Omnicef
General Information about Omnicef
Omnicef, also identified by its generic name cefdinir, is a robust antibiotic that is generally used to deal with a broad range of bacterial infections. It belongs to a category of medication known as cephalosporins, which work by interfering with the growth and copy of bacteria. Omnicef is out there in each oral suspension and capsule form, making it a flexible and handy choice for patients.
While Omnicef is usually properly tolerated, like all medicine, it does have potential side effects. Common side effects embrace nausea, diarrhea, and headaches. These unwanted effects are often delicate and may be managed by taking Omnicef with meals or adjusting the dosage. In rare circumstances, more critical unwanted aspect effects similar to allergic reactions or severe diarrhea could occur, and patients ought to seek medical attention if these happen.
For patients with pneumonia, Omnicef is usually prescribed as a first-line remedy. Pneumonia is a lung infection that can be attributable to numerous micro organism. Omnicef is effective against many of the micro organism that commonly cause pneumonia, making it a valuable software in fighting this potentially severe infection.
Omnicef can additionally be helpful in treating skin infections. This contains bacterial infections corresponding to impetigo, folliculitis, and cellulitis, among others. Omnicef is ready to penetrate the layers of pores and skin to succeed in the site of an infection and get rid of the micro organism inflicting the situation. This leads to faster healing and a discount in symptoms corresponding to redness, swelling, and ache.
Sinus infections, also called sinusitis, are one other frequent reason for an Omnicef prescription. These infections happen when the sinuses, the air-filled cavities behind the nose and cheeks, turn out to be infected and contaminated. Omnicef is ready to successfully deal with sinusitis by focusing on the bacteria liable for the infection and restoring health to the sinuses.
It is important to note that Omnicef is just effective in opposition to bacterial infections and received't be efficient against viral infections like the widespread cold or flu. Using Omnicef unnecessarily or not completing the total course of therapy can result in antibiotic resistance, making it harder to treat future infections.
One of the most typical makes use of of Omnicef is for the treatment of acute bacterial flare-ups of continual bronchitis. This condition occurs when the bronchial tubes, which carry air to and from the lungs, turn out to be infected and contaminated. Omnicef is especially efficient in treating this kind of an infection because of its capability to focus on and eliminate the micro organism liable for the flare-up. Patients sometimes see an enchancment of their symptoms inside a few days of starting the medication.
In conclusion, Omnicef is a flexible and potent antibiotic that is used to treat a extensive range of bacterial infections. It is especially efficient in treating situations similar to bronchitis, ear infections, throat and tonsil infections, pneumonia, sinus infections, and skin infections. While it may have some unwanted facet effects, Omnicef is a priceless device in the battle in opposition to bacterial infections and has helped countless patients recuperate from these illnesses.
In addition to bronchitis, Omnicef can additionally be generally prescribed for center ear infections, also called otitis media. This type of infection occurs when the middle ear turns into infected and fills with fluid, causing pain and discomfort. Omnicef is efficient in treating these kind of infections as a outcome of it could penetrate the thick mucus present in the center ear and reach the location of infection.
Throat and tonsil infections, such as strep throat, are also commonly treated with Omnicef. These kinds of infections are brought on by streptococcus bacteria and can lead to a sore throat, difficulty swallowing, and fever. Omnicef works by attacking and killing the micro organism, relieving signs and helping the patient recuperate.
