Nootropil
General Information about Nootropil
The traditional therapy for vestibular nystagmus contains vestibular rehabilitation workouts, medications, and in excessive cases, surgical procedures. However, researchers have been exploring the consequences of Nootropil on vestibular nystagmus, and the outcomes have been promising. Studies have shown that Nootropil can effectively cut back the period and depth of nystagmus in patients.
It can be value noting that Nootropil has been discovered to have minimal unwanted effects, making it a secure choice for those affected by vestibular nystagmus. Most widespread unwanted side effects of Nootropil embody headaches, dizziness, and nausea, which are normally gentle and disappear because the physique adjusts to the drug. Additionally, not like other medications used to treat nystagmus, Nootropil does not trigger drowsiness, making it appropriate for long-term use.
Apart from its effect on neurotransmitters, Nootropil has also been discovered to have a neuroprotective effect. This signifies that it can defend nerve cells from injury and even promote their growth and repair. This could probably be significantly useful in circumstances the place vestibular nystagmus is brought on by nerve damage. By defending and repairing broken nerve cells, Nootropil could contribute to reducing the duration and severity of nystagmus.
Firstly, it may be very important understand what vestibular nystagmus is and the way it impacts an individual. It is a condition that causes fast, involuntary eye actions, often as a outcome of dysfunction within the vestibular system – the a half of the inner ear liable for sustaining balance and coordination. These eye actions can be horizontal, vertical, or rotary and might trigger dizziness, vertigo, and disorientation. Vestibular nystagmus could be attributable to a variety of components corresponding to head trauma, internal ear infections, treatment unwanted effects, and extra. It can severely influence a person's high quality of life and ability to perform daily activities.
Moreover, the use of Nootropil in the remedy of vestibular nystagmus has been found to have a constructive impact on the overall high quality of life of patients. In addition to its effects on lowering nystagmus, Nootropil has also been proven to improve cognitive operate, memory, and a focus. This implies that patients not only experience a discount in nystagmus, however in addition they benefit from improved cognitive skills.
In conclusion, the invention of Nootropil's effectiveness in decreasing the duration of vestibular nystagmus is a significant development in the treatment of this situation. With its minimal side effects and extra advantages on cognitive function, it proves to be a beneficial choice for these suffering from nystagmus. However, it is important to consult a healthcare professional before starting any medication, as they might advise on the suitable dosage and length of therapy. With further research and understanding of its mechanisms, Nootropil has the potential to play a crucial position in managing vestibular nystagmus and bettering the quality of life for patients.
Nootropil is a widely used nootropic drug that has been gaining attention for its ability to enhance cognitive function and reminiscence. However, there's a lesser-known advantage of this drug that has been studied and confirmed – its capability to reduce the length of vestibular nystagmus. This might come as a shock to many, as historically, Nootropil is not recognized for its results on the vestibular system. Let us discover this fascinating discovery and perceive what it means for individuals who suffer from vestibular nystagmus.
The exact mechanism of how Nootropil works to reduce nystagmus just isn't absolutely understood yet. However, it's believed that the drug's action on neurotransmitters, especially acetylcholine, plays a crucial role. Nootropil has been found to extend acetylcholine levels in the brain, which is answerable for communication between nerve cells. This increase in acetylcholine might result in improved communication and coordination between the brain and the vestibular system, leading to a lowered period of nystagmus.
