Prandin
General Information about Prandin
One of the primary advantages of Prandin is its ability to control blood sugar levels shortly after a meal. This is particularly useful for individuals who battle with high blood sugar spikes after eating. By taking Prandin earlier than a meal, it could possibly stop these spikes from occurring and help maintain blood sugar ranges more secure all through the day.
Another advantage of Prandin is that it has a shorter period of action in comparability with other diabetes medications, which means its effects wear off faster. This may be beneficial for people with irregular meal patterns or those who may skip meals, because it allows for extra flexibility in when the treatment needs to be taken. However, it's nonetheless essential to maintain a constant schedule for taking Prandin to ensure its effectiveness.
Prandin is prescribed for patients who haven't been in a position to adequately control their blood sugar ranges through diet and exercise alone. It is typically taken earlier than meals, as it works by rising insulin manufacturing when glucose ranges rise after eating. By doing so, it helps the physique use glucose extra successfully, keeping blood sugar ranges in a wholesome vary.
Prandin, also recognized as repaglinide, is a medicine generally used for managing kind 2 diabetes. This drug belongs to a category of medicines known as meglitinides, which work by stimulating the pancreas to supply more insulin.
Type 2 diabetes is a persistent condition during which the physique both does not produce enough insulin or is unable to use it effectively. Insulin is a hormone that helps regulate blood sugar levels, and without enough of it, the body is unable to properly metabolize sugars from meals. This can lead to high blood sugar levels, causing varied well being complications over time.
Like any treatment, Prandin might cause unwanted effects in some people. The most common side effects reported embrace low blood sugar (hypoglycemia), headache, dizziness, and gastrointestinal discomfort. These unwanted effects are usually mild and could be managed by adjusting the dose or timing of the treatment. It is important to observe blood sugar ranges and report any unwanted effects to a healthcare provider.
Prandin is most likely not appropriate for everyone. Individuals with a historical past of liver disease, kidney illness, or sure kinds of heart situations should use warning when taking this medicine. It is important to tell a healthcare supplier of any pre-existing circumstances or different medications being taken before starting Prandin.
In conclusion, Prandin is an effective medicine for managing kind 2 diabetes. By stimulating the pancreas to provide more insulin, it helps the physique use glucose more effectively and retains blood sugar levels in a wholesome range. Although it may trigger some side effects, these can usually be managed with proper monitoring and changes. As all the time, it is important to observe a healthcare supplier's instructions and keep a healthy lifestyle while taking Prandin to realize optimal leads to managing diabetes.
Migrating panniculitis diabetes in senior dogs buy 2 mg prandin fast delivery, although rarely reported, is distinctive and perhaps pathognomonic: substantial, tender, subcutaneous nodules vanish after 1 or 2 weeks [3,5]. A wandering larva causes an ocular granuloma simulating a neoplasm or may simulate a more vigorous inflammatory reaction such as that seen in uveitis [6]. Incidence and prevalence Human gnathostomiasis occurs throughout SouthEast Asia, east of and including Bangladesh, China, Japan, Indonesia and the Philippines. There are also reports from Mexico, Guatamala and Ecuador and in travellers returning from any endemic area [1,2]. Investigations/diagnosis Diagnosis is reliably confirmed by biopsy of the liver or of a cutaneous nodule. Molecular methods also show promise in distinguishing between the main pathogens [8] but are not used in practice. Pathophysiology Pathology Larvae ingested by humans wander, mainly in subcutaneous tissues and muscles, causing deep tunnels, which form the sites of episodes of inflammation or abscess formation. Histology shows intense infiltration with neutrophils, plasma cells, chronic inflammatory cells and especially eosinophils. Individuals with mild symptoms may not require treatment, since they typically resolve in a few weeks. For patients requiring treatment, albendazole may prove to be the best agent [9]; in the case of ocular infection, vitrectomy is often combined with medical treatment. In cases with central nervous system involvement, concominant prednisolone is warranted. Eggs are passed in the faeces, hatch in water and are ingested by a species of Cyclops, in which they transform further. Humans are infected either by ingesting Cyclops in water or by eating inadequately cooked flesh of an intermediate host. Worms removed from a person are most commonly thirdstage larvae or immature