This consultation should at minimum occur after the fourth recurrence of diverticulitis in patients over age 50 antibiotics quiz buy 300 mg omnicef fast delivery. Limited data are available as to whether a patient who has experienced less than four recurrent cases of diverticulitis or who is younger than age 50 would benefit from a segmental colectomy. Conservative management of perforated duodenal diverticulum: a case report and review of the literature. A recent investigation surveyed 790 ambulatory patients who were awaiting their annual primary care visit; 22. Pathophysiology Effective swallowing and transfer of food bolus into the stomach requires multiple steps. These steps can be broadly placed into two phases: the oropharyngeal phase and the esophageal phase. The oropharyngeal phase of swallowing ultimately transforms the hypopharynx from a respiratory organ to a digestive organ. This process is a carefully coordinated neuromuscular phenomenon with both autonomic and volitional components. During swallowing, the rapidity of bolus transit into the stomach is accomplished primarily by gravity. Esophageal peristalsis is a secondary contributor that functions to strip the bolus and clear the esophagus. Primary peristalsis is associated with oropharyngeal swallowing and propagates down through the predominantly striated muscle esophagus via a sequential activation pattern originating from the brainstem. This continues into the smooth muscle esophagus where it also engages the intrinsic enteric nervous system to promote peristalsis through a similar but distinct mechanism. Secondary peristalsis is stimulated by distention of the proximal esophagus and will generate a propagating peristaltic contraction similar to primary peristalsis without a swallow-induced trigger. The strength, propagation velocity, and order of peristaltic contractions can be altered and this may lead to motor abnormalities associated with dysphagia. Videoscopic swallowing examinations have the added benefit of providing functional information in addition to anatomic information. They can evaluate delay in initiation of pharyngeal swallowing, aspiration of solids and liquids, retrograde flow of ingested bolus, and residual pharyngeal contents. If there is a suspicion for a malignancy or mechanical obstruction, a referral to otolaryngology is required. Direct laryngoscopy is used to evaluate for anatomic lesions in the nasopharynx and hypopharynx. In addition to anatomic abnormalities, function can be assessed by having the patient drink liquids with the nasal endoscope positioned in the hypopharynx. Oropharyngeal pooling of liquid indicates ineffective hypopharyngeal clearance and can suggest a high aspiration risk. Cross-sectional imaging is often an adjunct to the functional assessment of videoscopic imaging or direct laryngoscopy when an obstruction is noted without a clear lesion noted on direct examination. Diagnosis Dysphagia is never a normal symptom and always requires additional investigation. The first step in the diagnostic evaluation of dysphagia begins with a careful history to distinguish true dysphagia from other associated conditions such as odynophagia and globus sensation. Odynophagia can coexist with dysphagia; however, the predominant symptom is pain during swallowing. It is likely a pharyngeal hypersensitivity that may coexist with other esophageal diseases or occur alone as a functional disorder. Unlike dysphagia, the symptoms in globus persist between swallows and may actually improve during the swallow. After the above conditions have been ruled out, the next step focuses on distinguishing oropharyngeal dysphagia from esophageal dysphagia. Unfortunately, patients have a difficult time communicating their symptoms because localization of the point of perceived obstruction is hampered by poor discriminant capacity and may be masked by compensatory mechanisms. Localization of dysphagia to the throat or sternal notch is unreliable because the point of obstruction may be further down in the body. However, localization in the midchest or below is more reliable that the obstruction is esophageal in origin. As a result, the most useful and underused test for distinguishing oropharyngeal and esophageal dysphagia focuses on observing the patient swallow sips of water in the office. Often this allows the distinction between oropharyngeal and esophageal dysphagia to become apparent. Patients with oropharyngeal dysphagia will have difficulty almost immediately after initiating a swallow, such as coughing, choking, and nasal regurgitation. Patients who can initiate a swallow without difficulty, but note symptoms soon after the swallow, are likely to have esophageal dysphagia. Furthermore, this exercise may be able to elicit associated odynophagia or regurgitation. A careful assessment of the oropharynx and a careful neck examination may unmask a mass lesion, and a neurologic examination should be performed if oropharyngeal dysphagia is suspected. Additionally, a skin examination and assessment of the oropharyngeal mucosa may be helpful in assessing for potential dermatologic diseases that are associated with esophageal dysphagia. Esophageal Dysphagia If oropharyngeal dysphagia is excluded on history, the evaluation of dysphagia should proceed to upper endoscopy to rule out a mechanical obstruction. Although an esophogram can be used to assess for obstruction, most patients will eventually require endoscopy to obtain biopsies to rule out malignancy or eosinophilic esophagitis. Additionally, endoscopy has the added benefit of being therapeutic in some circumstances, and thus it is more cost-effective to begin the evaluation with endoscopy. If the endoscopy is negative, the next step is to perform esophageal manometry to rule out an esophageal motor disorder. Oropharyngeal Dysphagia Differential Diagnosis the etiology of oropharyngeal dysphagia can be broadly separated based on neuromuscular causes and anatomic causes (Table 1).
