Norvasc
General Information about Norvasc
Hypertension, or hypertension, is a typical well being problem that affects millions of individuals worldwide. It is often referred to as a “silent killer” as a end result of it has no noticeable symptoms, but can cause serious injury to the guts and other organs if left untreated. Norvasc is prescribed to assist decrease blood pressure and scale back the chance of coronary heart attack and stroke in patients with hypertension.
Aside from its use in treating high blood pressure, Norvasc can be commonly prescribed for patients with angina, a condition characterized by chest ache or discomfort brought on by decreased blood circulate to the guts. By relaxing and widening the blood vessels, Norvasc helps to improve blood flow and oxygen supply to the center, thereby lowering the frequency and severity of angina episodes.
While Norvasc is generally well-tolerated, like any other medicine, it may cause side effects in some patients. Common unwanted effects could embody headache, dizziness, drowsiness, nausea, and swelling of the legs and ankles. These unwanted effects are usually gentle and subside as the body adjusts to the medicine. However, if these side effects persist or worsen, it is very important seek the advice of a physician.
Norvasc is on the market in the form of oral tablets in various strengths, starting from 2.5mg to 10mg. The dosage may differ relying on the patient’s age, medical historical past, and situation being handled. It is normally suggested to take Norvasc once a day, across the similar time each day, with or with out food. It must be taken as directed by the physician and shouldn't be stopped suddenly with out medical advice, as it might possibly trigger a sudden increase in blood strain.
Norvasc shouldn't be taken by patients with a known allergy to amlodipine or any other ingredients within the medication. It can be important to tell the physician about any other medications or dietary supplements being taken, as they could work together with Norvasc and cause potential issues.
In conclusion, Norvasc is a generally prescribed medicine for the remedy of hypertension, angina, and different heart-related situations. It helps to lower blood pressure and improve blood move, thereby reducing the risk of coronary heart assault and stroke. While it could cause some gentle unwanted effects, they're normally momentary and may be managed. It is important to observe the doctor’s directions and schedule regular check-ups to monitor the effectiveness of the medicine. With proper use and precautions, Norvasc might help improve coronary heart well being and quality of life for people who want it.
In rare instances, Norvasc could cause serious unwanted side effects such as a rapid or irregular heartbeat, severe dizziness or fainting, and swelling of the throat, tongue, or face. These symptoms could additionally be indicators of an allergic reaction or a more extreme aspect effect, and quick medical consideration ought to be sought.
Norvasc, also known by its generic name amlodipine, is a commonly prescribed medicine used to deal with hypertension, chest pain, and different heart-related conditions. It belongs to a class of drugs known as calcium channel blockers, which work by relaxing and widening the blood vessels, allowing for simpler blood flow and lowering blood pressure.
The frequency of diagnosis of patients with celiac disease has increased; however heart attack at 20 purchase norvasc canada, the majority of patients with this condition remain undiagnosed. The confirmation of a diagnosis of celiac disease should be based on a combination of findings from the medical history, physical examination, serology, and duodenal biopsy. The recommended serologic marker that is used for screening patients is serum antitissue transglutaminase antibody. Strict, lifelong adherence to a gluten-free diet is the only treatment for celiac disease that is currently available. Clinicians must evaluate the patient with celiac disease for nutritional deficiencies (including folic acid, vitamin B12, fat-soluble vitamins, iron, and calcium) due to malabsorption. Celiac disease is a small intestinal immune-mediated enteropathy caused by intolerance to ingested gluten, a storage protein found in wheat, barley, and rye. Genetic, environmental, and immune factors all play a role in the development of celiac disease. The mainstay of treatment of the disease is strict, lifelong adherence to a gluten-free diet. Celiac disease has also been known as celiac sprue, nontropical sprue, and gluten-sensitive enteropathy; however, these terms are currently not recommended. The non-specific use of celiac disease related terminology may lead to misunderstandings. It is therefore important that accepted terms associated with celiac disease be used, and understood when engaging