Oxybutynin
General Information about Oxybutynin
In addition to overactive bladder, Oxybutynin also can assist with different kinds of bladder problems. These include bladder spasms, which may cause sudden, intense contractions of the bladder muscle tissue, resulting in urgency, frequency, and leakage, in addition to painful urination. Oxybutynin can help alleviate the discomfort and ache related to these symptoms, bettering the overall quality of life for those affected.
In conclusion, Oxybutynin, also referred to as Oxytrol, is an effective medicine for treating bladder problems such as overactive bladder, bladder spasms, and painful urination. It works by relaxing the muscular tissues within the bladder to reduce back urinary urgency, frequency, and leakage. While it could trigger some minor unwanted effects, it may possibly considerably enhance the quality of life for these living with bladder issues. It is essential to seek the assistance of with a doctor earlier than starting Oxybutynin and to comply with their directions for correct use and management of any potential unwanted effects.
Side effects of Oxybutynin could embrace dry mouth, constipation, drowsiness, dizziness, and blurred imaginative and prescient. These unwanted effects are often delicate and subside with continued use. It just isn't uncommon for folks to experience dry mouth whereas taking Oxybutynin. To handle this, it is strongly recommended to stay hydrated by consuming loads of water and using sugar-free lozenges or gum to stimulate saliva manufacturing.
Oxybutynin, offered under the brand name Oxytrol, is a drugs used to treat bladder problems such as urinary urgency, frequency, leakage, and painful urination. These symptoms could be attributable to conditions similar to overactive bladder or bladder spasms. Oxybutynin belongs to a class of medications known as anticholinergics, which work by relaxing the muscles in the bladder, thereby decreasing the signs related to bladder issues.
Overactive bladder is a common condition that affects tens of millions of people worldwide. It is characterized by a sudden and uncontrollable urge to urinate, typically accompanied by a frequent have to urinate. This can severely disrupt a person's daily activities and result in embarrassment and discomfort. Oxybutynin is useful in managing these signs by enjoyable the muscular tissues in the bladder, making it simpler to control the urge to urinate.
It is essential to notice that Oxybutynin just isn't a remedy for bladder problems, but quite it helps handle the signs. It is essential to continue taking the medicine as prescribed, as stopping abruptly can cause a rebound effect, leading to a worsening of signs.
Oxytrol shouldn't be utilized in people who have sure medical conditions, corresponding to glaucoma, abdomen or intestinal issues, or a blockage in the urinary tract. It can also work together with different medicines, together with sure antibiotics and antifungal drugs, in addition to blood stress medications and antidepressants. Therefore, it is essential to tell your physician about another medicines or dietary supplements you are taking before beginning Oxybutynin.
Oxybutynin comes in completely different varieties, together with extended-release tablets, immediate-release tablets, and pores and skin patches. The extended-release tablets are taken once a day and supply steady aid from signs, while the immediate-release tablets are usually taken a number of times a day as needed. The pores and skin patches, which are available as Oxytrol, are utilized to the pores and skin on a specific area of the abdomen, hip, or buttock, and launch the medication into the body gradually over a three to 4-day interval.
Effect of mandatory centers of excellence designation on demographic characteristics of patients who undergo bariatric surgery medicine urology order genuine oxybutynin. First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ruiz-Tovar J, Llavero C: Thromboembolic prophylaxis for morbidly obese patients undergoing bariatric surgery. Evidence of thromboembolism prophylaxis in bariatric surgery-results of a quality assurance trial in bariatric surgery in Germany from 2005 to 2007 and review of the literature. Portomesenteric thrombosis following laparoscopic bariatric surgery: incidence, patterns of clinical presentation, and etiology in a bariatric patient population. Dumping syndrome after esophageal, gastric or bariatric surgery: pathophysiology, diagnosis, and management. A pilot study of the effects of the somatostatin analog pasireotide in postoperative Acute Emergencies Related to Bariatric Surgery dumping syndrome. Algorithm to diagnose etiology of hypoglycemia after Roux-en-Y gastric bypass for morbid obesity: case series and review of the literature. Post-prandial hypoglycemia after bariatric surgery: pharmacological treatment with verapamil and acarbose. Potentially life-threatening sleep apnea is unrecognized without aggressive