This appears to be an effective therapy with fewer side effects than traditional therapy antibiotic kidney stones omnicef 300 mg purchase with mastercard. Lymphopenia (absolute lymphocyte count <1500 cells/microliter) does not require therapy. Typically, 1 mg/kg/day, or approximately 60 mg, is used for 4 to 6 weeks, with gradual tapering as long as the response is maintained. For patients who do not respond to glucocorticoids or are unable to taper prednisone to low doses, other treatments can be used. Immune thrombocytopenia results from antiplatelet antibodies that identify platelets for early destruction. Treatment is indicated when patients have signs or symptoms of spontaneous bleeding or when the platelet count drops below 50,000/mL. The initial treatment approach with glucocorticoids is similar to that used for hemolytic anemia. For patients with chronic thrombocytopenia or for those who cannot achieve an acceptable long-term dose of prednisone, steroid-sparing agents, including azathioprine,1 mycophenolate mofetil,1 danazol,1 rituximab,1 and intravenous immunoglobulin1 can be used in doses similar to those used for hemolytic anemia. Dapsone,1 cyclosporine (Sandimmune, Neoral),1 and cyclophosphamide (Cytoxan)1 have also been used. Manifestations of thrombotic thrombocytopenia purpura include fever, microangiopathic hemolysis, and central nervous system and renal abnormalities. Symptoms can range from mild to severe and include headache, aseptic meningitis, neuropathy, myelopathy, cognitive dysfunction, seizures, cerebritis, and stroke. A thorough evaluation is necessary to define the cause of nervous system dysfunction and differentiate it from a medication side effect. For seizures, antiepileptic therapy is used, preferably in coordination with a neurologist. Lupus cerebritis and transverse myelitis are two of the more serious manifestations that need to be treated emergently with aggressive immunosuppression in coordination with a rheumatologist or neurologist. Treatment includes high-dose corticosteroids and cyclophosphamide,1 similar to treatment for lupus nephritis. Dermatomyositis and Polymyositis Clinical Features Dermatomyositis may affect skin and muscle. Cutaneous dermatomyositis manifests with violaceous erythema of characteristic areas, including the periorbital skin. Connective Tissue Disorders 9 Rheumatology and the Musculoskeletal System capillary loops and erythema are observed. As in lupus, a punch biopsy of an actively inflamed cutaneous lesion shows characteristic features. Evaluation of patients with cutaneous dermatomyositis is not complete without assessment for systemic involvement. Serum aldolase is the most specific marker for myositis, and it can be used as a measure of response to treatment. Creatinine kinase and alanine aminotransferase levels may be elevated but are not specific indicators. An electromyogram shows dampening of signals, and a muscle biopsy shows a characteristic pattern of myositis. Inflammatory lung disease, diagnosed by the characteristic pattern on chest computed tomography, bronchoalveolar lavage, or biopsy, may be life limiting and therefore should be treated aggressively, similar to lung disease in scleroderma. Adult patients should have age-appropriate cancer screening because dermatomyositis is a paraneoplastic phenomenon in 10% to 50% of patients. Some patients present with characteristic cutaneous dermatomyositis but no systemic involvement. The risk of concurrent or subsequent cancer development is thought to be increased. These patients require monitoring for systemic involvement that may develop over time. Treatment Treatment of Limited Scleroderma For limited scleroderma, treatment with topical medium-potency corticosteroids such as triamcinolone 0. For rapidly evolving disease, prednisone1 1 mg/kg/day and methotrexate1 15 to 20 mg/week may help slow progression of disease. If this is not helpful, the -blocker prazosin (Minipress)1 1 mg three times daily or the angiotensin receptor blocker losartan (Cozaar)1 50 mg daily may be helpful. Antiplatelet therapy with low-dose aspirin1 (81 mg/ day) or dipyridamole (Persantine)1 50 to 100 mg three or four times daily may be useful. Topical vasodilators such as nitroglycerin ointment (Nitro-Bid)1 applied to the base of the affected finger three times daily can be helpful in refractory disease. Patients with severe recurrent digital ischemia may ultimately benefit from surgical sympathectomy. Treatment Patients with dermatomyositis need photoprotection similar to patients with lupus. Periodic evaluation by clinical examination and review of systems allows for early intervention for developing visceral or muscle involvement. Dermatomyositis with systemic involvement is initially treated with immunosuppression using prednisone at doses of 1 mg/ kg/day. Steroid-sparing agents are incorporated early in the disease and include antimalarials (methotrexate,1 azathioprine,1 and mycophenolate mofetil1) at doses that are used in treating lupus.