in patient consultations or discussions with other healthcare providers. Patients with subclinical celiac disease have no or minimal symptoms but manifest mucosal damage on biopsy and have positive serologic testing. While the reason for this increase is not known, it may be due to environmental factors such as the changing nature of gluten or other factors associated with diet. Previously believed to rarely occur in nonwhite populations, improved screening and diagnostic techniques now provide evidence that the prevalence of celiac disease in many non-Western nations is similar to that in Europe and North America. This transition in dietary preferences may lead to an increased prevalence of the disease in those populations. Storage proteins similar to glutenins, called hordeins and secalins, are found in barley and rye, respectively. Table 41-1 refers to grains and other foods that do and do not contain gluten and related proteins. Ingestion of any of these proteins will lead to an autoimmune response in celiac disease patients. Wheat, barley, and rye are all derived from the Triticeae tribe of the grass (Gramineae) family. Oats, from the Aveneae tribe, are distantly related and therefore contain fewer disease-activating proteins. Genetic factors, in combination with exposure to gluten, are necessary for the development of celiac disease. A concordance rate of 85% in monozygotic twins has been reported, indicating that genetics play a large role in the disease, but other factors also are likely to involved. Both adenovirus and hepatitis C viruses are thought to act as triggers, whereas other agents, including Campylobacter jejuni, Giardia lamblia, rotavirus, and enterovirus infections, have been described in case reports as associated with celiac disease. Based on this finding, prolonged breast-feeding with introduction of gluten-containing grains during breast-feeding was recommended to help avoid the development of celiac disease. Gluten is unusually rich in the amino acids glutamine and proline, which enable part of the molecule to withstand the digestive processes. The presence of gluten in the lamina propria and an inherited combination of genes contribute to the heightened immune sensitivity to gluten found in patients with celiac disease (Table 41-2). Non-celiac gluten sensitivity is a condition in which the ingestion of gluten results in morphological or symptomatic manifestations in the absence of celiac disease. It is noteworthy that symptoms alone cannot reliably differentiate celiac disease from non-celiac gluten sensitivity. Therefore a diagnostic evaluation including celiac serology and small-intestinal biopsy (while the patient is including gluten in their diet) is needed. Differentiating between these disorders is very important as it will impact upon the implications of the level of adherence to the gluten-free diet, approach to continued disease-state monitoring and evaluation, and the counseling of family members (as nonceliac disease sensitivity does not appear to have a strong hereditary basis). In patients without celiac disease, the gliadin peptides are entirely degraded by lysosomal acid proteases during intestinal transcytosis. This then leads to villous atrophy, crypt hyperplasia, and the expansion of antibody-producing B cells found in celiac disease. Vomiting, irritability, anorexia, and even constipation are also common in these young patients. Extraintestinal manifestations such as short stature, neurologic findings (eg, peripheral neuropathy, ataxia, seizure, migraine, and dementia), or anemia are often found in older children and adolescents. Less common but important presentations of celiac disease in adults include abdominal pain, constipation, weight loss, neurologic symptoms, dermatitis herpetiformis, hypoproteinemia, hypocalcemia, and elevated liver enzymes. Some adults may be diagnosed as a result of having an endoscopy performed in response to their complaints of symptoms associated with gastroesophageal reflux. Clinicians should also note that individuals with certain disorders are more likely to have celiac disease than the general population. Although patients with these disorders are more frequently found to have celiac disease than the general population, these associated conditions are not believed to cause celiac disease. The co-occurrence of celiac disease and type 1 diabetes mellitus is 5 to 7 times more prevalent than celiac disease alone. Although these findings in diabetic patients may lead clinicians to test for celiac disease, testing for celiac disease in asymptomatic diabetes mellitus patients remains controversial. It is noteworthy however that researchers have reported that adults with undetected celiac disease and type 1 diabetes were found to have worse glycemic control and a higher prevalence of retinopathy and nephropathy.
