Periactin
General Information about Periactin
In some circumstances, Periactin is probably not suitable for everyone. Patients with sure medical conditions, similar to glaucoma, asthma, or an enlarged prostate, ought to consult with a physician before taking this medication. It also needs to be used with caution in kids under the age of two and in older adults.
Periactin should be used with warning and based on the directions of a doctor. Like all medications, it could cause unwanted facet effects in some individuals. These can embody drowsiness, dry mouth, blurred imaginative and prescient, and constipation. It is important to monitor for any opposed reactions and converse with a well being care provider if they occur.
Allergies are a standard downside that many people face, with tens of millions of people suffering from allergic reactions yearly. These reactions happen when the immune system overreacts to a substance that is normally innocent, such as pollen, pet dander, or mud. The body releases histamine, which causes a big selection of symptoms together with sneezing, runny nose, itching, watery eyes, hives, and rashes. These signs could be uncomfortable and disruptive to day by day life, making it difficult to focus and performance usually.
In conclusion, Periactin is a generally prescribed treatment for the relief of signs of allergies and the common cold. It works by blocking the effects of histamine within the physique, offering fast aid for unpleasant signs similar to sneezing, itching, and watery eyes. While it's an efficient treatment choice, it should be used with caution and beneath the guidance of a health care provider. With the right administration, Periactin can help individuals effectively manage their allergies and improve their quality of life.
Periactin is usually prescribed by docs to alleviate these signs. It is available in each tablet and liquid type, making it straightforward to take and acceptable for all ages. It is typically taken one to a few instances a day, depending on the severity of the signs. Periactin works by blocking the consequences of histamine, effectively reducing or eliminating allergy signs. It can also assist with symptoms of the widespread chilly, such as a runny nostril and watery eyes.
With its ability to provide fast reduction and flexibility in dosage, Periactin has become a preferred choice for managing allergy signs. It can be affordable and widely out there, making it accessible to those who need it. However, you will need to note that Periactin isn't a treatment for allergy symptoms. It can only provide temporary relief of signs and ought to be utilized in mixture with other allergy administration methods, such as avoiding triggers and utilizing nasal sprays or eye drops.
Periactin, also identified by its generic name cyproheptadine, is a drugs commonly used to treat symptoms of allergies and the common chilly. It is an antihistamine, which implies it actually works by blocking the consequences of histamine, a chemical within the body that causes symptoms such as sneezing, runny nostril, and itching.
One of the advantages of Periactin is that it is a first-generation antihistamine, that means it can work rapidly and supply fast reduction. This is especially helpful for people who expertise sudden and extreme allergy signs. It may additionally be taken on an as-needed foundation, making it a versatile treatment choice for those with occasional allergies.
It results in the release of mediators like histamine allergy forecast colorado buy cheap periactin on line, prostaglandins, proteoglycans, and cytokines. Idiopathic anaphylaxis is labeled when specific allergen cannot be identified, and the serum specific IgE levels are normal. Anaphylaxis generally occurs on re-exposure to a specific antigen, but can also occur on first exposure, because there may be crossreactivity among many drugs. Other triggers of perioperative anaphylaxis include heparin, protamine, oxytocin15 local anesthetics16,17 and blood transfusion, including exposure to immunoglobulin A (IgA) in blood products in patients with severe IgA deficiency. The common sources of latex exposure in the perioperative period are those items that have prolonged contact with skin or mucosal surfaces, such as gloves, drains and catheters. Latex allergy is seen more commonly in patients with repeated exposure to latex gloves or catheters from prior surgeries, especially children with spina bifida. In a study, patients with anaphylaxis to rocuronium had cross-reactivity rates of 44% with suxamethonium, 40% with vecuronium, 20% with atracurium, and 5% with cisatracurium. Crossreactivity rates in patients with anaphylaxis to suxamethonium