Olanzapine
General Information about Olanzapine
Olanzapine is especially helpful in treating agitation because of its rapid onset of motion. This signifies that it might possibly begin working within hours of being taken and might help calm a person down shortly, avoiding additional escalation of their agitation. It is usually used for short-term treatment and is commonly mixed with other medications for optimum effectiveness.
In conclusion, olanzapine is a useful medicine for the short-term treatment of agitation attributable to schizophrenia or bipolar dysfunction. It works by blocking particular receptors in the mind and can shortly calm a person down during an episode of agitation. While it could have potential side effects, it's a useful gizmo in managing the symptoms of these extreme mental disorders. However, it should always be taken underneath the steering of a healthcare skilled, and any issues or unwanted facet effects ought to be reported to a well being care provider immediately.
Schizophrenia is a extreme mental dysfunction that impacts roughly 1% of the inhabitants worldwide. It is characterized by symptoms such as delusions, hallucinations, disorganized pondering, and emotional flatness. Bipolar disorder, however, is a temper disorder that causes extreme shifts in mood, vitality, and behavior. The signs of bipolar dysfunction can vary from episodes of extreme euphoria and happiness to feelings of intense unhappiness and hopelessness.
Despite its effectiveness, olanzapine isn't with out potential unwanted side effects. Like most drugs, it could possibly cause drowsiness, dizziness, dry mouth, and constipation. It can even improve the danger of weight acquire, high cholesterol, and diabetes. Therefore, it is important for patients taking olanzapine to have regular check-ups with their physician and to follow a healthy diet and train routine to attenuate these risks.
Aside from treating agitation, olanzapine has also shown to be efficient in managing other signs of schizophrenia and bipolar dysfunction. These include delusions, hallucinations, and disordered considering, as properly as temper signs corresponding to mania and depression.
One of the primary makes use of of olanzapine is for the remedy of agitation in sufferers with schizophrenia or bipolar disorder. Agitation is a term used to describe a variety of behaviors, similar to restlessness, verbal or physical aggression, and irritability. These behaviors could be triggered by a wide range of factors, including stress, anxiousness, and adjustments in treatment. Agitation just isn't a symptom of the dysfunction itself but is often a facet impact or a manifestation of an underlying psychiatric condition.
Olanzapine, additionally recognized by its brand name Zyprexa, is a medicine used for the remedy of schizophrenia and bipolar disorder. It belongs to a category of drugs often recognized as atypical antipsychotics and was first permitted to be used within the United States in 1996.
Olanzapine works by blocking particular receptors within the mind, particularly the dopamine and serotonin receptors. Dopamine is a neurotransmitter concerned in regulating pleasure, motivation, and reward, whereas serotonin is concerned in mood regulation. By blocking these receptors, olanzapine may help scale back the signs of schizophrenia and bipolar dysfunction.
Besides the medical treatment medications questions cheapest olanzapine, the patients and their parents need moral support and reassurance. Parents should be explained hygienic measures, proper diet and importance of taking treatment completely and regularly. Multidrug Therapy (MdT) It is now a well known fact that, simultaneous administration of several different antibacterial agents may prevent the emergence of drug resistant mutants. Parents should be advised to give rifampicin on empty stomach and clofazimine with meals or with a glass of milk. When compared to histopathological examination, a significant enhancement of 15% in diagnosis was seen. Treatment of reactions Drugs commonly used in these conditions are antimalarials like chloroquine (given orally), antimonials. Symptoms like iritis and neuritis occurring during reactions (or occurring independently) should be properly treated in order to avoid irreversible sequelae, i. As of 1st August 2010, more than 214 countries and overseas territories or communities have reported laboratory confirmed cases of pandemic influenza H1N1 2009, including over 18449 deaths. This is of course the tip of the iceberg as is evident from a seroepidemiology study done from Pune, India during the peak transmission showed that the peak seroprevalence was 7. Now novel H1N1 infection has become part of seasonal circulating virus though for some more time it will continue to infect and affect more severely the younger people more frequently than others. Hence virus spreads mainly via coughing, sneezing, hands, social contact, and from medical interventions like suctioning, nebulization and open ventilation which generate respiratory mist. If illness persists beyond 