Impact of smoking cessation before resection of lung cancer: A society of thoracic surgeons general thoracic surgery database study oxygenating treatment nootropil 800 mg free shipping. Effect of preoperative smoking cessation interventions on postoperative complications. Stopping smoking shortly before surgery and postoperative complications: A systematic review and meta-analysis. Smoking cessation reduces postoperative complications: A systematic review and meta-analysis. Perioperative rehabilitation and physiotherapy for lung cancer patients with chronic obstructive pulmonary disease. The effects of preoperative short-term intense physical therapy in lung cancer patients: A randomized controlled trial. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing one-lung ventilation. Mean pulmonary artery pressure under thoracotomy as an indicator of safety for lung resection. Transesophageal echocardiography and the intraoperative diagnosis of left atrial invasion by carcinoid tumor. Transesophageal echocardiographic detection of left atrial involvement in a lung tumor. Transesophageal echocardiography for the intraoperative evaluation of a large anterior mediastinal mass. Reduced cerebral oxygen saturation measured by absolute cerebral oximetry during thoracic surgery correlates with postoperative complications. Cerebral desaturation during single-lung ventilation is negatively correlated with preoperative respiratory functions. Minimally invasive measurement of cardiac output during surgery and critical care: a meta-analysis of accuracy and precision. A comparison of three methods of hemoglobin monitoring in patients undergoing spine surgery. A comparison of lidocaine and bupivacaine digital nerve blocks on noninvasive continuous hemoglobin monitoring in a randomized trial in volunteers. Variation in the arterial to end-tidal Pco2 difference during one-lung thoracic anaesthesia. Recommendations for airway control and difficult management in thoracic anesthesia: Are we ready for the challenge Tracheal width and left double-lumen tube size: a formula to estimate left-bronchial width. Comparison of VivaSight double-lumen tube with a conventional double-lumen tube in adult patients undergoing videoassisted thoracoscopic surgery. Rupture of the left main-stem bronchus by the tracheal portion of a double-lumen endobronchial tube. Tracheal rupture following the insertion of a disposable double-lumen endotracheal tube. Airway injuries after one-lung ventilation: A comparison between double-lumen tube and endobronchial blocker: a randomized, prospective, controlled trial. A comparison of the efficacy and adverse effects of double-lumen endobronchial tubes and bronchial blockers in thoracic surgery: a systematic review and meta-analysis of randomized controlled trials. One-lung ventilation in a patient with a tracheostomy and severe tracheobronchial disease. Selective bronchial intubation with the Univent system in patients with a tracheostomy. A comparison of a left-sided Broncho-Cath with the torque control blocker Univent and the wire-guided blocker. Choosing a lung isolation device for thoracic surgery: A randomized trial of three bronchial blockers versus doublelumen tubes. The effects of endobronchial cuff inflation on double-lumen endobronchial tube movement after lateral decubitus positioning. The use of air in the inspired gas mixture during two-lung ventilation delays lung collapse during one-lung ventilation. Effects of different tidal volumes for one-lung ventilation on oxygenation with open chest condition and surgical manipulation: A randomised cross-over trial. The effects of different ventilatory settings on pulmonary and systemic inflammatory responses during major surgery. Effects of mechanical ventilation on release of cytokines into systemic circulation in patients with normal pulmonary function. Intraoperative tidal volume as a risk factor for respiratory failure after pneumonectomy. Comparison of volume control with pressure control ventilation during one-lung anaesthesia. Pressure-controlled versus volume-controlled ventilation during one-lung ventilation for thoracic surgery. Effects of ventilatory mode during onelung ventilation on intraoperative and postoperative arterial oxygenation in thoracic surgery. The effect of one-lung ventilation upon pulmonary inflammatory responses during lung resection. Effect of therapeutic hypercapnia on inflammatory responses to one-lung ventilation in lobectomy patients. Effectiveness of low levels of nonventilated lung continuous positive airway pressure in improving arterial oxygenation during one-lung ventilation. Maintenance of oxygenation during one-lung ventilation: effect of intermittent reinflation of the collapsed lung with oxygen.