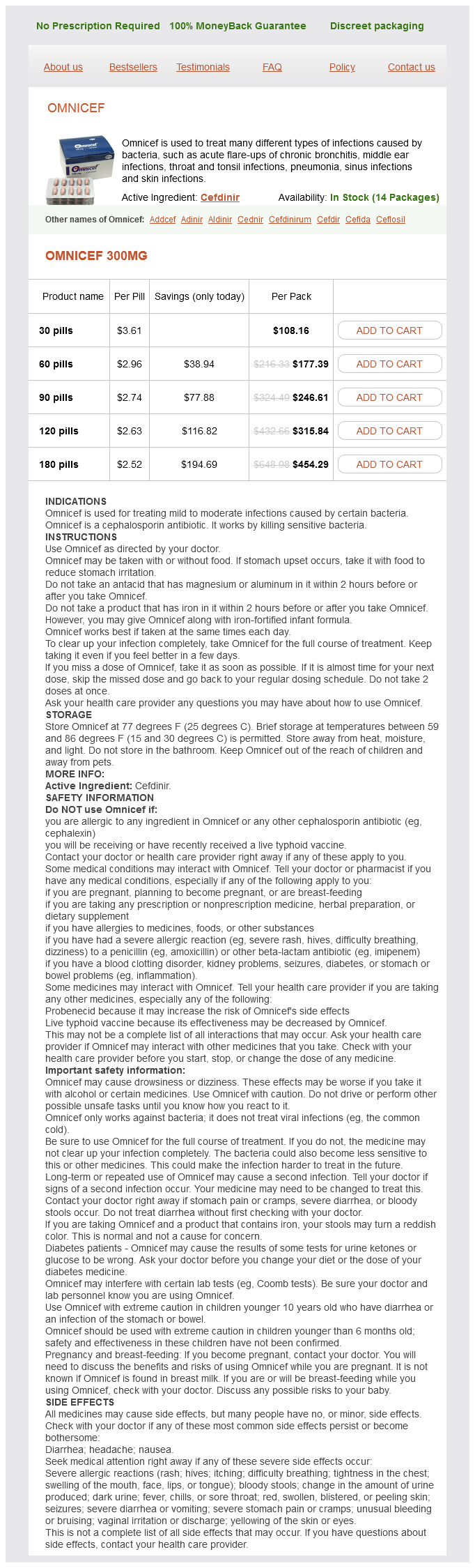
Omnicef Dosage and Price
Omnicef 300mg
- 30 pills - $108.16
- 60 pills - $177.39
- 90 pills - $246.61
- 120 pills - $315.84
- 180 pills - $454.29
Other sites of involvement have been described but are infrequent compared to those summarized above 1d infection tumblr cheap omnicef 300 mg online. Lung Acute Pneumonia Acute pneumonia is clinically indistinguishable from bacterial pneumonia. Patients may present with fevers, chills, dyspnea, and cough, which initially might not be productive but, with time, may be accompanied by sputum production. Radiographic findings can also be difficult to discern from those due to a bacterial pneumonia. The radiographic pattern of pulmonary blastomycosis includes the following: · Lobar infiltrates that mimic bacterial pneumonias · Cavitary lung lesions and miliary patterns, which can mimic tuberculosis · Mass lesions that may be mistaken for neoplasms · Cystic lesions that resemble abscesses There is no definitive plain radiograph or computed tomographic scan findings characteristic of pulmonary blastomycosis. The spectrum of clinical pulmonary disease ranges from spontaneous resolution to pneumonia, with or without the acute respiratory distress syndrome; the latter is accompanied by high (50%89%) mortality rates. Chronic Pneumonia A nonresolving pneumonia is one of the hallmarks of pulmonary blastomycosis. Chronic pneumonia may be associated with fever, chills, weight loss, sputum-producing cough, and hemoptysis. There is no characteristic radiographic appearance to help establish the diagnosis. Skin Cutaneous lesions are the most common extrapulmonary manifestations of blastomycosis. Lesions usually result from dissemination of a primary pulmonary lesion or rarely from direct inoculation. Lesions can have a number of different appearances, with verrucae (wartlike lesions) and ulcers being the most common establishes a presumptive diagnosis. Serologic assays are extremely variable in their sensitivity and specificity and do not play a role in confirming or excluding the diagnosis, thus limiting their value in therapeutic decision making. A reliable skin test is unavailable, but a urinary antigen detection assay exists that may aid in diagnosis and may be of benefit to follow the efficacy of treatment in established infections. Lipid preparations of amphotericin B (Abelect, Amphotec, AmBisome)1 have been shown to be effective in animal models, although clinical trial data are unavailable for these agents in humans. Clinical experience suggests that the lipid formulations are as effective but less toxic than the deoxycholate preparation. Patients on itraconazole should have serum 1 levels of the antifungal drug measured after at least 2 weeks of therapy, targeting a level >1. Ketoconazole (Nizoral), although once recommended as the agent of choice, is less effective and more toxic than itraconazole. Experience with fluconazole (Diflucan)1 for the