Pletal
General Information about Pletal
In conclusion, Pletal is a valuable treatment for people suffering from intermittent claudication. It has been shown to effectively improve walking distance, scale back pain and cramping, and enhance total quality of life in patients with PAD. It is a protected and well-tolerated remedy choice, but it's important to seek the advice of with a health care provider earlier than starting this treatment. With Pletal, individuals with PAD can regain their mobility, engage in physical actions, and live a more fulfilling life.
Intermittent claudication is a standard symptom of PAD, affecting roughly 10 million folks in the United States alone. It sometimes occurs in individuals over the age of 60, and those who have underlying well being conditions like diabetes, high cholesterol, or hypertension. The symptoms of intermittent claudication may be debilitating, making it difficult for people to walk even short distances without experiencing pain or discomfort. This can significantly influence their every day activities and overall high quality of life.
Pletal is a well-tolerated medication, with minimal unwanted side effects reported. However, some sufferers could experience delicate unwanted effects, such as headache, diarrhea, and dizziness. It is also important to note that Pletal may interact with other drugs, such as blood thinners and sure heart medicines, so it is important to consult with a physician before starting this remedy.
Apart from bettering strolling and lowering pain, Pletal has additionally been found to have other constructive effects on sufferers with PAD. It has been proven to enhance blood circulate to the legs, reduce the formation of blood clots, and improve the pliability of the arteries. This is important as PAD is commonly associated with an elevated threat of cardiovascular occasions, similar to coronary heart assaults and strokes.
Pletal, also referred to as Cilostazol, is a medicine used to treat a condition known as intermittent claudication. It is a peripheral arterial disease (PAD) characterised by a narrowing of the arteries in the legs, which might result in decreased blood move and oxygenation to the muscular tissues. This can outcome in ache, cramping, and weak spot within the legs, especially throughout bodily actions, such as walking. Pletal works by growing blood circulate to the legs, lowering the frequency and severity of those symptoms.
Pletal, a phosphodiesterase inhibitor, has been accredited by the United States Food and Drug Administration (FDA) for the therapy of intermittent claudication. It works by dilating the blood vessels, lowering clot formation, and increasing blood circulate to the legs. This leads to improved oxygenation to the muscle tissue, lowering the frequency and severity of pain and cramps.
Research has proven that Pletal is effective in enhancing strolling distance, pain-free walking distance, and general physical operate in patients with intermittent claudication. One examine discovered that Pletal improved the typical pain-free strolling distance by 52% in participants in comparison with those on a placebo. It also showed a major enchancment in the general high quality of life of patients, with decreased limitations in day by day activities and an increased ability to interact in physical actions.
A semifluid substance is excreted from the outer cells and is collected in a cavity muscle relaxant orphenadrine order generic pletal, which forms simultaneously. One layer of ectodermal cells, the primitive trophoblast, covers it except at one pole where the rapidly dividing cells have formed the "inner cell mass," which constitutes the beginning of the embryo. Most of the time, in monozygotic twins the zygote will split after 2 days, resulting in a shared placenta but two separate sacs (monochorionic diamniotic twins), occurring 60% to 70% of the time. In about 1% to 2% of monozygotic twinning the splitting occurs late enough to result in both a shared placenta and a shared sac (monochorionic monoamniotic twins). During the menstrual cycle, the ovarian hormones, estrogen and progesterone, act upon the endometrium, producing the premenstrual mucosa, which is sloughed or cast off during menstruation but remains when fertilization occurs. The pregravid endometrium gradually undergoes further changes to become the early decidua to which the blastocyst rapidly adheres once it has reached the uterus. By the invasive capacity of its trophoblastic cells, the blastocyst sinks into the endometrium, which then closes over it and seals it from the uterine cavity, forming the decidua capsularis. During the period of migration and implantation of the blastocyst, marked cellular proliferation has been taking place in the embryonic area. After implantation, mesodermic cells grow out beneath the primitive trophoblast, which, by proliferation, forms villous projections into the surrounding decidua. These decrease in number as pregnancy progresses and are difficult to find after the third month of gestation. Emerging evidence suggests that during this period the foundations