evaluation. Obstructive sleep-related breathing disorders in patients evaluated for bariatric surgery. American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. Perioperative risks of untreated obstructive sleep apnea in the bariatric surgery patient: a retrospective study. Early improvement in obstructive sleep apnea and increase in orexin levels after bariatric surgery in adolescents and young adults. Sex effect on obesity indices and metabolic outcomes in patients with obese obstructive sleep apnea and type 2 diabetes after laparoscopic Roux-en-Y gastric bypass surgery: a preliminary study. Long-term medical complications after malabsorptive procedures: effects of a late clinical nutritional intervention. The use of the biliopancreatic diversion as a treatment for failed gastric partitioning in the morbidly obese. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. Decreased energy density and changes in food selection following Roux-en-Y gastric bypass. Taste and olfactory changes following laparoscopic gastric bypass and sleeve Michael A. Comparison of nutritional status during the first year after sleeve gastrectomy and Roux-en-Y gastric bypass. Nutritional consequences of adjustable gastric banding and gastric bypass: a 1-year prospective study. High-dose vitamin D supplementation is necessary after bariatric surgery: a prospective 2-year follow-up study. A 46-yr-old woman with ataxia and blurred vision 3 months after bariatric surgery. Evaluation of vitamin and trace element requirements after sleeve gastrectomy at long term. Vitamin and mineral deficiencies after biliopancreatic diversion and biliopancreatic diversion with duodenal switchthe rule rather than the exception. Evaluation of serum Vitamin B12 level and related nutritional status among apparently healthy obese female individuals. Risk of secondary hyperparathyroidism after laparoscopic gastric bypass surgery in obese women. Regulation of bone mass by serotonin: molecular biology and therapeutic implications. Evaluation of bone disease in morbidly obese women after gastric bypass and risk factors implicated in bone loss. Persisting hypocalcemia after surgical parathyroidectomy: the differential effectiveness of calcium citrate versus calcium carbonate with acid suppression. Fracture risk following bariatric surgery: Acute Emergencies Related to Bariatric Surgery a population-based study. Change in fracture risk and fracture pattern after bariatric surgery: nested case-control study. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. Enteric hyperoxaluria, nephrolithiasis, and oxalate nephropathy: potentially serious and unappreciated complications of Roux-en-Y gastric bypass. Fat malabsorption and increased intestinal oxalate absorption are common after Roux-en-Y gastric bypass surgery. American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery Medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Preliminary comparison of sertraline levels in postbariatric surgery patients versus matched nonsurgical cohort.
When the original graft extends down to the femoral arteries treatment for chlamydia cheap oxybutynin online visa, the extra-anatomic reconstruction by necessity becomes more elaborate. While this is beneficial for performance of the proximal anastomosis, it carries significant risk, including splenic capsular injury, bleeding, pancreatic injury, and longer operative time and dissection, further complicating what is already a difficult operation. The author has used emergent percutaneous access in instances of aortic pathology and bleeding with proximal balloon control of the hemorrhage. With ultrasound guidance, femoral access can easily be obtained, even in the setting of prior aortofemoral bypass. This has the potential to be life-saving and allows some stabilization of the patient before operative management. If endovascular repair were an option anatomically, then the author would proceed with it as a bridge to stability. One important technique would be to avoid endografts with suprarenal fixation because this complicates subsequent open repair. If endovascular options are limited or anatomically not possible, the patient would then undergo midline incision with proximal supraceliac aortic control as described previously. Once proximal control is obtained, the operative team would proceed with infrarenal exposure and ligation of the aorta (two-layered closure). If there is limited contamination with minimal overall blood loss, in situ repair with an antibioticimpregnated graft is a consideration. Note the lateral location of the incision used to expose the mid-to-distal profunda femoris artery. In this high-risk patient population, endovascular therapies are also attractive alternatives. If the highrisk patient is an endovascular candidate anatomically, then consideration could be given to the application of endovascular graft placement as a definitive treatment option. Graft-related complications after