An oral loading dose (eg blood pressure 7843 generic 5 mg norvasc free shipping, 20 mg/kg), should be divided into 3 to 4 doses and given at 4 to 6-hour intervals to therapeutic levels of between 10 and 20 mcg/mL (mg/L; 40-79 µmol/L). One should also remember that 100 mg of phenytoin acid is equal to 92 mg of phenytoin sodium. It has a relatively narrow therapeutic window, and dose titration is complicated by MichaelisMenten kinetics. There are also many drug interactions associated with its metabolism and protein binding. It may exacerbate seizures in generalized epilepsies and should be avoided in those epilepsies. Pregabalin Mechanism of Action Pregabalin is structurally related to gabapentin and binds to the 2 subunit of voltage-gated Ca2+ channels which possibly results in decreased release of the excitatory neurotransmitters glutamate, noradrenaline, substance P, and calcitonin gene-related peptide. It does not display dose-dependent bioavailability, and bioavailability is unaffected by food. A withdrawal reaction characterized by anxiety, nervousness, and irritability has been noted in patients being treated for generalized anxiety upon abrupt discontinuation of the drug. Dosing and Administration Pregabalin is started at doses of 150 mg/day divided into twice or thrice daily intervals. The manufacturer recommends that patients with end-stage renal disease maintained on hemodialysis receive a 25 to 75 mg daily dose with 25 to 75 mg given after every 4 hours of hemodialysis. Like gabapentin it can cause weight gain and peripheral edema, especially as the dose is increased. It is extensively metabolized by primary biotransformation via carboxylesterases with no active metabolites. Multiorgan hypersensitivity has occurred within 4 weeks of starting treatment in patients younger than 12 years of age. It is responsible for a modest increase in the clearance of carbamazepine, lamotrigine, phenobarbital, and phenytoin. Similarly, carbamazepine, phenytoin, primidone, and phenobarbital significantly increase the clearance of rufinamide. Valproic acid significantly decreases the clearance of rufinamide and elevates serum levels by 70%. Hepatic impairment causes higher and more prolonged plasma concentrations of the drug, although renal dysfunction does not change its pharmacokinetics. It also inhibits carbonic anhydrase, which may have some antiseizure effects but is likely not a major mechanism of action. Topiramate can also cause metabolic acidosis at doses as low as 50 mg/day, especially in patients with renal disease, severe respiratory disorders, diarrhea, surgery, and in patients on the ketogenic diet. Topiramate can modestly increase the clearance of valproic acid and increase formation of toxic metabolites. Doses can be initiated at 25 mg/day and increased by 25 to 50 mg/day every 1 to 2 weeks. Elimination is primarily renal, although hepatic metabolism occurs at higher doses. Disadvantages With rapid dosage escalation, topiramate can compromise cognitive functioning, including impaired word finding and impaired short-term memory. Valproic acid is extensively bound to albumin, and the valproic acid free fraction will increase as the total serum concentration increases. Because binding is saturable, monitoring of free fractions, although uncommon, may be better than total concentrations, especially at higher concentrations or in patients with hypoalbuminemia. The primary pathway of valproic acid metabolism is -oxidation, although up to 40% of a dose may be excreted as the glucuronide. It crosses into the placenta and concentrations may be up to five times higher in cord serum blood than in the mother due to higher binding in the fetal compartment. Alopecia and hair changes are temporary, and hair growth returns even with continued dosing. Weight gain can be significant for many patients and is associated with an increase in fasting insulin and leptin serum levels,138 possibly due to the inhibition of insulin metabolism by the liver139 and leading to the development of insulin resistance in obese patients. Valproic acid has also been shown to alter carnitine metabolism, and it is possible that carnitine deficiency may cause both liver toxicity and hyperammonemia140 but routine carnitine supplementation is not generally supported. Valproic acid decreases clearance of phenobarbital and lamotrigine by 30% to 50% and can lead to phenobarbital and lamotrigine toxicity. The concentration-dose ratio decreases with increasing dose probably because of increasing free concentrations and a resulting increase in clearance. The sprinkle capsule, designed to be opened and mixed with food, has a slower rate of absorption, which results in fewer fluctuations in the peak-to-trough ratio. Dosing may be initiated at 10 to 15 mg/kg/day and increased by 5 to 10 mg/kg weekly. It is also used in other neurologic or psychiatric disorders (eg, migraine headache and bipolar disorder). Place in Therapy Valproic acid is first-line therapy for generalized seizures, including myoclonic, atonic, and absence seizures. It can be used as both monotherapy and adjunctive therapy for focal-onset seizures, and it is very useful in patients with mixed seizure disorders. Its use is limited by potential long-term side effects such as weight gain and teratogenicity.