of a successful pregnancy and even the future health of the adult individual are set. Most patients do not have any specific signs or symptoms of implantation, although it is not uncommon to experience light bleeding at implantation or cramping during the first trimester. Some women will experience cramping during their first trimester, though this is usually of little concern unless there is bleeding as well. During this phase, the developing embryo is most sensitive to exposures to toxins, medications, radiation, and the effects of maternal condition that can disrupt the development process. Errors may result in major disruptions in structure or function of the fetus, or the complete loss of the pregnancy. Later exposures to teratogens can result in a constellation of malformations related to the organ systems that are developing at that time; cardiovascular malformations tend to occur early in the embryonic period, genitourinary abnormalities tend to result from later exposures. At the start of the third month of gestation, the risk of miscarriage decreases sharply, all major structures including hands, feet, head, brain, and other organs are present, and they continue to grow and develop. The fetal heart can be seen beating on ultrasonography, and the fetus bends its head and also makes general and startle movements. During this trimester, the risk of pregnancy loss dramatically lessens and levels of human chorionic gonadotropin plateau and often decline, easing many of the early adverse symptoms of pregnancy such as breast tenderness and morning sickness, though the enlarging uterus may now precipitate heartburn and constipation. Despite the relative lack of complications during the second trimester, early signs of later problems may first appear during this phase of pregnancy. Although the fetus begins moving during the first trimester, it is not until the second trimester that movement of the fetus ("quickening") is felt. This typically happens around 20 to 24 weeks for first pregnancies and as early as 16 to 18 weeks for experienced mothers. Fetal and maternal changes are frequent during the second trimester: During this period, the fetus changes from a lightweight, weighing about 100 g and measuring 3 in. There is an increase in maternal blood volume and cardiac output (20% greater) to feed the needs of the growing pregnancy. The placenta is fully functional, taking over the role of making estrogen and progesterone that had been performed by the corpus luteum. By the early portion of the second trimester, the external genitalia have formed sufficiently that they can be recognized on ultrasonographic studies, distinguishing the fetus as male or female. It is also at this point that a female fetus will have the most egg cells of any point in her life. Screening for open neural tube and other defects (via measurement of maternal serum -fetoprotein and other markers) is generally performed between 15 and 20 weeks. It is most often during this phase of pregnancy that complications such as preeclampsia, bleeding, complications of diabetes or hypertension, abnormalities of growth or amniotic fluid, and preterm labor may emerge. During the third trimester of gestation, the dramatic growth of the fetus continues as it attains its final birth weight and its organs prepare for function as an autonomous individual. Fetal fat accumulates to provide nutrition and insulation for the first few days of independent life, accounting for about 15% of fetal weight at term. As the uterus grows, displacement of the abdominal contents results in early fullness with meals, heartburn, and constipation. This results in low back pain and the characteristic "duck waddle" of late pregnancy. Normal amounts of colostrum have been present from the beginning of this trimester, and some women experience breast leakage throughout, this period. In general, the detection of more than four fetal movements over the course of an hour indicates a healthy fetus. Because placental function declines after 40 weeks, testing of fetal and placental reserve through fetal nonstress testing, contraction stress testing, biophysical profiles, or measurements of fetal blood flow in various vessels may be indicated when there are complications of pregnancy or it extends beyond term. It does this by establishing the placenta, an efficient interface between its vascular system and that of its mother. In the rare instances when decidual cells fail to develop, implantation overlies an old scar or there are defects in the development of the fibrinoid layer (Nitabuch layer), invasion of the uterine wall by chorionic villi is extensive. This is the yolk sac (not illustrated), the function of which in mammalian development is not known. As the embryo grows, the yolk sac decreases in size, until at term only a minute remnant can be found near the site of the cord attachment to the chorionic plate. During the first 3 weeks after implantation, a luxuriant growth of the rudimentary villi over the entire blastodermic vesicle occurs, developing into a structure called the chorion frondosum or "leafy chorion.