abdominal aortic aneurysm repair: reassurance from a 36-year population-based experience. Secondary aortoenteric fistula: contemporary outcome with use of extraanatomic bypass and infected graft excision. Emergent endovascular treatment of a bleeding recurrent aortoenteric fistula as a "bridge" to definitive surgical repair. Outcome after endovascular stent graft repair of aortoenteric fistula: a systemic review. Management of secondary aorto-enteric and other abdominal arterio-enteric fistulas: a review and pooled data analysis. The graft is prepared as the operation ensues because there is a defined thawing process when preparing a cryopreserved allograft. Slits to enlarge the circumference of the proximal portion of the graft may have to be made to accommodate the anastomosis because of size discrepancy. The graft is rotated so that the lumbar orifices are positioned anteriorly; each lumbar artery is oversewn with interrupted 4-0 polypropylene suture. With the approaches outlined in this chapter, morbidity and mortality can be reduced (mortality <20%), and a durable, infection-resistant, limb-saving reconstruction can be accomplished. Most true aneurysms of the lower extremities are degenerative in nature, while pseudoaneurysms are related to anastomotic, traumatic, and mycotic etiologies. Common risk factors for aneurysm formation include male sex, older age, smoking, and hypertension. Approximately 40% of patients are asymptomatic at the time of diagnosis, another 40% present with signs of lower extremity ischemia from embolization of mural thrombus or thrombosis, and 20% have local pain or notice a groin mass. Catheter-based angiography has limited ability to assess the presence of an aneurysm because it only demonstrates the lumen of an artery and may miss the diagnosis in aneurysms lined with smooth mural thrombus. However, it is generally not advisable to completely excise large aneurysms because they may be adherent to the common femoral/femoral veins and femoral nerve/branches. Excision of large aneurysms can also lead to more lymphatic disruption, which can induce troublesome lymphedema of the involved extremity postoperatively. Bilateral lower extremity perfusion should also be evaluated with segmental pressure testing. Efforts should be made to preserve these branches to avoid local groin wound ischemic complications. In addition, care should be exercised in searching for (and dividing, in most cases) the crossing iliac circumflex vein, also known as "the vein of pain," to avoid later inadvertent injury. Failure to control this branch before opening the aneurysm can lead to troublesome back-bleeding. Clinical presentation Anastomotic aneurysms typically present >5 years after the original bypass surgery. The diagnosis is suggested by the complaint of a painless pulsatile mass in 6070% of patients and symptoms of acute limb ischemia in another 20%. Patients may also present with a clinical picture suggestive of graft infection, such as groin erythema, pain, fever, chills, or night sweats. In the groin, this most commonly occurs at the femoral anastomosis of an aortofemoral bypass. Careful analysis, however, suggests that degeneration of the femoral artery wall is a more important contributory factor. Symptoms can be pain from expansion/ rupture, ischemia from thrombosis or embolization of mural clot, or venous obstruction/deep vein thrombosis from compression of the adjacent vein.
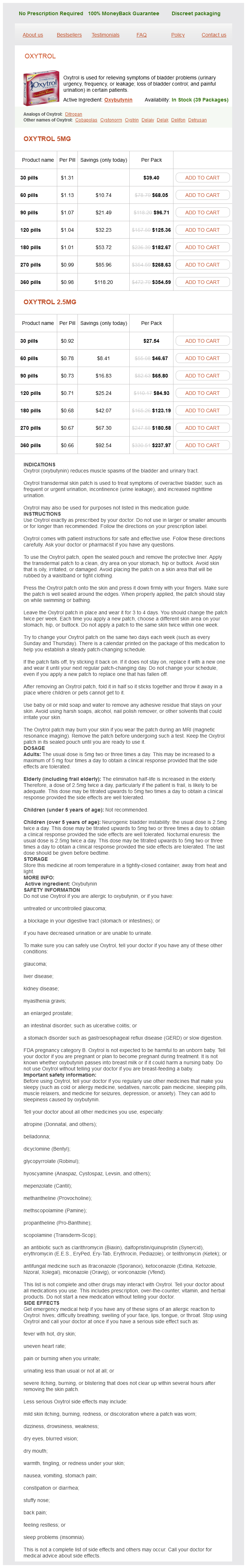
Oxybutynin Dosage and Price
Oxytrol 5mg
- 30 pills - $39.40
- 60 pills - $68.05
- 90 pills - $96.71
- 120 pills - $125.36
- 180 pills - $182.67
- 270 pills - $268.63
- 360 pills - $354.59
Oxytrol 2.5mg
- 30 pills - $27.54
- 60 pills - $46.67
- 90 pills - $65.80
- 120 pills - $84.93
- 180 pills - $123.19
- 270 pills - $180.58
- 360 pills - $237.97
A marker pigtail catheter is placed on the wire with the Iliac deployment and completion of the procedure 53 markings aligned with the docking gate of the graft and into the iliac system treatment vitamin d deficiency order discount oxybutynin on-line. The pigtail catheter is removed and the appropriate iliac limb is advanced over the supportive guidewire and into the docking section and deployed according to the roadmap image. Additional iliac components are placed at this time as needed, as in the case of a bimodular device or if additional distal iliac coverage is needed. Having deployed all components of the stent graft, a low-pressure aortic balloon is advanced through each iliac system, up into the abdominal aorta, to press the aortic graft throughout the aortic seal zone, fully expand any overlapping components, and press the iliac portions of the grafts throughout both iliac seal zones. Care should be taken not to be too zealous because even a low-pressure balloon that is aggressively overinflated can cause vessel rupture of the treated segment or device failure due to rupturing the graft material itself. Note is made of the