adults, which measure 24 mm long and are rust brown in colour due to ingested blood. They are firm, warm, red and painful, and last up to 4 weeks, before disappearing figure 33. Head of an adult worm that was extruded from a subcutaneous swelling in a patient from Bangladesh. Differential diagnosis Other nematodes that may cause similar clinical pictures include Lagochilascaris minor, a cause of subcutaneous abscesses in Surinam and Central America; Thelazia callipaeda, which parasitizes the conjunctival sac in the Far East; and Gongylonema pulchrum, a cosmopolitan parasite of pigs, bears, hedgehogs and monkeys that causes migratory lesions in the oropharyngeal submucosa of humans [5]. Isolated swellings may simulate inflammatory or neoplastic disease of other internal organs. Part 3: InfectIons & InfestatIons Complications and comorbidities Fatal encephalomyelitis has also been described [6]. It shows degenerate coiled Dirofilaria worm within an abscess, and surrounding lymphocytic infiltrate and fibrosis. Pathophysiology Causative organisms management Albendazole in a dose of 400 mg/day for 21 days or ivermectin 200 g/kg at a single dose are effective [7]. Dirofilariasis Definition Dirofilariasis is an infection by filarial nematodes of the genus Dirofilaria. Investigations Diagnosis is made by extracting the worm from the lesion, or by identifying it in an excised specimen [1]. Encysted larvae of Trichinella spiralis are ingested in meat, hatch in the duodenum, penetrate the submucosa and within 5 days have matured and mated and started producing 200 2000 invasive larvae, which reach muscles where they become encysted and infective to a fresh host within 21 days. Cysts may calcify, but the larvae remain viable for many years and can outlive their dead host by 10 days [1]. These are followed within a week by an acute illness with fever, generalized muscle pain and tenderness; sweating; periorbital oedema; conjunctivitis; some paralysis of the muscles of the tongue, jaw and respiration; a transient maculopapular rash of the extremities; and splinter haemorrhages beneath the nails. Pathophysiology Predisposing factors Humans acquire the disease by eating raw or undercooked meat infected by Trichinella spiralis such as bush pig in Africa, polar and black bear meat in Alaska and the Arctic. Clinical variants In severe infections, there is involvement of the heart and central nervous system. A necrotizing vasculopathy equivalent to classic polyarteritis nodosa is described [2]. Pathology Intestinal infection causes partial villous atrophy and mucosal and submucosal inflammation. The coiled larvae are surrounded by an inflammatory infiltrate of lymphocytes and macrophages until they become encapsulated. Investigations Clinical features can suggest the diagnosis within a week of eating inadequately cooked meat, especially pork. Worms may be found in faeces in the second to fourth week of the infection, and after 4 weeks in biopsied muscle. The eosinophil count, erythrocyte sedimentation rate and serum creatine phosphokinase are all raised. Symptomatic therapy aimed at fever and pain reduction can be achieved with analgesia and antipyretics. Management of the disease with systemic symptoms including central nervous system involvement, cardiac inflammation or pulmonary infiltration consists of combined use of a corticosteroid and an antiparasitic agent. Corticosteroids are life saving in suppressing allergic reaction at the height of larval spread. Mebendazole and albendazole reduce the severity of infection if given early enough in the acute disease, but albendazole is possibly more effective [4,5]. However, once the parasites are encysted in muscle, antiparasitics are ineffective.
Clinical features Lesions confined to the skin and subcutaneous tissues are generally located on exposed sites diabetes vs hyperglycemia purchase prandin 1 mg online, and may be associated with trauma [2,3]. Papules, nodules, ulcers and multiple granulomatous lesions have all been described. Colonization of nails has been reported, and Prototheca may occur as transients on the skin. Investigations the organisms stain with methenamine silver and appear as round, nonbudding structures 510 m in diameter. Infections caused by Pythium insidiosum Definition and nomenclature Infections caused by Pythium species were first recognized in animals in 1884, affecting mainly horses and mules. Since 1987, a number of cases of human infection have been reported, nearly all of them from Thailand and in farmers exposed to swampy areas. Synonyms and inclusions · Swamp cancer · Florida horse leech Management Spontaneous recovery has occurred in one cutaneous infection. However, surgical excision is recommended for localized lesions, and systemic amphotericin B, ketoconazole [5] or itraconazole have proved effective on occasions. Glossary of terms Anamorph Anthropophilic Arthroconidium Asexual An asexual state. A spore resulting from the breaking up of a hypha into separate