treatment of blastomycosis is limited, although in vitro studies have demonstrated that fluconazole is effective against B. The echinocandins (caspofungin [Cancidas],1 micafungin [Mycamine],1 and anidulafungin [Eraxis]1) have limited activity against B. Box 2 summarizes the therapeutic options for treatment of various types of blastomycosis. Amphotericin B-based therapy is usually the treatment option of choice in persons who have severe disease. Whenever the patient is clinically stable, it is desirable to switch from the potentially toxic amphotericin B to a less-toxic agent (usually an azole). In patients with overwhelming pulmonary disease, amphotericin B-based products are the therapeutic agents of choice. Blastomycosis Box 2 Establishing the Diagnosis of Blastomycosis Serology Current serologic assays are neither sensitive nor specific, and they should not be used to establish or refute a diagnosis or in therapeutic decision making. Antigen Detection the only currently available antigen detection assay has its greatest sensitivity in urine, although antigens can be detected in serum and other body fluids. The greatest benefit of the antigen detection assay may be to follow efficacy of treatment in patients with established disease (antigen levels decrease with successful treatment or rise with recurrence). Skin Testing A commercially available standardized reagent for skin testing is not available. Direct Examination A wet preparation of respiratory secretions or a touch preparation of tissues examined under high magnification by light microscopy can reveal the characteristic thick-walled, broad-based budding yeast form. However, this method has a low diagnostic yield: 36% for a single specimen and 46% for multiple specimens. Calcofluor white stains can help in identifying the pathogen but require fluorescence microscopy. Histopathologic Examination the fungus may be difficult to identify with hematoxylin and eosin stain. If there is a high index of suspicion, the Gomori methenamine-silver stain should be used to optimize detection of thick-walled, broadbased budding yeast forms compatible with B. Culture Diagnostic yield ranges from approximately 86% from sputum to 92% from specimens obtained by bronchoscopy. Confirmation of identity traditionally requires demonstration of thermal-dimorphism (mycelial-to-yeast conversion), which can further delay diagnosis. For patients with less-severe pulmonary disease, an alternative to amphotericin B is a 6- to 12-month course of oral itraconazole. A similarly prolonged course of oral itraconazole is also appropriate for persons with bone and joint disease. The precise duration of therapy, however, is unknown and should be individualized. Patients who are immunosuppressed and in whom the immunosuppression cannot be reversed can require lifelong suppressive itraconazole therapy at 200 mg per day. Overwhelming pulmonary blastomycosis associated with the adult respiratory distress syndrome.