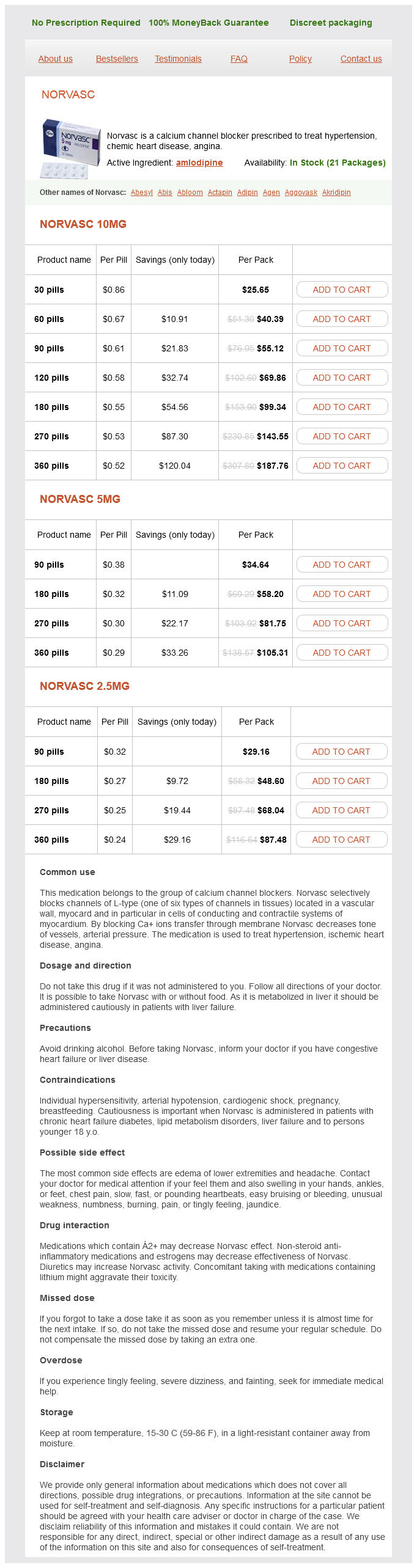
Norvasc Dosage and Price
Norvasc 10mg
- 30 pills - $25.65
- 60 pills - $40.39
- 90 pills - $55.12
- 120 pills - $69.86
- 180 pills - $99.34
- 270 pills - $143.55
- 360 pills - $187.76
Norvasc 5mg
- 90 pills - $34.64
- 180 pills - $58.20
- 270 pills - $81.75
- 360 pills - $105.31
Norvasc 2.5mg
- 90 pills - $29.16
- 180 pills - $48.60
- 270 pills - $68.04
- 360 pills - $87.48
Hepatic encephalopathy is categorized as type A arterial hypertension treatment norvasc 10 mg buy cheap, B, or C based on nomenclature developed by the 11th World Congress of Gastroenterology. Coagulation Defects End stage chronic liver disease is associated with decreased synthetic capability of the liver leading to decreased levels of most procoagulant factors as well as the naturally occurring anticoagulants, antithrombin and protein C. The rebalanced homeostasis seen in chronic liver disease can be tipped toward either thrombosis or clinically significant bleeding at any time depending on the circumstances experienced by the patient at the time. However, given the relatively high levels of von Willebrand factor present in cirrhosis, platelet function is actually increased. Cirrhotic patients with platelet counts as low as 60 × 109 per liter are able to preserve thrombin formation similar to the lower end of the normal range for healthy persons. While it has been observed that hyperfibrinolysis occurs in chronic liver disease owing to increased levels of tissue plasminogen activator and thrombin-activatable fibrinolysis inhibitor, reduced levels of plasminogen and increased levels of plasminogen activator inhibitor are also observed, both of which promote a hypofibrinolytic state. Osteoporosis, as a result of vitamin D malabsorption and resultant calcium deficiency, can also occur. A thorough history including risk factors that predispose patients to cirrhosis should be taken. Information concerning any history of transfusions, as well as any personal history of autoimmune or hepatic diseases, should be gathered. A family history should also be taken, looking especially for any family member with a prior history of autoimmune or hepatic diseases. Laboratory Abnormalities There are no laboratory or radiographic tests of hepatic function that can accurately diagnose cirrhosis. Tests that measure the level of serum liver enzymes are usually referred to as liver function tests. Liver function tests are often the first step in the evaluation of patients who present with symptoms or signs suggestive of cirrhosis. Liver injury, whether acute or chronic, results, at some point in the course of the disease, in increases in the serum concentrations of the aminotransferase enzymes. The degree of elevation, rate of rise, and nature of the course of alteration in aminotransferase serum levels are helpful in suggesting possible etiologies. Liver function tests will typically be elevated to the highest levels in acute viral, ischemic, or toxic liver injury. Chronic hepatitis and cirrhosis patients may present with elevated aminotransferase levels, but they may also present with aminotransferase levels within the normal reference range. The degree of aminotransferase level elevation is dependent on the course of the hepatic injury being experienced by the patients and also depends on when the enzyme levels are tested. Seventy percent of patients with alcoholic liver disease in the study by Cohen