cells; characteristic of the parasitic form of ringworm fungi. Fusarium and, more rarely, Acremonium infection may produce targetlike lesions, which may undergo central necrosis. In some cases of Fusarium infection, scattered skin lesions have been accompanied by digital cellulitis and superficial white onychomycosis caused by the same organism. Skin involvement has also been described in a variety of invasive infections affecting the paranasal sinuses such as those caused by Exophiala dermatidis. The response rates in both Fusarium and Trichosporon infections are low, and a lipidassociated amphotericin B formulation is often used instead. Pathophysiology the organisms appear to invade blood vessels with large, sparsely septate hyphae, 320 m in diameter, similar to those seen in zygomycosis. It is now recognized, however, that the organism is not a true fungus and is probably more closely related to the algae. A thickwalled cell, intercalary or terminal containing stored food and able to function as a spore. Having two distinct forms, which often correspond to saprophytic and parasitic phases, respectively. Dermatophyte hair infection with hyphae inside the hair and a sheath of spores outside the hair. One of the branching filaments, septate or nonseptate, that make up the vegetative mycelium of moulds. The larger of the two types of conidia in those fungi that bear large and small (microconidia) spores. The smaller of the two types of conidia in those fungi that bear large (macroconidia) and small spores. Strictly having two or more forms; used frequently to describe nonsporing (sterile) cultures of dermatophytes. Skin disease caused by Malassezia species Pityriasis versicolor 11 Crespo Erchiga V, Delgado Florencio V. Other cutaneous disorders associated with Malassezia yeasts 8 Crespo Erchiga V, Delgado Florencio V. Helminths, including nematodes, may be long lived up to 30 years for Schistosoma spp. All nematodes must spend part of their life cycle outside the human body, either on soil or in water, or in an insect, crustacean or vertebrate intermediate host. Strongyloides stercoralis is the exception to this rule: autoinfection with this worm permits lifelong infections in humans. With some species of nematode, the worm is masked from immune recognition, and large worm burdens may be tolerated with remarkably little clinical effect. With others, inflammation, often in response to naturally dying worms or their progeny, causes severe disease. A summary of the organisms and diseases caused by infection with human nematodes is provided in Table 33. The disease is second in the world to trachoma as an infectious aetiology of blindness. The disease typically affects rural communities and is a major cause of blindness and cutaneous disease, most notably in subSaharan Africa [1]. Fewer cases have been identified in Yemen, Central America, Mexico, Columbia, Ecuador and Venezuela. Part 3: InfectIons & InfestatIons Pathophysiology Pathology [3,4] Mature worms and microfilariae are found in granulomatous dermal nodules (onchocercal nodules), often situated on the scalp of their hosts in Central America, but in Africa near bony prominences on the trunk and limbs or in the natal cleft. The nodules measure some 335 mm in diameter, and consist of an outer layer of fibroblasts, which contains the parasites in an organized fibrinous exudate. The longer the disease lasts, the more these changes are replaced by fibrosis and atrophy of dermis and epidermis [4,5]. In some instances, there is a dense predominantly perivascular reaction with mononuclear cells and eosinophils, but few microfilariae [6]. The reason for this extreme reaction is unknown, but serum from patients with this form of onchocerciasis recognize a collagen antigen expressed by a specific nematode gene, which suggests that crossreaction between antibodies to Onchocerca and human collagen might play a role in the pathogenesis of this condition [7]. In these patients, there is evidence of defective Tlymphocyte stimulation by certain filarial antigens, which can be reversed by treatment [8].
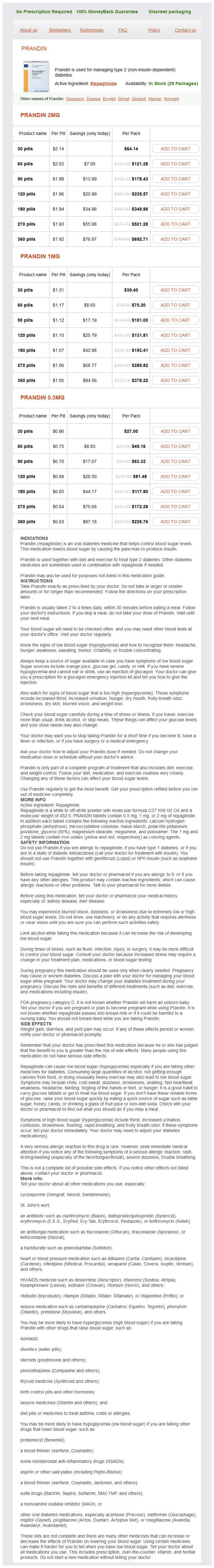
Prandin Dosage and Price
Prandin 2mg
- 30 pills - $64.14
- 60 pills - $121.28
- 90 pills - $178.43
- 120 pills - $235.57
- 180 pills - $349.86
- 270 pills - $521.28
- 360 pills - $692.71
Prandin 1mg
- 30 pills - $39.40
- 60 pills - $70.20
- 90 pills - $101.00
- 120 pills - $131.81
- 180 pills - $193.41
- 270 pills - $285.82
- 360 pills - $378.22
Prandin 0.5mg
- 30 pills - $27.00
- 60 pills - $45.16
- 90 pills - $63.32
- 120 pills - $81.48
- 180 pills - $117.80
- 270 pills - $172.28
- 360 pills - $226.76
