Ondansetron
General Information about Ondansetron
In conclusion, Ondansetron, also known as Zofran, is a extremely potent and well-tolerated treatment used to forestall nausea and vomiting in patients present process chemotherapy or surgical procedure. Its effectiveness, minimal unwanted effects, and versatility make it a priceless tool within the management of those signs. As with any medicine, it is essential to use Ondansetron as directed by your healthcare supplier and inform them of any underlying medical conditions or medicines you are taking to ensure secure and efficient treatment.
Nausea and vomiting are frequent side effects of most cancers chemotherapy, and they are often debilitating for a patient. In addition, sufferers who bear surgical procedure may experience these symptoms, which can delay their recovery course of. This is the place Ondansetron comes into play – it effectively blocks the indicators that trigger these signs, providing reduction to sufferers and allowing them to better tolerate their treatments or recover faster from surgery.
Ondansetron is on the market in several types, together with tablets, oral resolution, and injections. The acceptable form and dosage depend upon the affected person's condition, age, and medical history. Patients are suggested to observe the dosage directions given by their healthcare supplier and to take the medication on the prescribed time for max effectiveness.
Ondansetron, generally known as Zofran, is a medication that is primarily used to prevent nausea and vomiting associated with cancer chemotherapy or surgical procedure. It is a type of drug that belongs to a class of medicines called serotonin 5-HT3 receptor antagonists. Ondansetron works by blocking the motion of serotonin, a chemical in the physique that may set off nausea and vomiting.
However, like some other medication, Ondansetron might have some precautions and contraindications. It just isn't appropriate for sufferers with a history of allergic reactions to this medication or other serotonin 5-HT3 receptor antagonists. It is also not really helpful to be used with certain drugs, as they may interact negatively. Therefore, it is crucial to inform your healthcare supplier about any medicines you are presently taking to keep away from potential interactions.
Moreover, Ondansetron is a well-tolerated drug with minimal unwanted aspect effects. The commonest unwanted effects reported are headache, dizziness, and constipation, but these are gentle and manageable. Unlike different medications used for a similar objective, Ondansetron is not known to trigger sedation or drowsiness, which makes it highly suitable to be used in most cancers sufferers who're already coping with the side effects of their therapies.
In addition to its use in cancer patients, Ondansetron can be useful in treating nausea and vomiting in other conditions, corresponding to gastroenteritis and morning sickness in pregnant girls. It has also been shown to be effective in managing the symptoms of opiate withdrawal and postoperative nausea and vomiting. This versatility makes Ondansetron a useful medicine for healthcare providers, as it may be used to address various situations.
One of probably the most important advantages of Ondansetron is its efficacy. Numerous medical trials have proven that this medicine is highly effective in preventing and treating nausea and vomiting in patients undergoing chemotherapy or surgery. It has been reported that up to 90% of sufferers experience aid from their symptoms after taking Ondansetron.