were 24% with rocuronium, 12% with vecuronium, and 6% with atracurium. The antibiotics included cefazolin (60%), penicillin (20%), cefuroxime (10%), and metronidazole (10%). Laryngeal angioedema, bronchospasm and cardiovascular collapse are the main manifestations of anaphylaxis in the perioperative period in an anesthetized patient. However, the patient will be at a higher risk of anaphylaxis in future surgery during re-exposure to the involved agent. Diagnosing severe anaphylaxis in the perioperative period can be difficult because hypotension, difficulty in ventilation and heart rate variation may also arise from anesthetic agents, sympathectomy associated with spinal/epidural anesthesia, surgical, or patient-related factors. Intraoperatively patients are covered with drapes and generally sedated or anesthetized and unable to report pruritus, so the early cutaneous signs of anaphylaxis might remain un-noticed. Anaphylaxis should be suspected, if there is unexplained hypotension refractory to vasopressors, or unexplained resistance to ventilation and bronchospasm. Since anaphylaxis is uncommon, there may be delay in the 124 Yearbook of Anesthesiology-6 diagnosis by anesthesiologist in the perioperative period and the management training on a full-scale anesthesia simulator is suggested. In a study, none of 42 anesthesiologists tested on a simulator could make the correct diagnosis during the first 10 minutes of anaphylaxis, and most of them failed to have a structured plan for its treatment. If the signs appear late during the anesthesia maintenance, it suggests latex allergy, allergy to colloids, antiseptics (chlorhexidine) or dyes. This could be due to delayed absorption from skin or mucosa, drugs administration at the end of the surgery, or deflation of a tourniquet resulting in the release of allergen in the circulation. Hereditary angioedema, caused by C1 inhibitor deficiency, is a rare autosomal dominant condition that resembles anaphylaxis. The disease manifests with angioedema of the face, larynx, oropharynx, extremities, abdomen, and genitalia, and its common triggers include surgery, intubation, and anesthesia. Sole angioedema is an uncommon feature of perioperative anaphylaxis,8 and the possibility of hereditary angioedema or angiotensin-converting enzyme inhibitor (or angiotensin receptor blocker)-induced angioedema should be considered. Tryptase Measurement of serum tryptase, a protease released by mast cell degranulation, provides additional diagnostic clue and should be performed whenever feasible. Increased tryptase levels beyond 24 hours may indicate lateonset anaphylaxis, biphasic reaction, or underlying mastocytosis or clonal mast cell disorders. Perioperative Anaphylaxis 125 Plasma Histamine Elevated plasma histamine level correlates with signs and symptoms of anaphylaxis and are more likely to be raised than are total serum tryptase levels. Blood samples for histamine require special handling: blood should be drawn through a wide bore needle and kept cold at all times, to be centrifuged immediately, and freeze the plasma promptly. Urine Histamine Histamine and its metabolites can be detected in the urine after anaphylaxis and the increased levels are more specific than increase in plasma histamine for anaphylaxis. Airway Airway should be secured immediately and high flow oxygen should be given if there are signs of respiratory distress. Intubation could be difficult in patients in whom the upper airway anatomy is edematous and distorted. Repeated failed attempts can lead to complete airway obstruction and may be fatal. The main factor associated with mortality by anaphylaxis is the delay in epinephrine administration. It is b-1 adrenergic agonist effects result in increased inotropic and chronotropic effects on heart. The b-2 adrenergic agonist effects result in bronchodilation and also has inhibitory effects on the release of inflammatory mediators from basophils and mast cells. Excessive administration on the other hand, can cause ventricular arrhythmias, pulmonary edema, and hypertensive crisis. Response to epinephrine may be suppressed in patients on beta-blockers, angiotensin-converting enzyme inhibitors, or those who have a spinal blockade. In patients taking beta-blockers, glucagon can be given to treat hypotension because its inotropic and chronotropic effects are not mediated through beta receptors. Beta-adrenergic agonists such as salbutamol or nebulized epinephrine can be used to treat bronchospasm. Sugammadex, a reversal agent for rocuronium and vecuronium, may reverse anaphylaxis triggered by rocuronium. However, both drugs have slow onset of action and have not been shown to improve the clinical outcome.