Attention to the patient as a whole is an essential part of the proper management of any cutaneous tuberculous lesion and involves a careful search for an underlying focus of disease and coexistent infections diabete mellitus type 2 prandin 0.5 mg line. Because of the rising incidence of drugresistant tuberculosis, it is vital to confirm the diagnosis bacteriologically whenever possible and to obtain drug susceptibilities [3]. Drug therapy Treatment of cutaneous tuberculosis should follow the same drug regimen as that for systemic tuberculosis [4]. Rifampacin can commonly cause elevated serum transaminases, during the first 2 months of treatment, but therapy can usually be continued except in severe cases. The induction of liver enzymes by rifampicin may reduce the effectiveness of oral contraceptives. Pyrazinamide causes hepatitis in 1%, and arthritis and the precipitation of gout and cutaneous hypersensitivity in 3. Ethambutol may cause visual disturbances and rarely a retrobulbar neuritis, which is reversible if detected early. Patients should be warned of this risk and advised to stop the drug if visual symptoms develop. Visual acuity using a Snellen chart should be carried out before treatment starts. Reactions were significantly more common in those not receiving standard antituberculosis chemotherapy [13]. This is defined as resistance to rifampicin and isoniazid with or without resistance to other antituberculous drugs, and is now a worldwide problem [14,15]. Such patients who are sputum smear positive remain infectious for much longer than those with susceptible organisms and have a higher death rate from, and a lower cure rate for, their tuberculosis [5]. Globally in 2012, data from drug resistance surveys and continuous surveillance among notified tuberculosis cases suggest that 3. There have been important breakthroughs in tuberculosis diagnostics in recent years. Treatment of such patients is complex, and is difficult in many developing countries that lack adequate primary care facilities and the necessary tools to detect drug resistance promptly. Ideally, treatment should only be carried out by experienced physicians in hospitals with appropriate isolation facilities and in consultation with appropriate mycobacterial reference laboratories [5,8]. Yates and Ormerod have shown that the standard 6month regimen is effective in treating cutaneous tuberculosis [4]. In their series of patients, over 50% had coexisting disease elsewhere, all had a good clinical response and there were no relapses following treatment. Historically, some forms of skin tuberculosis have been treated by isoniazid alone [20]. This is no longer appropriate as drug resistance is likely to develop with monotherapy and if drug resistance to isoniazid is already present, it means, in effect, that no therapy is being given. The excision of small lesions of lupus vulgaris or warty tuberculosis, if diagnosed early, may be effective. Surgery may be helpful in scrofuloderma, sometimes shortening the time needed for chemotherapy. When tuberculosis has become generalized or has affected the meninges, the prognosis must be doubtful. Tuberculosis confined to the skin usually responds well to multiple therapy and a clinical response will usually occur within 46 weeks, with lupus vulgaris showing a faster response time than scrofuloderma. Calmette and Guerin, at the Pasteur Institute in Lille developed the vaccine from 1908 onwards using in vitro attenuation by repeated passage of an isolate of M. Unusual reactions have also occurred, such as generalized maculopapular or purpuric eruptions associated with arthralgia and abdominal pain or myalgia, usually after repeated vaccination [14,15]. This can be a recurrent problem [19] and is more likely to occur after multiple vaccinations [20]. Disseminated cutaneous granulomas have been noted in infants with immunodeficiency syndromes [26,27]. The relatively lower risk of tuberculosis with etanercept may be particularly relevant for Asia, an endemic area for tuberculosis [13]. Part 3: InfectIons & InfestatIons primary inoculation tuberculosis Definition and nomenclature A tuberculous chancre is the result of the inoculation of M. Synonyms and inclusions · Tuberculous chancre · Tuberculosis primary complex Introduction and general description figure 27. Ribera, Hospital Universitari Germans, Universitat Autònoma de Barcelona, Badalona, Spain, and the Editor of the British Journal of Dermatology. Miliary tuberculosis has been reported [5,6] and reactivation has also occurred during antibiotic prophylaxis [7]. Some form of injury is mandatory for the initiation of the infection, as the tubercle bacillus cannot penetrate the normal intact skin or mucosal barrier. The bacillus enters the skin through abrasions and minor injuries, usually on the face or limbs and commonly in children. The disease also occurs in at risk occupations such as healthcare workers, particularly in areas of high prevalence for tuberculosis [1,2]. Tuberculous chancres have followed ritual circumcision [3], infections with inadequately sterilized syringes and needlestick injuries [4,5,6], wounds [7], operations. In regions where tuberculosis is prevalent in the community, lesions may occur anywhere on the body from contact with sputum or following insect bites [14] or pyococcal infections of the skin.