The small vessels of the kidney and the glomerular capillaries are also frequently the target of small vessel vasculitides treatment naive purchase ondansetron 4 mg without a prescription. Clinically, the presence of a glomerular disease should be considered when proteinuria is present. Therefore, the approach to the patient with possible glomerular disease should begin with an assessment of the protein excretion in the urine and a microscopic analysis of the urine for dysmorphic red blood cells and/or red blood cell casts. When hematuria and/or proteinuria has been identified and glomerular disease is determined to be the most likely etiology, further clinical information and serologic testing can assist in the classification of the renal disorder before invasive testing. Although it is often difficult to predict the histologic pattern of injury in a patient with glomerular disease, patients frequently fall into two general clinical presentations-the nephritic syndrome and the nephrotic syndrome. Patients with the nephritic syndrome typically present with hematuria, dysmorphic red blood cells and/or red blood cell casts, and proteinuria. The proteinuria can range from 200 mg/day to heavy proteinuria (greater than 10 g/day). Patients with the nephrotic syndrome present with proteinuria, hypoalbuminemia (serum albumin less than 3. Dysmorphic red blood cells and casts are typically absent, but exceptions do exist. Additional complications of the nephrotic syndrome include hyperlipidemia, thrombosis, and infection. The diseases that cause the nephrotic syndrome can lead to chronic, progressive renal injury, but typically are more slowly progressive than diseases presenting as the nephritic syndrome. The pathologic diagnosis of glomerular diseases incorporates the histologic pattern defined by light microscopy, immunofluorescence staining for immunoglobulins (Igs) and complement proteins, and examination of the glomerular ultrastructure by electron microscopy. The primary glomerular diseases are listed in Table 9-1, with the prominent histologic findings on biopsy that define the disorder. There is a general correlation between the pattern of histologic injury and the clinical presentation. Thus, the clinical findings can suggest the underlying pathologic process, although definitive diagnosis requires a biopsy. The clinician must also consider if there is a systemic process that may be causing the proteinuria. Primary glomerular diseases can often not be distinguished histologically from the injury pattern seen in systemic diseases, so this distinction is usually made clinically. The nephritic syndrome is usually caused by glomerular inflammation and manifests with an "active" urine sediment. Diseases that present with the nephrotic syndrome disrupt the size and charge-selective barriers that ordinarily prevent the ultrafiltration of macromolecules across the glomerular capillary wall. In cases in which the nephritic syndrome is the predominant clinical presentation, a search for systemic diseases is warranted Table 9-3). The history and physical examination should particularly focus on the assessment of rashes, lung disease, neurologic abnormalities, evidence of viral or bacterial infections, and musculoskeletal and hematologic abnormalities. Laboratory assessment should be tailored to the clinical findings in the history and physical examination. Serum complement (C3) levels are often 182 Chapter 9 the Patient with Glomerular Disease or Vasculitis Table 9-1. These early assessments may provide a presumptive diagnosis and should lead the clinician to an appropriate therapeutic intervention while awaiting renal biopsy results, but they are not a substitute for renal biopsy. Proper management of the glomerular diseases requires a tissue diagnosis to confirm the clinical findings and provide information regarding the acuity and chronicity of the disease process. With the identification of significant proteinuria, with or without other features of the nephrotic syndrome, secondary causes of proteinuria should be considered Table 9-5). History and physical examination should evaluate for the presence of viral and bacterial infections, malignancies (particularly lung, breast, and lymphomas), and chronic diseases (such as diabetes), and medications should be reviewed for their potential to cause glomerular proteinuria. Renal biopsy should be performed in all cases in which no cause is evident, or to determine the extent of renal disease to guide therapy or prognosis. Treatment of glomerular disorders can be approached by management of the nephrotic syndrome and immunomodulatory therapies for specific glomerular diseases and vasculitides. The management of systemic diseases that cause secondary glomerular injury is rapidly changing. Therefore, the reader is encouraged to refer to recent disease-specific reviews of the literature for current management strategies for these systemic diseases. Untreated nephrotic syndrome is associated with significant morbidity due to 184 Chapter 9 the Patient with Glomerular Disease or Vasculitis Table 9-3. Often treatment requires both general management and disease-specific treatment to achieve remission and lessen morbidity. The general treatment strategies that should be considered in the patient with nephrotic syndrome include management of proteinuria, hypertension, edema, hyperlipidemia, and hypercoagulability. In nephrotic syndrome, treatment to reduce the degree of proteinuria to the nonnephrotic range will often result in an elevation or normalization of serum proteins (such as albumin). The reduction in proteinuria is more pronounced if the patient complies with dietary salt restriction. Treatment to achieve goal blood pressure should include lifestyle modification (salt restriction, weight normalization, regular exercise, and smoking cessation). Edema associated with nephrotic syndrome should be treated with dietary sodium restriction (1.