A careful application of secure penile dressing can prevent postoperative complications infantile spasms 2012 discount pletal 50 mg online, such as hematoma and edema, and may additionally reduce parental anxiety. It is critical to keep the reconstructed meatus moist and free of dried up secretions by generously applying a petroleumbased ointment for several weeks. In these instances, one must consider doing a complete revision of neourethra with alternative tissue sources, such as the oral mucosa. Bleeding from the exposed spongiosal tissues, either from glans, corpus spongiosum, or corpus cavernosum, should not be managed with aggressive cauterization, not only because of ineffectiveness in stopping the bleeding 890 hypospadias Infection True skin infections with cellulitis are uncommon after hypospadias repair. The first principle is to properly inform the patient and family about the problems and likely etiologies, plan for correction, and potential complications. The second principle is to recognize any related anatomic features, such as penoscrotal transposition and chordee, as well as any available viable tissues not only for neourethra formation and penile skin coverage but also vascular supporting tissues for covering the neourethra. At times, planning a staged approach, correcting chordee, and debriding unhealthy local tissues before proceeding with neourethra reconstruction, may be prudent. Third, the neourethra must be reconstructed from robust, mucosalined tissues with an excellent potential for neovascularity (most likely this will be oral mucosa). Again, if a significant portion of urethra is unhealthy or ischemic, it is better to perform a revision urethroplasty using an oral mucosa graft. Early strictures are best managed by gentle dilation and intermittent catheterization. More severe strictures, particularly along the course of the urethra, may be corrected by a dilation technique or internal urethrotomy using either endoscopic knife or laser. Generally speaking, if the strictured segment is long and is surrounded by dense periurethral fibrosis, the above-mentioned minimally invasive techniques are ineffective, and the stricture is prone to recur. It is advised that in these situations, one should consider a revision urethroplasty using oral mucosa. Placing an oral mucosa graft dorsally against corpora cavernosal bodies will minimize the risk of fistula formation. Many testes not in the scrotum at birth descend by 12 weeks after birth, so that by three months of age the incidence of congenital undescended testes is approximately 12 percent. Primitive germ cells migrate from the yolk sac in the sixth week of gestation, as the gonad in the male develops into a testis. The key structure in controlling the process is the gubernaculum, which is the embryonic ligament anchoring the testis and urogenital ridge to the inguinal region. The gubernaculum enlarges in the first phase to anchor the testis near the inguinal region as the embryo enlarges between 10 and 15 weeks of gestation. In the second phase, which occurs between 28 and 35 weeks of gestation, the gubernaculum migrates through the inguinal canal, across the pubic region, and into the scrotum. The main hormone controlling the first phase is the homolog of insulin and relaxin, known as insulinlike hormone 3 (Insl3). In the second phase, testosterone acts apparently indirectly via the genitofemoral nerve, which supplies the gubernaculum and scrotum. Recognizable hormonal syndromes, however, are rare causes of cryptorchidism in clinical practice. Many undescended testes are located in the superficial inguinal pouch, the subcutaneous space arrest just above and lateral to the external inguinal ring containing the processus vaginalis (with its contained 892 orchidopexy testis). This is the most common position for an undescended testis and is not categorized as ectopic. These testes are located in the scrotum by 12 weeks of age, but later in childhood retract out of the scrotum, and often have an exaggerated cremaster reflex. Actually, in most cases, the spermatic cord fails to elongate normally, while the distance between the inguinal canal and scrotum doubles with growth during the first decade. If the testis is near the top of the scrotum, regular follow up is required to make sure that it does not ascend out of the scrotum with time. Those with less experience would be wise to delay surgery to the older end of the range, rather than to attempt orchidopexy in a young infant, to avoid testicular atrophy. Magnification should be mandatory for surgery in babies less than one year of age. Indications Surgery is recommended for three common reasons: abnormal fertility, a risk of testicular tumors in adult life, and the obvious cosmetic abnormalities. Although many undescended testes have patent processus vaginalis, this is an uncommon presentation for an inguinal hernia. Trauma and torsion in undescended testes are more common than when the testis is descended, although these are unlikely indications for surgery. Germ-cell development in cryptorchidism is normal in the first six months, but then becomes abnormal subsequently due to secondary degeneration. This is caused by the testes residing at a higher temperature (3537°C) than when in the scrotum (33°C). With the current practice of recommending surgery at a much younger age, it is hoped that the cancer risk in the next generation will be lower, although this is unproven. Evidence is now emerging that acquired cryptorchidism has a much lower risk of subsequent malignancy. No premedication is usually required, although an oral preparation would be preferable to intramuscular injections. On admission to the day surgical unit, anesthetic cream containing lidocaine (lignocaine) and prilocaine is applied to the back of the hand so that intravenous access can be obtained without pain. An ilioinguinal nerve block, local anesthesia, or caudal anesthesia is provided to control pain for the first 46 hours after operation. Povidone-iodine, or other appropriate antiseptic, is painted on the skin from the umbilicus to below the scrotum and perineum.