and Kaplan had ratios greater than 2, whereas 92% of patients had ratios greater than 1. Child-Pugh Classification and Model for End-Stage Liver Disease Score the Child-Pugh classification system has gained widespread acceptance as a means of quantifying the myriad effects of the cirrhotic process on the laboratory and clinical manifestations of this disease. Elevated conjugated bilirubin levels with concomitant increases in alkaline phosphatase and normal aminotransferase levels are a sign of cholestatic disease and possible cholestatic drug reactions. Causes of conjugated hyperbilirubinemia include bile duct obstruction, hepatitis, cirrhosis, primary sclerosing cholangitis, primary biliary cirrhosis, total parenteral nutrition, drug toxins, and vanishing bile duct syndrome. If a hepatocellular pattern predominates, the magnitude of elevation provides diagnostic assistance. If the degree of elevation is greater than 10 times normal, the etiology is likely a result of drugs or other toxins, ischemia, or acute viral hepatitis. Unfortunately, most liver enzyme abnormalities will fall into a mixed pattern providing limited diagnostic assistance. Endoscopic and Radiographic Abnormalities While no radiographic test is considered a diagnostic standard for cirrhosis, radiographic studies may be used to detect ascites, hepatosplenomegaly, hepatic or portal vein thromboses, and hepatocellular carcinoma. Hepatic nodularity, irregularity, increased echogenicity, and atrophy are all ultrasonographic findings indicative of cirrhosis. Computed tomography and magnetic resonance imaging can demonstrate liver nodularity as well as atrophic and hypertrophic changes. Ascites and varices may also be detected on computed tomography or magnetic resonance imaging scans. Liver Biopsy Liver biopsy should be considered after a thorough noninvasive workup has failed to confirm a diagnosis in suspected cirrhosis. Liver biopsy has a sensitivity and specificity of 80% to 100% for an accurate diagnosis of cirrhosis and its etiology. The success of biopsy as a diagnostic tool is dependent on the number of histologic samples retrieved as well as the sampling method used. Identify and eliminate, where possible, the causes of cirrhosis (eg, alcohol abuse). Assess the risk for variceal bleeding and begin pharmacologic prophylaxis when indicated. Prophylactic endoscopic therapy can be used for patients with high-risk medium and large varices as well as in patients with contraindications or intolerance to nonselective -adrenergic blockers. Endoscopic therapy is also appropriate for patients suffering acute bleeding episodes. Variceal obliteration with endoscopic techniques in conjunction with pharmacologic intervention is the recommended treatment of choice in patients with acute bleeding. Evaluate the patient for clinical signs of ascites and manage with pharmacologic therapy (eg, diuretics) and paracentesis. Frequent monitoring for signs of hepatorenal syndrome, pulmonary insufficiency, and endocrine dysfunction is necessary. Desired Outcomes the desired therapeutic outcomes can be viewed in two categories: resolution of acute complications such as tamponade of bleeding and resolution of hemodynamic instability for an episode of acute variceal hemorrhage and prevention of complications through lowering of portal pressure with medical therapy using non-selective -adrenergic blocker therapy or supporting abstinence from alcohol.