In severe cases medicine plies effective 800 mg nootropil, or if the fetus is mature at the onset of symptoms, prompt delivery is indicated, usually by cesarean section. Anesthesia for delivery of patients with placenta previa may be with neuraxial anesthesia, provided the mother is hemodynamically stable. Past 2880 recommendations for general anesthesia to provide "more control" are not supported by the literature, as there is no difference in complications between the two techniques, except that general anesthesia is associated with greater blood loss and greater need for transfusion. An emergency hysterectomy may be required if there is severe hemorrhage, even after delivery of the placenta, because of uterine atony. The risk of severe hemorrhage after attempted removal of the placenta is greatly increased in patients who have undergone prior uterine surgery, including cesarean delivery. This is related to a higher incidence of placenta accreta, which results from the penetration of myometrium by placental villi. The risk of placenta accreta in women with previa increases from 3% in primary cesarean section to 61% in quaternary section. When placenta accreta is suspected or known, delivery is usually scheduled at 36 to 37 weeks of gestation via cesarean hysterectomy. Some institutions may use occlusive balloon catheters placed in the internal iliac arteries prior to surgical delivery. In the face of bleeding with either placenta previa or accreta, when maintenance of fertility is desired, arterial embolization or ligation, uterine compression sutures, and/or methotrexate therapy may be attempted to avoid hysterectomy. Complications include Couvelaire uterus (when extravasated blood dissects between the myometrial fibers), renal failure, disseminated intravascular coagulation, and anterior pituitary necrosis (Sheehan syndrome). The diagnosis of abruptio placentae is based on the presence of uterine tenderness and hypertonus as well as vaginal bleeding of dark, clotted blood. Bleeding may be concealed if the placental margins have remained attached to the uterine wall. If the blood loss is severe (>2 L), there may be changes in the maternal blood pressure and pulse rate, indicative of hypovolemia. Fetal movement may increase during acute hypoxia or decrease if hypoxia is gradual. Management of abruption depends on presentation, gestational age, and the degree of compromise. Management of milder cases of abruption includes artificial rupture of 2881 amniotic membranes and oxytocin augmentation of labor, if required. In the presence of nonreassuring fetal status, an emergency cesarean delivery may be performed. If fetal death has occurred, usually with severe abruption, vaginal delivery is reasonable if the mother is stable. Postpartum hemorrhage is usually defined as blood loss greater than 500 mL after vaginal delivery or greater than 1,000 mL after cesarean section. The incidence of postpartum hemorrhage is increasing in the United States, mainly due to an increase in uterine atony. Treatment of postpartum hemorrhage may require aggressive uterotonic therapy for atony, intrauterine balloon tamponade or evacuation of the uterus for retained products of conception (Table 41-2). If there is a need for dilation and curettage, the anesthesiologist may be asked to provide uterine relaxation. This can be accomplished with volatile agents if the patient is under general anesthesia or with intravenous nitroglycerin if regional anesthesia or general anesthesia is used. The choice of anesthetic technique depends on the anticipated duration of surgery, maternal condition and volume status, the potential for coagulopathy, and urgency of the procedure. General anesthesia is indicated in the presence of uncontrolled hemorrhage and/or severe coagulation abnormalities. Neuraxial anesthesia, usually continuous epidural anesthesia, has been successfully used for hysterectomy in planned, controlled situations. A saddle block is an option for anesthesia when dilation and curettage for treatment of postpartum hemorrhage is indicated and the patient is hemodynamically stable. All of these tasks may be challenging in the parturient and consideration should be given to performing them in advance of hemorrhage when hemorrhage is anticipated. Prompt transfusion of blood component therapy is crucial for replacement of blood loss, maintenance of tissue oxygenation, and correction of coagulopathy. In recent years, transfusion rates for postpartum hemorrhage have increased 92% in the United States. Early administration of platelets and cryoprecipitate has also become common in hemostatic resuscitation protocols for major traumatic hemorrhage, and crystalloid and colloid administration is minimized in favor of blood products (see Chapter 53). Hypothermia, metabolic acidosis, and coagulopathy commonly occur in traumatic and obstetric hemorrhage. Because of these commonalities, it has become common to extend these successful transfusion practices from the trauma literature to obstetric practice. Transfusion of cryoprecipitate or better, fibrinogen concentrate, should be incorporated early in obstetric hemorrhage because decreased fibrinogen levels strongly correlate with increased severity of postpartum hemorrhage. Other options are available to decrease transfusion requirements and reduce blood loss. Intraoperative cell salvage, formerly shunned because of concerns about the risk of amniotic fluid contamination of red cells, has been implemented safely during cesarean section in many centers. The antifibrinolytic drug tranexamic acid has been shown to decrease bleeding in both elective cesarean section and postpartum hemorrhage and is recommended for early use in resuscitation by a European task force131; however, further studies are needed to confirm its safety. Medical and surgical advancements have changed the types of cardiac problems seen in pregnancy. Patients with congenital heart disease are reaching childbearing age, and the number of patients with rheumatic heart disease has declined. Older parturients may present with aortic stenosis and insufficiency associated with a bicuspid aortic valve.