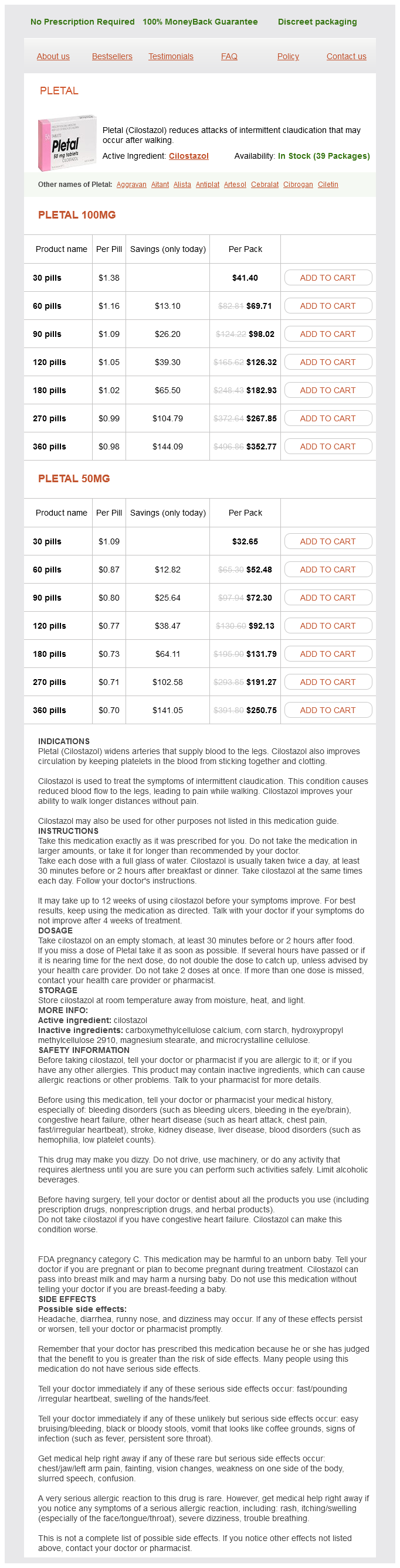
Pletal Dosage and Price
Pletal 100mg
- 30 pills - $41.40
- 60 pills - $69.71
- 90 pills - $98.02
- 120 pills - $126.32
- 180 pills - $182.93
- 270 pills - $267.85
- 360 pills - $352.77
Pletal 50mg
- 30 pills - $32.65
- 60 pills - $52.48
- 90 pills - $72.30
- 120 pills - $92.13
- 180 pills - $131.79
- 270 pills - $191.27
- 360 pills - $250.75
Congenital stricture of the meatus causes dysuria and small ulcerations at the urethral meatus back spasms 39 weeks pregnant cheap 100 mg pletal visa. Congenital urethrorectal fistula, in which a communication exists between the membranous urethra and the rectum, is also very rare and is usually associated with imperforate anus. Acquired diverticula are frequently observed in spinal cord injury patients who develop painless, undetected periurethral abscesses from chronic urethral catheters. Acquired pseudodiverticula are frequently found in the posterior urethra following instrumental trauma, whereas congenital diverticula are almost always located on the ventral wall of the anterior urethra. Diverticula are rarely asymptomatic and are best treated by complete excision and reconstruction of the urethral channel. When found dorsal to the true urethra, they are termed epispadiac duplicated urethrae. Congenital hypertrophy of the verumontanum is probably caused by maternal estrogens. It may be quite enlarged in young children and may nearly obstruct the prostatic urethra. Obstructive urinary symptoms such as stranguria and urinary frequency occur, until overflow incontinence develops. This form of incontinence in this age group can often be confused with benign enuresis. Surgical removal of the histologically normal but enlarged verumontanum by transurethral resection is usually curative but renal damage may persist. Verumontanitis, or inflammation of the verumontanum, is usually due to underlying inflammation from chronic prostatitis, urethritis, or seminal vesiculitis. Verumontanitis in adults can provoke abnormal sexual symptoms, such as pain with ejaculation or hematospermia, and can cause urinary symptoms such as frequency and urgency. The ejaculatory ducts may be obstructed, leading to seminal vesicle dilation and pain radiating to the low back, perineum, scrotum, and rectum. The diagnosis is generally made by urethroscopy and treatment is directed at the underlying obstructive or inflammatory condition. If the foreskin is not retracted during early childhood and the congenital adhesions are not released, complete fibrous bands can develop between the prepuce and glans penis. When adhesions are present proximal to the glans corona, the preputial cavity or sulcus behind the glans near the fold of the inner preputial skin may be obliterated. These adhesions may be easily overlooked if the foreskin is partially retracted, exposing just the glans and not the entire preputial sulcus. Understand, however, that men who demonstrate