The diagnosis of acute rejection requires an ultrasound-guided kidney biopsy medicine for diarrhea discount ondansetron 4 mg amex, with application of the Banff criteria to grade the severity of rejection or disclose other pathology. Although most acute rejection can be reversed, its occurrence remains a powerful predictor of long-term graft survival, most notably antibody-mediated rejection or T-cell rejection involving the large vessels. Recurrent Disease the diagnosis of recurrent disease is guided by the clinical scenario and knowledge of which diseases tend to recur in kidney transplants. Recurrent nephritis may present as proteinuria, nephrotic syndrome, microscopic hematuria, and loss of function. It can be differentiated from other causes (chronic allograft dysfunction, de novo glomerular disease) by kidney biopsy. In the patient who has undergone transplantation, the important variables are the frequency of recurrence and frequency of graft loss due to recurrence. Alternatively, IgA nephropathy recurs in approximately 50% of recipients, but uncommonly causes graft loss. Systemic lupus erythematosus may also recur microscopically in kidney allografts but rarely is clinically important. Glomerular disease was the cause of 30% of all graft loss in one study, half of which was due to recurrent disease. Chronic Allograft Damage Despite a significant reduction in the incidence of acute rejection over the last several decades, long-term graft survival has improved only marginally. The most common cause of graft loss is patient death with a functioning graft, the majority of which is due to cardiovascular disease, and accounts for 278 Chapter 13 the Patient with a Kidney Transplant close to half of all cases. The remaining cases of graft loss are due to a range of both immunologic (chronic rejection) and nonimmunologic. Glomerular pathology can consist of recurrent primary or de novo disease, the latter often in the form of transplant glomerulopathy. Chronic antibody-mediated graft damage, occasionally in the form of transplant glomerulopathy, is often due to medication nonadherence and has been reported as responsible for over 60% of graft failures. Chronic allograft damage is not typically a reversible disease, and treatment is patient specific. The success of kid- ney transplantation and the growing population of transplant recipients are unfortunately accompanied by the complications from comorbid diseases and side effects of long-term immunosuppression. Patients often die with functioning grafts due to cardiovascular disease, infections, and malignancy, and these and other conditions contribute to a spectrum of common disorders in transplantation. Infectious Diseases In the patient who has undergone transplantation, typical signs and symptoms of infection may be absent, and coinfections are common, necessitating increased scrutiny. Infections after kidney transplantation occur in patterns that are important to recognize. Immediately after transplant, patients are at risk for common postoperative infections: wound infections, pneumonia, line, and urinary infections. The first 6 months after transplant is marked by a risk of opportunistic infections due to more intense immunosuppression, especially after antibody induction. After 6 months, the risk of opportunistic infections is lower but remains present, and patients remain at risk for more frequent and severe infections with community-acquired pathogens. Some common pathogens and principles specific to kidney transplantation will be reviewed. Immunosuppression during Infection There are no clear guidelines for decreasing immunosuppression during infection. Furthermore, many infections carry an increased risk of acute rejection due to upregulation of immune surveillance and activity. In general, mild infections treated with appropriate antimicrobials can be managed without a change in immunosuppression. Severe or life-threatening infections should include attention to the requirement for stress doses of corticosteroids, which are often adequate to decrease the risk of rejection during an illness. Reduction of immunosuppression is best done with careful monitoring of graft function along with the consultation of transplant physicians. Clinically, the disease often presents as low-grade fever, leukopenia and/or thrombocytopenia, and malaise. Tissue invasion can occur in 5% to 15% of infections, with syndromes of pneumonitis, hepatitis, esophagitis, and diarrhea being most common. Immunohistochemical techniques and the presence of viral inclusions can be used to confirm the diagnosis through kidney biopsy. The mainstay of management is 280 Chapter 13 the Patient with a Kidney Transplant 4. There is no consensus on management or outcome of either disease in respect to kidney transplantation. For hepatitis B, patients with antigenemia usually receive evaluation and liver biopsy before transplant, as antiviral therapies may be more effective before transplantation. For hepatitis C, the effects on outcomes and management are somewhat controversial. Although many patients have mild, indolent disease, there are reports of rapid progression to cirrhosis and liver failure after kidney transplantation. A complicating factor is that interferon therapy increases the risk of acute rejection. Most patients with hepatitis C should receive liver biopsy to exclude cirrhosis and should have consideration of interferon therapy before transplantation.