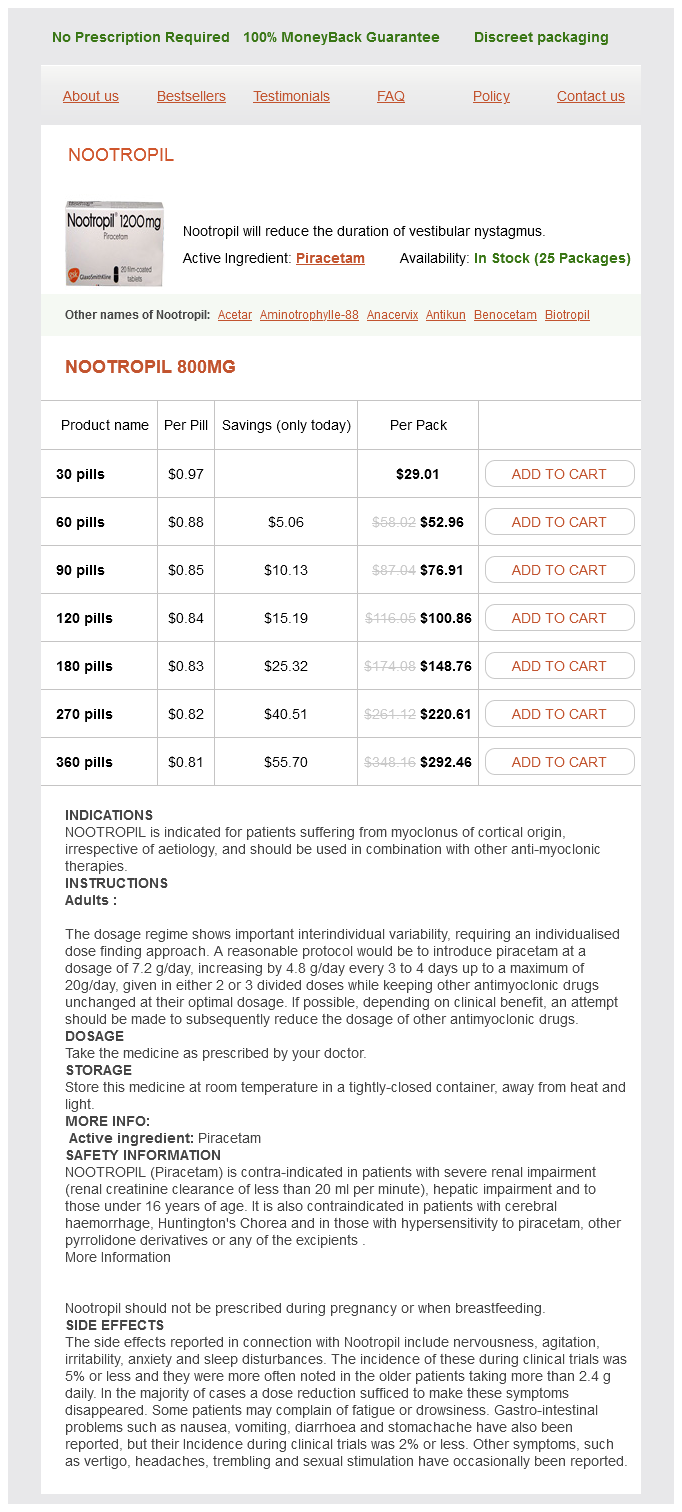
Nootropil Dosage and Price
Nootropil 800mg
- 30 pills - $29.01
- 60 pills - $52.96
- 90 pills - $76.91
- 120 pills - $100.86
- 180 pills - $148.76
- 270 pills - $220.61
- 360 pills - $292.46
Their respective 2/1 binding ratios are 220:1 for clonidine versus 1 medicine 8 discogs generic nootropil 800 mg mastercard,620:1 for dexmedetomidine. Analgesia is mediated supraspinally (locus coeruleus), spinally (substantia gelatinosa), and peripherally. Clonidine can be administered orally, transdermally, intravenously, perineurally, and neuraxially for perioperative pain management. Side effects from clonidine include sedation, hypotension, and bradycardia if the dose exceeds 150 g. Dexmedetomidine is a potent and highly selective 2-adrenoreceptor agonist which demonstrates cardioprotective, neuroprotective, and renoprotective effects against hypoxic/ischemic injury. The drug does not decrease gut motility and prevents postoperative nausea and vomiting and shivering. It provides adequate sedation without significant respiratory depression and analgesia that is opioid sparing. Likewise, because the gabapentinoids can prevent the establishment of surgery-induced central sensitization, these drugs may play a role in preventing the transition from acute pain to chronic pain. As an added bonus, there is a decreased incidence of postoperative delirium, vomiting, pruritus, and urinary retention associated with the perioperative use of these drugs, probably secondary to their opioidsparing effects. Common side effects associated with these drugs include sedation, headache, dizziness, and visual disturbances. The antinociceptive mechanism of action of the gabapentinoids has two aspects: modulation of the calcium-induced release of glutamate centrally in the dorsal horn, and activation of descending noradrenergic pathways in the spinal cord and brain. The gastrointestinal absorption of gabapentin occurs only in the duodenum through a saturable transport system resulting in bioavailability that decreases with increasing doses. Consequently, increased doses of gabapentin result in incrementally smaller increases in plasma drug concentration. Gabapentin oral absorption is significantly impaired by antacids, including bicitra. Although the multimodal approach to perioperative pain management is to be applauded, we need to display caution when combining multiple pharmaceutical agents with different mechanisms of action ("poly-pharmacy") for fear of eliciting unacceptable side effects. The ideal multimodal drug combination should enhance analgesia while at the same time decrease drugrelated adverse side effects. It is the general consensus that the gabapentinoids are opioid-sparing and effective in attenuating immediate postoperative pain; however, these drugs can also increase the risk of postoperative sedation, so great care should be taken when dosing these drugs, particularly in combination with opioid analgesics. Unfortunately, the optimal perioperative dosing regimen and treatment duration remain unclear. Preoperative dosing of gabapentin as high as 1,200 mg orally has been recommended; however, this may place the