Needling therapies in the management of myofascial pain showed no efficacy beyond that of placebo [29] allergy forecast arkansas generic 4 mg periactin otc. It might be effective in the management of chronic migraine and chronic daily headaches; however, its efficacy in myofascial pain and cervicogenic headaches is still debatable [3032]. Cervical Discogenic Pain C23 provocative discography, but not at the lower levels, can reproduce cervicogenic headache [33]. Radiofrequency lesioning was shown to be effective in obtaining some pain relief for a few months in one study [34]. However, cervical disk interventions are not commonly performed because of the potential for serious complications mainly infection and vascular injury. Practical Approach to the Management of Cervicogenic Headache Cervicogenic headache is one of the most debatable and challenging areas in headache medicine. Patients usually benefit the most from a multidisciplinary approach incorporating physical therapy, pharmacotherapy, psychotherapy (biofeedback and relaxation therapy), and the judicious utilization of interventional pain management modalities. This requires careful history and physical examination with special attention to: 1. Assessment of any tender points over the occipital nerves, suboccipital muscles, trapezius, and cervical paraspinal muscles 2. Cervical spine range of movements: flexion, extension, lateral flexion, and rotation 3. Segmental palpation of the cervical facet joints, upper versus lower facet joints · By following the above steps, cervicogenic headache can be easily differentiated from other headache disorders. Features that tend to distinguish cervicogenic headache from migraine and tension-type headache include side-locked pain, provocation of typical headache by digital pressure on neck muscles and by head movement, and posterior-to-anterior radiation of pain. Tender points over the suboccipital muscles, trapezius, and cervical paraspinal muscles; consider trigger point injections. Tenderness to palpation over the C23 joint, especially in patients with whiplash injury; consider third occipital nerve block and neurolysis. Tenderness to palpation over the lower cervical facet (C36) with increased pain on extension and lateral rotation; consider cervical facet nerve (medial branch) block and neurolysis. Tenderness to palpation over the atlantoaxial (C12) joint with increased pain on rotation of C1 over C2 while the neck is flexed; consider atlantoaxial joint injection. Patients with clinical picture of C2 or C3 neuralgia, or patients who do not respond to the above algorithm; consider C2 or C3 nerve root block and pulsed radiofrequency ablation. Stimulation of the greater occipital nerve induces increased central excitability of dural afferent input. Entrapment of the C2 root and ganglion by the atlantoepistrophic ligament: clinical syndrome and surgical anatomy. Needling therapy in the management of myofascial trigger point pain: a systemic review. Treatment of whiplash associated neck pain [corrected] with botulinum toxin-A: a pilot study. A randomized, double-blind, prospective pilot study of botulinum toxin injection for refractory, unilateral, cervicothoracic, paraspinal, myofascial pain syndrome. Cervicogenic headaches: radiofrequency neurotomy and the cervical disc and fusion. Atlantoaxial Joint: Atlantoaxial Joint Injection and Radiofrequency Ablation Samer N. Narouze 11 Cervicogenic headache is referred pain from cervical structures innervated by the upper three cervical spinal nerves. It is a fairly common cause of cervicogenic headache as it may account for up to 16 % of patients with occipital headache [1]. Distending the lateral atlantoaxial joint with contrast agent in human volunteers produces occipital pain, and injection of local anesthetic into the joint relieves the headache [1, 2]. Clinical Presentation and Physical Examination Clinical presentations suggestive of pain originating from the lateral atlantoaxial joint include occipital or suboccipital pain with little radiation, focal tenderness over the suboccipital area or over the transverse process of C1, restricted painful rotation of C1 on C2, and pain provocation by passive rotation of C1 (while flexing the neck to limit lower cervical facet movements). These clinical presentations merely indicate that the lateral atlantoaxial joint could be a possible source of occipital headache; however, they are not specific and therefore cannot be used alone to establish the diagnosis [4]. The vertebral artery is lateral to the atlantoaxial joint as it courses through the C2 and C1 foramina. The vertebral artery then curves medially crossing the medial posterior aspect of the atlanto-occipital joint to go through the foramen magnum. Therefore, during atlantoaxial joint injection, the needle should be directed toward the junction of the middle and lateral thirds of the posterior aspect of the joint. This will avoid injury to the C2 nerve root medially or the vertebral artery laterally. Atlanto-occipital joint Vertebral artery Lateral atlanto-axial joint C2 dorsal root ganglion S. Narouze Degeneration and Whiplash Injury the pathology of lateral atlantoaxial joint pain is usually either degenerative and osteoarthritic or posttraumatic in nature [5, 6]. However, the presence of osteoarthritic changes in imaging studies does not mean that the joint is necessarily painful; also the absence of abnormal findings does not preclude the joint from being painful. The only means of establishing a definite diagnosis is a diagnostic block with intra-articular injection of local anesthetic [1]. The fluoroscopy C-arm is placed over the head and neck in an anteroposterior direction, and under fluoroscopic guidance, the C-arm is rotated in a cephalad-caudad direction till the lateral atlantoaxial joint is well visualized. The needle insertion site is marked on the skin overlying the lateral third of the atlantoaxial joint. The skin is prepped and draped in the usual sterile fashion, and a skin wheel is raised with local anesthetic at the insertion site. The needle is withdrawn slightly, directed toward the posterolateral aspect of the lateral atlantoaxial joint, and advanced for a couple of millimeters.