distance from the intended landing zone within the docking section to the intended iliac landing zone. The docking section is positioned so that the iliac limbs are crossed to facilitate cannulation of the docking section. Optimization of docking section location can be performed with any of the modular type devices. If there are concerns for a type I endoleak, additional angioplasty or aortic or iliac cuff placement may be necessary. If there is concern of kinking of iliac components as they transition into the iliac arteries, additional supportive stents, either covered or uncovered, may be necessary to treat any significant dissections in the iliac arteries. Once satisfactory insertion of the stent graft has been confirmed, the sheaths and catheters are removed. If an open surgical exposure was performed, the artery access sites are typically closed primarily with polypropylene suture in a transverse manner. More severely diseased atherosclerotic arteries may require endarterectomy and patch angioplasty. After ensuring satisfactory distal lower extremity arterial perfusion, protamine sulfate may be administered. Adequate postoperative pain control is necessary and often requires the use of intravenous narcotics immediately perioperatively with a quick transition to oral analgesics. Likewise, the threshold for elective repair based on aneurysm growth rate has not been defined. Arterial degeneration remains the most common etiology with infection, anastomotic disorders, dissection, trauma, and collagen vascular disorders comprising the remainder. Others arise when the aneurysm enlarges to compress surrounding pelvic structures, such as the ureter or iliac veins, causing hydronephrosis, limb swelling, or venous thrombosis. Blood loss from iliac vein injury and intestinal or ureteral injury are significant risks of this operation. Damage to sympathetic and parasympathetic nerves, resulting in erectile dysfunction or retrograde ejaculation, are additional risks. It can be used for both primary degenerative iliac aneurysms and anastomotic pseudoaneurysms, but only as a bridge to definitive therapy in mycotic aneurysms. In addition, it provides an alternative in patients with prior abdominal or pelvic surgery or radiation, or in those at high risk because of medical comorbidities. Caution is advised in pursuing 55 56 Endovascular repair of iliac artery aneurysms an endovascular approach for patients with venous or ureteral compressive symptoms, because the aneurysm is not sufficiently decompressed immediately after endograft placement resolve these symptoms. This study will demonstrate the size and extent of aneurysmal disease, length of proximal and distal landing zones, and degrees of vessel tortuosity and calcification. More serious complications include gluteal muscle necrosis and spinal cord infarction. Note the eggshell calcification of the aneurysm sac with no contrast opacification to suggest an endoleak. Each of these can be performed simultaneously with endograft placement or in a staged fashion. Preferentially, a coaxial system consisting of a 30-cm, 5-Fr sheath, catheter, and 0. It should be preferentially occluded at its origin, proximal to the anterior and posterior divisions, to maximize pelvic collateral flow. A straight catheter is advanced over the aortic bifurcation into the superficial femoral artery. Contrast arteriography is performed to rule out technical problems, assess correct endograft positioning, and visualize any endoleaks. Iliac branch device Each of the two techniques described in the previous sections has a potential issue regarding pelvic ischemia/ buttock claudication versus distal type I endoleak. A third iteration is a bifurcated-bifurcated endograft, which consists of a single-component bifurcated main body, attached iliac limb, and iliac limb side branch. Gore & Associates) is approved for use worldwide; the Zenith Branch Iliac Endovascular Graft (Cook Medical Inc. In terms of their placement, the straight and helical devices are delivered in a 20-Fr sheath with a preloaded wire and catheter passing external to its distal portion, entering the branch ostium and common iliac segment, and exiting the sheath along a grooved pusher device. This wire is snared from the contralateral groin to establish through-and-through access. To deliver the bifurcated-bifurcated device, it is placed in the infrarenal position, and the helical branch is cannulated from the contralateral side by a fenestration opposite and superior to the branch ostium, which is later sealed by overlying endograft. Completion digital subtraction angiogram of a patent iliac branch device with no kink or endoleak. The 12-Fr sheath is in place from the contralateral side with a coaxial 7-Fr sheath for deployment of the balloon-expandable bridging stent between the iliac branch and native internal iliac artery. The contralateral limb and proximal infrarenal aortic extension are placed in the standard fashion.