7 days, person remains infective till resolution of symptoms. When both the H and N antigens change such way that they are antigenically totally different from the past circulating strains it is called as antigenic shift and it results in pandemic as the population has no immunity to the new virus. The novel H1N1 2009 strain responsible for current pandemic is a re-assortant virus with gene segments from viruses of swine (European, North American and Asian; five segments), birds (two segments) and humans (one segment). Novel H1N1 2009 virus is antigenically different from the earlier human H1N1 viruses. It was believed that this virus has no cross protection from previous exposure to seasonal H1N1 virus. However we now know that the novel H1N1 2009 virus infection is milder in elderly population and hence there seems to some cross protection between this virus and the 1918-1919 H1N1 virus. Pandemic H1N1 2009 infection, though milder than previous influenza pandemics and with less mortality, affected healthy young people more often than the elderly people. In India, 33% of cases were reported in 519 years of age group and 40% in 2039 years of age group; seroepidemiology study done from Pune, India during the peak transmission showed that the peak seroprevalence in general population was 7. Seroprevalence was higher in people exposed to children and sick patients and was 20% in hospital staff, 35. Pregnancy, asthma, other lung diseases, diabetes, morbid obesity, autoimmune disorders and associated immunosuppressive therapies, neurological disorders and cardiovascular disease are some of the risk factors for increased morbidity and mortality associated with pandemic influenza. Spectrum of illness can vary from non-febrile upper respiratory tract infection to severe and often fatal pneumonia. The most commonly reported symptoms include cough, fever, sore throat, malaise and headache. Fever is absent in 309 some outpatients and in up to 1 in 6 surviving hospitalized vip. Among patients presenting with acute respiratory illness for care in Mexico, 13% tested positive for new influenza A (H1N1) virus infection (about one-fifth have had seasonal influenza), of whom about 10% have been hospitalized and one-third of those hospitalized required mechanical ventilation. They are also counseled to take rest and measures of infection control at home as discussed later to prevent spread of infection to their contacts and in community. Other complications known to occur, though rare, include rhabdomyolysis, renal failure, myocarditis, hemophagocytic syndrome. There are patients who are at risk of developing complications following influenza infection because of underlying medical conditions that includes those who have chronic pulmonary (including asthma), cardiovascular (except hypertension), renal, hepatic, neurologic, hematologic, or metabolic (including diabetes mellitus) disorders; those who are immunosuppressed (including immunosuppression caused by medications or by human immunodeficiency virus); those who are or will be pregnant during the influenza season; those aged 6 months to 18 years and receiving long-term aspirin therapy and who therefore might be at risk for experiencing Reye syndrome after influenza virus infection; and residents of nursing homes and other chronic-care facilities. The swab should be placed in transport medium containing tube and stored and transported at 4°C within 24 hours of collection; or else it should be stored at 70°C. Serological testing is not recommended as it can only tell whether the strain is type A or type B and cannot differentiate between pandemic H1N1 and other type A seasonal influenza strains. Antiviral therapy should be started as early as possible, preferably within 48 hours of onset of illness to be maximally effective. However it should be started even if it is delayed at any stage of active disease when ongoing viral replication is anticipated or documented. It is especially recommended in individuals at high risk of complications like children less than 5 years of age, patients with progressive respiratory disease including pneumonia and those with high risk medical conditions. Oseltamivir is preferred being oral agent and with minimum side effects and gives higher systemic level. Oseltamivir is the recommended treatment for lower respiratory tract complications. Inhaled zanamivir has been temporally associated with bronchospasm and patients with pre-existing airway disease appear to be at increased risk for this severe adverse reaction. There is no role of using preventive antiviral therapy due to risk of development of drug resistance. Hand hygiene and cough etiquette are important measures for a patient who is managed at home. Surgical mask is not as effective and tends to clog within 24 hours making it ineffective and uncomfortable. Only N95 masks are highly effective in preventing spread of virus, but are expensive, not easily available and are best used in hospital set up. Isolation in home for 510 days also helps in preventing spread to contacts at work places.