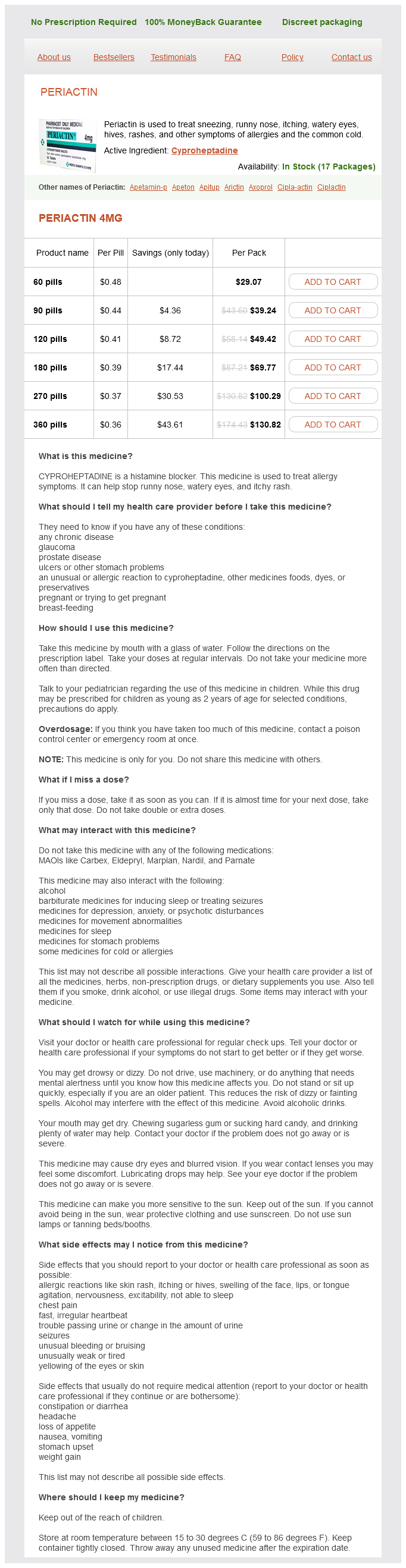
Periactin Dosage and Price
Periactin 4mg
- 60 pills - $29.07
- 90 pills - $39.24
- 120 pills - $49.42
- 180 pills - $69.77
- 270 pills - $100.29
- 360 pills - $130.82
The dorsal mesentery of the pancreas is shown as it fuses with posterior parietal peritoneum allergy symptoms from eggs periactin 4 mg buy cheap, indicated by dashed line posterior to pancreas (P). The ascending and descending mesocolons will fuse with the posterior wall of the abdomen (curved arrows) forming the colonic compartment of the anterior pararenal space. Note the subperitoneal space defined by the stippled area subjacent to the parietal peritoneum is in continuity circumferentially, within the compartments of the anterior pararenal space and the mesenteries. The fused fascia dorsal to these organs is the retroduodenal pancreatic fascia of Treitz. It is important to emphasize that the pancreas, while positioned beneath the posterior peritoneum, remains connected by the mesenteries of the subperitoneal space to the other abdominal organs. It is important to note that although the ascending and descending mesocolons have fused they remain in continuity with the other organs. The region of dorsal mesogastrium between the stomach and the transverse colon is the gastrocolic ligament. At the anatomic splenic flexure (the junction of the transverse colon and descending colon), the transverse mesocolon extends laterally to attach to the lateral abdominal wall, forming the phrenicocolic ligament. Note the subperitoneal region of the mesentery is preserved after fusion allowing continuity of the subperitoneal space. Schematic sagittal drawings showing growth and development of the dorsal mesogastrium. Fusion of the dorsal mesogastrium with the anterior border of the transverse colon forming the gastrocolic ligament. Fusion of the dorsal mesogastrium with the transverse mesogastrium as its courses from the transverse colon to the posterior body wall. Note the transverse mesocolon in the adult is the result of the fusion of the dorsal mesogastrium and the mesentery of the transverse colon. The mesenteric attachment grows correspondingly as it is carried out into the umbilical cord with the bowel loops. In this process, the cecum comes to lie on the right, the transverse colon crosses ventral to the duodenum, and the small intestine lies to the left of the ascending colon. The rotation of this mesentery occurs about the axis of the superior mesenteric artery. The focal point of the rotation is the root of the superior mesenteric artery as it originates from the aorta. The root of the small bowel mesentery finally affixes itself posteriorly and extends dorsally from the left upper abdomen to the right lower abdomen. In this manner, the root of the small bowel mesentery interconnects the upper and lower portions of the abdomen. The development of the gonadal ridge is from mesodermal epithelium lining of the