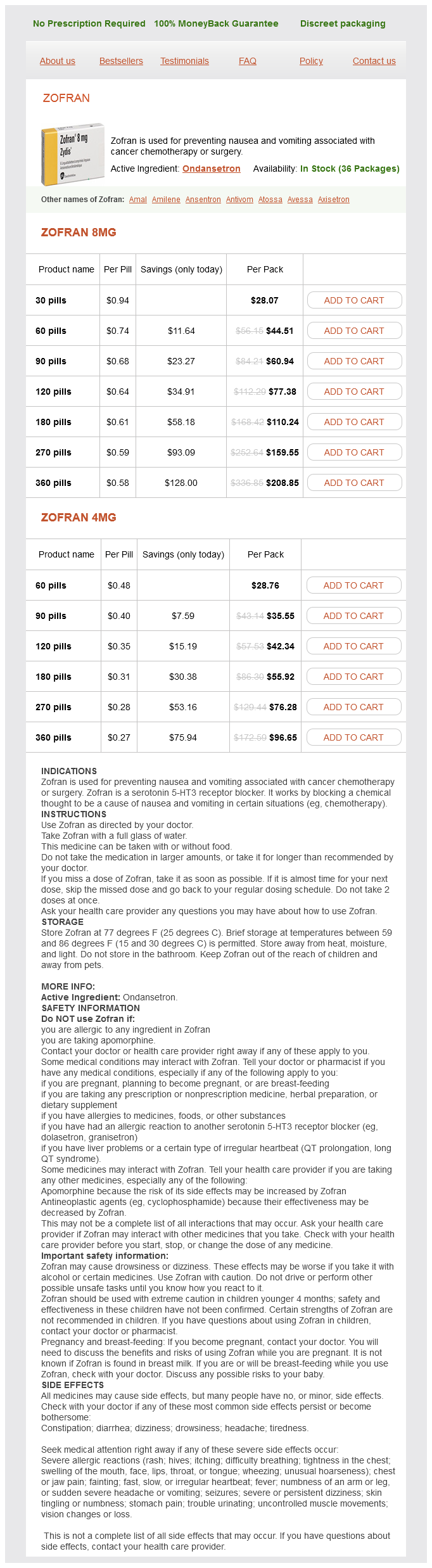
Ondansetron Dosage and Price
Zofran 8mg
- 30 pills - $28.07
- 60 pills - $44.51
- 90 pills - $60.94
- 120 pills - $77.38
- 180 pills - $110.24
- 270 pills - $159.55
- 360 pills - $208.85
Zofran 4mg
- 60 pills - $28.76
- 90 pills - $35.55
- 120 pills - $42.34
- 180 pills - $55.92
- 270 pills - $76.28
- 360 pills - $96.65
Its functions may include roles in temperature regulation medications bipolar discount ondansetron american express, permeability barrier, and innate immunity. As gestation progresses, the skin becomes less transparent, and peeling and surface cracking are increasingly seen, indicative of a thickening stratum corneum, and lanugo hair density peaks and then regresses. Despite definition of these milestones of gross and microscopic skin development, with the exception of 36 the permeability barrier, little is known about the competency or developmental timetable of most skin functions in premature infants. The permeability barrier in the preterm infant the permeability barrier resides in the stratum corneum through its provision of a hydrophobic lipid shield over the underlying nucleated cell layers. Instead, the extracellular compartment of the stratum corneum is filled with a highly organized series of hydrophobic lipid membranes in the extracellular spaces, whereas the anucleate corneocytes form an aqueous compartment as a result of loss of their plasma and organelle membranes. This interposition of hydrophobic lipid membranes in the extracellular compartment retards the movement of water inward or outward across the stratum corneum. The stacking of multiple layers of cornified cells surrounded by extracellular lipid bilayers further enhances this barrier to water movement, through the generation of a tortuous intercellular pathway for water movement. In addition to increasing stratum corneum thickness, the development of a competent permeability barrier in fetal rat skin is accompanied by (1) deposition of neutral lipid in the intercellular domains of stratum corneum; (2) increasing stratum corneum cholesterol and ceramide content; and (3) the organization of these lipids into mature lamellar membrane structures, as viewed by electron microscopy. It may not be surprising, therefore, that extremely premature infants do not respond as rapidly to maturational signals initiated by birth. In fetal rat skin, it is air exposure with evaporation of water from the skin surface that stimulates accelerated barrier formation, because this acceleration can be prevented by covering the skin surface with a vapor-impermeable membrane. One group demonstrated that preterm infants of mothers treated with glucocorticoids have reduced insensible water losses and lower serum sodium concentrations in the first 4 days of life, consistent with a maturational effect on the skin barrier. An acidic pH within the stratum corneum is required for normal permeability barrier homeostasis and for stratum corneum integrity and cohesion. This pH declines over the ensuing days to weeks to become acidic, comparable with that of adults. Instead, cutaneous water losses and respiratory fluid losses are together considered insensible. Neonatal fluid requirements must be modified by postnatal age to compensate for fluid redistribution. While the foregoing describes usual nursery practices, it is important to bear in mind that cutaneous fluid losses are not inherently insensible. Fluid replacements must be adjusted for a number of environmental conditions Table 4. They are also modified by the ambient temperature and humidity, since both affect the vapor pressure of water at the skin surface. Newer hybrid beds with a radiant warmer and humidifier allow for easy access to and observation