The advantages of this procedure are technical simplicity treatment 20 initiative olanzapine 7.5 mg order otc, maintenance of low right atrial and coronary sinus pressure and reduction in risk of formation of atrial thrombi and perhaps reduction in arrhythmias. In the bidirectional Glenn procedure, the upper end of the divided superior vena cava is anastomosed end to side to the superior aspect of the undivided right pulmonary artery, thus diverting the superior vena caval blood into both right and left pulmonary arteries. Hemodynamic advantages associated with the bidirectional Glenn include, improved effective pulmonary flow, reduced total pulmonary flow and less left ventricular volume overloading. Staging the Fontan appears to decrease overall mortality, presumably related to improving the ventricular function by correcting afterload mismatch associated with one stage Fontan. At the present time, staged Fontan with bidirectional Glenn initially followed later by extracardiac conduit diversion of the inferior vena caval blood into the pulmonary artery appears to be the preferred approach. A bidirectional Glenn procedure (superior vena cava to pulmonary artery anastomosis) may be performed around the age of 6 months. Preoperative catheter evaluation to define the pulmonary artery pressure and anatomy and to exclude a persistent left superior vena cava (because it may divert blood away from the pulmonary arteries) prior to bidirectional Glenn surgery should be undertaken. At the time of bidirectional Glenn procedure, stenoses, if any of the pulmonary artery should be repaired. Issues related to subaortic obstruction and mitral valve regurgitation should also be addressed. When the patient reaches the age and size (approximately 15 kg) suitable for Fontan-Kreutzer operation, diversion of inferior vena caval blood into the pulmonary artery either by a lateral tunnel or extracardiac conduit is recommended. At the present time extracardiac conduit diversion of inferior vena caval blood into the pulmonary artery is preferred by most surgeons. Immediately prior to Fontan conversion, cardiac catheterization should be undertaken to ensure normal Medical Management Following Palliative Surgery Problems encountered with tricuspid atresia patients are similar to those found in other types of cyanotic cardiac malformations. Appropriate monitoring for and treatment of relative anemia, polycythemia, coagulopathy and hyperuricemia should be undertaken. The risks for development of a cerebrovascular accident or brain abscess are similar to those seen with other cyanotic anomalies. Historical Aspects of Corrective Surgery for Tricuspid Atresia Fontan72 and Kreutzer73 concurrently described physiologically corrective operations for tricuspid atresia in 1971. Fontan operation, as described by Fontan consisted of superior vena cava-right pulmonary artery shunt (classical Glenn), anastomosis of the proximal end of the divided right pulmonary artery to the right atrium directly or by means of an aortic homograft, closure of the atrial defect, insertion of a pulmonary valve homograft into the inferior vena caval orifice and ligation of the main pulmonary artery, thus bypassing the right ventricle completely;72 it would appear that Fontan concept was to use the right atrium as a pump. Many modifications of these procedures have been suggested, as reviewed elsewhere by us. Over a period of time, a number of other concepts/procedures evolved and these include total 408 anatomy and pressure of the pulmonary artery as well as normal left ventricular end-diastolic pressure. At the same time, aortopulmonary collaterals should be evaluated by means of selective subclavian artery and descending thoracic aortic angiography. If collateral vessels are present, they should be occluded with coils or devices, as appropriate. The criteria outlined by Choussat and associates106 have been modified or exceeded by many groups of workers. These factors, when present, would make the Fontan-Kreutzer operation a high-risk procedure and should be identified at the time of preoperative evaluation. They include elevated pulmonary artery pressure (mean pressure >18 mm Hg) or resistance (> 4 Wood units/m2), distorted or small (McGoon ratio of 1. With one or more of these risk factors, physiologically corrective procedures of the Fontan type may carry significant risk. In such high-risk Fontan-Kreutzer patients, leaving open a small atrial septal defect to allow decompression of the right atrium in the immediate postoperative period with a plan to close the defect later has been proposed. Six to twelve months later, transcatheter closure of the fenestration may be undertaken if the fenestration did not spontaneously close. In patients with transposition of the great arteries, early pulmonary artery banding, treatment of aortic coarctation, and relieving or bypassing subaortic obstruction should also be incorporated into the treatment plan. Follow-up after Corrective Operation Close follow-up after correction is indicated. Afterload reduction with an angiotensin-converting enzyme inhibitor is used by some cardiologists to improve left ventricular output. Because of the potential for development of thrombi in the right atrium, anticoagulants are routinely used by most cardiologists. I recommend platelet-inhibiting doses of Aspirin, others advocate Warfarin anticoagulation. Supraventricular arrhythmias (atrial flutter or fibrillation, paroxysmal supraventricular tachycardia) may be seen, particularly with older types of Fontan operation. In a patient without adequate control, electrophysiologic study and surgical or transcatheter ablation may be needed. Sick sinus node syndrome and atrioventricular block occur in some children and may require pacemaker therapy. Symptoms and signs indicative of obstruction to Fontan pathways should be promptly investigated. Obstructive lesions should be treated with balloon angioplasty, stenting or even surgery, as necessary. A persistent shunt may be due to intentional fenestration created at the time of Fontan or a residual atrial septal defect. If significant hypoxemia is present, the residual shunt should be closed, preferably by a transcatheter device. Closing the defect has beneficial effect in preventing paradoxical embolism and stroke.
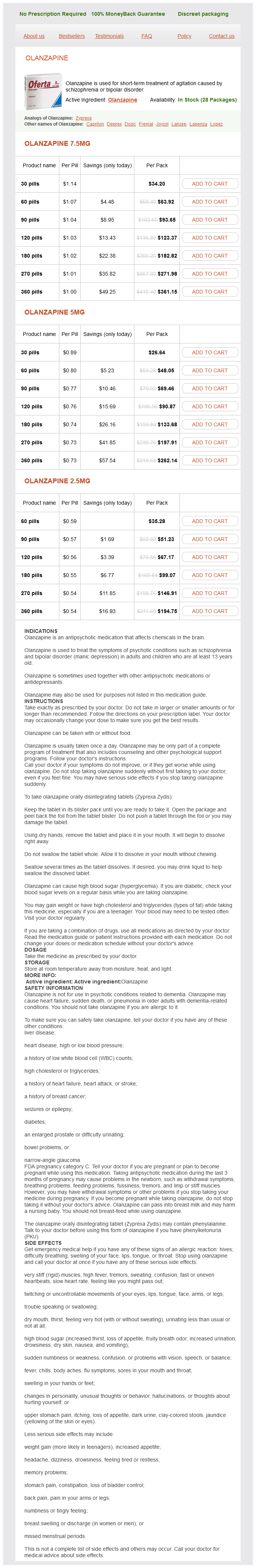
Olanzapine Dosage and Price
Olanzapine 7.5mg
- 30 pills - $34.20
- 60 pills - $63.92
- 90 pills - $93.65
- 120 pills - $123.37
- 180 pills - $182.82
- 270 pills - $271.98
- 360 pills - $361.15
Olanzapine 5mg
- 30 pills - $26.64
- 60 pills - $48.05
- 90 pills - $69.46
- 120 pills - $90.87
- 180 pills - $133.68
- 270 pills - $197.91
- 360 pills - $262.14
Olanzapine 2.5mg
- 60 pills - $35.28
- 90 pills - $51.23
- 120 pills - $67.17
- 180 pills - $99.07
- 270 pills - $146.91
- 360 pills - $194.75
Examination of the Lower Respiratory Tract Neck the important aspects to be assessed in relation to the respiratory tract are the trachea medicine park lodging cheap 2.5 mg olanzapine with mastercard, neck vein and the presence of surgical emphysema. Signs of Allergic Problems People with allergic rhinitis frequently develop a transverse nasal crease resulting from repeated rubbing of the nose to relieve the itching (Darriers line). Another feature of nasobronchial allergy is dark circles under the eyes (allergic shiners). Trachea this is inspected and palpated for deviation (in the standing or sitting position), with the examiner facing the patient. Tracheal deviation causes the clavicular head of the sternomastoid muscle on that side to appear prominent (Trail sign). Should there be massive pleural effusion, pneumothorax and large intrathoracic cysts and tumors; the finger will slip to the opposite side It is pulled to the same side in upper lobe collapse, fibrosis and pleural adhesions. Changes in the Anatomical Structures the nasal passages may be narrow, as in midface hypoplasia associated with various syndromes. Signs, such as the presence of ulceration, crusting, purulent or a blood-stained discharge, presence of foreign bodies, trauma and tumors (vascular and nonvascular) should be noted. Examination of the Ears the ears should be examined for congenital anomalies, infections, foreign bodies and impacted wax. Examine the mastoids and retroauricular areas for