posterior abdominal wall. The primordial germ cells originate from endoderm of the yolk sac and migrate along the suspending mesentery of the hindgut in the subperitoneal space. In the female, an enfolding occurs along the lateral gonadal ridge forming a paramesonephric duct. Thus, the subperitoneal space in the female extends from the extraperitoneal space to the female pelvic organs by the broad ligament. The cervix is suspended by a thickened portion of the caudal portion of the broad ligament, the transverse cervical ligament (of Mackenrodt). The illustration demonstrates the continuity of the ventral and dorsal mesenteries of the foregut; the continuity of the dorsal mesentery of the foregut, midgut, and hindgut; and the continuity of the mesenteric attachments with the remainder of the subperitoneal space. The inguinal ligament of the mesonephros forms the round ligament in the female and the gubernaculum in the male. The portion of the broad ligament extending from the ovary and fallopian tube contains the blood vessels, nerves, and lymphatics and is the suspensory ligament of the ovary. Embryology of Specific Organs Embryologic Rotation and Fixation of the Gut the final position and attachments of the mesentery differ greatly from their midline origin. Knowledge of these changes to the final form aids in the understanding of the anatomy of the peritoneal recesses and its contribution to spread of intraperitoneal disease. As a consequence, the peritoneal sac that originally lies to the right of the mesentery extends posterior to the stomach in the left abdomen. The potential space between the folds of the greater omentum is obliterated by its fusion. The more distal segment, the postarterial limb, becomes the distal ileum, appendix, and the ascending and proximal transverse colon. When the final part of rotation occurs, the prearterial limb is carried to the left upper quadrant, beneath the superior mesenteric arterial axis. The transverse duodenum (third portion) lies posterior to the superior mesenteric artery. This complex series of rotations and fixations result in the final form of mesenteric parietal attachments and peritoneal recesses. The cranial portion forms the liver and intrahepatic ducts, and the caudal portion forms the gallbladder Embryology of Specific Organs 21 the anterior pararenal space. A small portion of the tail of the pancreas near the splenic hilum remains unfused within dorsal mesogastrium. Spleen A condensation of multiple mesenchymal clusters gives rise to the spleen within the dorsal mesentery of the stomach. The portion between the spleen and the posterior abdominal wall becomes the splenorenal ligament. As the greater curvature of the stomach rotates, the mesogastrium elongates and carries the spleen to the left. It forms during the 4th6th weeks from a proliferation of cells of the coelomic mesothelium located between the root of the dorsal mesogastrium and the genital ridge.