excellent penile hygiene have no increased risk of contracting penile cancer compared to uncircumcised men. Paraphimosis is a tight retraction of the foreskin behind or proximal to the coronary sulcus. It may result from the retraction of a congenitally phimotic prepuce or from the contraction of an essentially normal prepuce that has become swollen due to either edema or inflammation. Ulceration at the point of the constricting band may result in a release of the obstruction. With small constricting bands, the edema may become so excessive that the constricting object is not visible. Reduction of the device should be attempted before operation, as it may be possible to reduce the edema under anesthesia with constant manual pressure applied distal to the constricting ring. Less commonly, a "waist" or "hourglass" defect may exist in which one segment of the penis is narrower than the surrounding areas. In most cases, the pain will resolve with time although plaques and curvature may persist. The leading theory is that minor trauma (often unnoticed) from penile buckling during sex shears layers of the tunica albuginea and disrupts small blood vessels. The inability to drain these inflammatory mediators away from the injury leads to prolonged inflammation and fibrosis. With obstruction to flow, trapped blood increases pressure and the penile shaft becomes very hard and painful. Nonischemic priapism, also known as high-flow priapism, is rare and occurs with excessive blood flow through the penis as a result of arterial rupture within the erectile tissue, most commonly from blunt injury to the groin or pelvis. In nonischemic priapism, the penis is enlarged but not as rigid as a normal erection and there is usually less pain. This generally occurs after 48 hours of unwanted erection as thrombosis within the cavernous spaces causes fibrosis and permanent loss of function. Medical conditions associated with priapism include spinal cord injury, leukemia, gout, sickle cell anemia, and advanced pelvic and metastatic cancer. Treatment is directed at relieving the erection with corporal irrigation to remove blood clots, intracorporal injection of -agonist drugs to contract arteries, and occasionally surgical shunts to restore venous outflow. Rupture of the corpora cavernosa is rare but is encountered from direct trauma or penile fracture from vigorous intercourse or with the use of devices. Rupture of the tunica albuginea usually includes rupture of Buck fascia (see Plate 2-4), in which case the penis quickly swells as a result of extravasation of blood. Early surgical repair of the ruptured tunica albuginea may prevent thrombosis and subsequent fibrosis of the erectile tissue with consequent erectile dysfunction. Severe straddle injuries result from a blow to the perineum and bulbous urethra, usually after a fall astride a blunt or sharp object with the bulbous urethra crushed against the underside of the bony symphysis pubis.