eczema, tenderness and lymph node enlargement. For better visualization of the external ear canal and tympanic membrane, pull the pinna up and posteriorly with the thumb and index finger. Otoscopic evaluation is a must for patients with fever of unknown or known origin, as well as those with ear symptoms. The otoscope should have a strong light and the speculum should be of the largest size that can fit comfortably into the ear canal. Gently place the otoscope over the external auditory meatus and inspect the external ear canal. Absence of the normal light reflex, dull appearance, bulging, retraction, perforation, and so on, should be noted. Examination of the Chest Inspection this should be performed with the chest as maximally exposed as the custom permits, with the eyes at the level of the chest, from head and foot ends and from front and lateral aspects. Assess the shoulders for drooping (indicates painful conditions of the chest wall on the same side, pleurisy, pneumonia, collapse and fibrosis), position of the cardiac apical impulse, and precordial shape. A localized bulge indicates parietal wall inflammatory swellings, hematoma or tumors. Localized paucity of movements occurs in trauma and in painful conditions of the chest wall and pleura, pleural effusion, pneumothorax, pneumonia, collapse and tumors of the lung. X-linked agammaglobulinemia; enlarged in infections and tumors), congestion, follicles or membranes. Chest movements are assessed over supraclavicular, upper interscapular and lower interscapular areas from the back, and infraclavicular and inframammary areas from the front. To do this, encircle the chest from both sides with four fingers and palm, with the thumbs meeting in the midline but not touching the chest wall. On inspiration, if one thumb remains closer to the midline it indicates reduced chest movements on that side. Tactile vocal fremitus is compared for spoken words over identical areas on both sides of the chest with the medial margin of the right palm. Percussion the examiner should master the technique of percussion to feel, rather than hear, the normal and abnormal lung resonance. The left middle finger (the pleximeter) is placed parallel to the long axis over the area to be percussed; back of the middle phalanx of the pleximeter finger is struck, as a tapping movement arising from the wrist. The terminal phalanx of the plexor finger should be at right angles to the metacarpal bone and the pleximeter finger while the blow is delivered. On the left side, the normal resonance is replaced by the tympanitic note of the stomach at the same level. The cardiac dullness should be verified on the left side and will be more resonant in emphysema. The normal resonance on the right side is replaced by liver dullness in the 7th space in the mid-axillary line, and on the left side by the tympanitic note of the stomach almost at the same level. A band of lung resonance that normally presents in the central area (Kronig isthmus) will be replaced by a dull note in massive pleural effusion, consolidation, neoplasia, or collapse of the apical part of lung. Subsequently, the upper and lower interscapular and the infrascapular spaces should be percussed. Lung resonance is increased in airway obstruction and pneumothorax; in the latter situation it reaches up to a tympanitic note. Localized obstruction occurs in congenital lobar emphysema or in partial obstruction by a foreign body in the bronchus (check valve or ball valve). Overall, hyperinflation occurs in obstructive airway disease, as in asthma pushing down the liver dullness. Percussion note is impaired or dull when the lung becomes more solid (pneumonia, consolidation, collapse, fibrosis, sequestration, abscess, infraction), or the pleura becomes thickened or contains fluid (pleural effusion, empyema, hemothorax) or solid (mesothelioma). A feel of resistance below the pleximeter finger is perceived in pleural effusion, as if percussed against a wall, and is described as a "stony dullness". In hydropneumothorax, a shifting dullness can be identified by percussing the chest (from anterior to posterior) in the supine, lying position of the patient.