less invasive methods. Relief of biliary obstruction can be achieved by endoscopic or percutaneous stent insertion or with surgical procedures such as choledochojejunostomy, tumor debulking, or a palliative Whipple procedure, which is no longer performed for this indication. Axial computed tomography image reveals a diffusely enlarged and predominantly hypodense pancreas (arrows) with mild heterogeneous enhancement. Classic Sign: Leukemia · Overlapping features with lymphoma · Often lacks bulky peripancreatic lymphadenopathy involvement with pathologic evaluation of tissue facilitates appropriate diagnosis. What the Referring Physician Needs to Know: Leukemia · Because extramedullary involvement of leukemia is known to be highly responsive to systemic antileukemic therapy, consideration of this rare diagnosis is important for management, especially to avoid unnecessary surgery. Extramedullary myeloid lesions are more common and are called granulocytic sarcomas. Granulocytic sarcomas can involve virtually any organ system but has particular predilection for soft tissues, bones, skin, lymph nodes, and periosteum. Although patients may be asymptomatic, cholestatic jaundice and pancreatitis may occur. Imaging Three morphologic patterns of pancreatic leukemia have been described: (1) well or ill-circumscribed focal form, (2) diffuse infiltrative form, and (3) combination of nodular and diffuse infiltrative form. Leukemic involvement of the pancreas is by and large indistinguishable from that of pancreatic lymphoma on imaging. Likewise, the common bile duct may be involved, but jaundice is not a common feature. The involved gland appears hypointense on T1-weighted images and hyperintense on T2-weighted images. Differential Diagnosis Clinical features and systemic manifestations are a clue to diagnosis. Prevalence and Epidemiology Pancreatic carcinoma appears as a focal mass, most commonly in the head of the pancreas. Clinical Presentation Clinical features are similar to those associated with focal involvement of the gland (see corresponding chapter on pancreatic carcinoma).