patient at an increased risk for postoperative respiratory depression. In a recent retrospective study52 involving patients undergoing total hip and knee arthroplasty, the authors suggest that premedication of patients with greater than 300 mg of gabapentin, as part of a multimodal analgesic regimen, is associated with an increased risk of postoperative respiratory depression. Unfortunately, these patients had also received a preoperative dose of sustained release oxycodone, which likewise put them at an increased risk for postoperative respiratory depression. In another placebo-controlled crossover study, the effects of pregabalin and remifentanil, alone and in combination, on analgesia, ventilation, and cognitive function were examined. Prudence therefore dictates that great care should be taken when dosing gabapentinoids in combination with opioids. In the opioid-naive patient, the preoperative dose of gabapentin should rarely exceed 300 mg orally. In addition, gabapentinoids should not be combined with a preoperative dose of sustained release opioid. Only in rare circumstances, such as in the opioid-dependent patient or in the patient at increased risk for chronic postsurgical pain. This binding appears to modulate the function and traffic of these channels, which appear on the synaptic bulb of presynaptic neurons. Calcium influx through these channels after a pain-evoked action potential is believed to trigger the fusion of synaptic vesicles with the neuronal membrane and consequent release of neurotransmitters in the dorsal horn of the spinal cord. Gabapentin may exert its analgesic effect by inhibiting or modulating this process. In addition, gabapentin may exert an analgesic effect by activating descending inhibitory noradrenergic pathways that regulate neurotransmission of pain signals in the dorsal horn of the spinal cord. Perioperative gabapentinoids: choice of agent, dose, timing, and effects on chronic postsurgical pain. However, because it takes gabapentin and pregabalin 4 to 6 hours and 8 hours, respectively, to reach peak cerebrospinal fluid levels dosing of the drug the evening prior to surgery may ultimately prove to be the most beneficial method of administration. The postoperative dosing of the gabapentinoid may therefore be titrated based on side effects, with larger doses being prescribed during the evening. The ideal gabapentinoid dosing regimen that can optimize 3959 immediate postoperative pain and minimize the risk of postoperative respiratory depression, while reducing the development of chronic postsurgical pain, has yet to be elucidated and merits further investigation. Following intravenous administration, the local anesthetic lidocaine has been shown to be analgesic, antihyperalgesic, and anti-inflammatory. Serum concentrations greater than 5 g/mL are associated with cardiovascular and central nervous system toxicity. Lidocaine infusion is contraindicated in any patient with arrhythmia, heart failure, coronary artery disease, StokesAdams disease (cardiovascular syncope) and heart block. Future studies are warranted that will identify surgical indications and ideal dosing regimens that are both safe and efficacious.