of infants. Nonetheless, increased bacterial colonization under such dressings is observed in other clinical settings48 and remains a serious consideration with their use on preterm infants. In addition, many of these dressings contain adhesive materials, and even those without adhesives can cling to the moist skin surface of the preterm newborn and injure the epidermis, unless they are either removed carefully or allowed to detach spontaneously. Because the benefits of these agents have only been shown in studies with small numbers of subjects, confirmation in larger cohorts is required before their routine use can be generally recommended. Nonetheless, internal hydrocarbon accumulations (paraffinomas) are reported, albeit rarely. A systematic review of randomized controlled trials comparing prophylactic application of topical ointment in preterm infants to routine skin care55 reported that daily application of topical ointment increases the risk for coagulase-negative staphylococcal and nosocomial infections in these patients. Therefore, routine application of topical ointments is no longer recommended for premature infants. Circumstances may be very different in these settings: survival of preterm infants is much lower, care practices differ, and the morbid risks divergent. Indeed, sunflower seed oil and Aquaphor have been shown to reduce the incidence of nosocomial infections in Bangladesh and Egypt. The same factors that determine the movement of water from inside out also regulate the movement of low molecular weight substances from outside in. It is likely that there are also qualitative changes in the lipid composition and/or structural integrity of the lipid bilayers of immature stratum corneum that may further alter its permeability function. In addition to immaturity of the permeability barrier, several other factors in premature infants may contribute to toxicity from topical xenobiotics. Once absorbed, reduced levels of serum-binding proteins, such as albumin, may increase the proportion of free drug. Immaturity of detoxification mechanisms, such as hepatic conjugation and renal function, also alters drug pharmacodynamics and can increase toxicity. The increased permeability of premature skin to small hydrophilic molecules has also been exploited to enhance the percutaneous delivery of medications such as theophylline. Clinical implications of increased percutaneous absorption of xenobiotics In the care of the preterm infant, it is safest to assume that any medication applied to the skin may be absorbed systemically. As a corollary, the ideal topical medications for preterm infants are those with low systemic toxicity. It is also necessary to consider the composition of the vehicle used for topical drug delivery, because some components may also be absorbed across the immature skin barrier (see Chapter 5). While chlorhexidine in alcohol provides better antisepsis than either ingredient alone,91 alcohol itself poses a risk for percutaneous absorption and skin necrosis in the premature neonate, especially when used under occlusion. Conversely, systemic hypotension may increase the likelihood of an intracranial hemorrhage. Early initiation of oral feeds100 is undertaken to reverse a negative energy balance in the preterm infant. Caloric losses caused by increased evaporative water loss from the skin surface in all likelihood contribute to this caloric drain. Similarly, the threshold for irritant contact dermatitis from fecal contact (diaper dermatitis), for chemical burns from prolonged contact with antiseptics,90 or for thermal burns is much reduced. A regimen of emollient lubrication or use of nonadherent, semipermeable dressings may also help protect against mechanical injuries (see above).