Probenecid
General Information about Probenecid
In conclusion, Probenecid, also referred to as Benemid, is an important and efficient treatment in the treatment of gout and hyperuricemia. Its ability to prevent the formation of uric acid and cut back its ranges within the blood make it a useful device in managing this painful condition. Although it is probably not suitable for everyone, it supplies an alternative for many who can not take other gout medications, making it an essential addition to the remedy choices available for gout patients.
However, like all drugs, Probenecid has its own set of potential unwanted aspect effects, including nausea, vomiting, lack of appetite, headache, and rash. In rare instances, it can also result in more critical side effects corresponding to kidney stones and hypersensitivity reactions. It is essential for sufferers to seek the guidance of with their healthcare provider earlier than starting Probenecid and to report any unusual unwanted facet effects.
In the past, remedies for gout focused on relieving the signs of acute attacks, which generally embrace extreme ache, swelling, redness, and warmth in the affected joint. These remedies involved using nonsteroidal anti-inflammatory medication (NSAIDs), corticosteroids, and colchicine. However, these medications present only short-term aid and do not address the underlying explanation for gout.
This treatment is particularly helpful for sufferers who are unable to take other gout medicines, such as NSAIDs, due to underlying health circumstances or allergy symptoms. In addition, Probenecid has additionally been shown to be efficient in treating hyperuricemia, which is a situation where there's an excess of uric acid within the blood with out the presence of gout signs.
Probenecid is usually prescribed for long-term use, unlike different gout drugs which would possibly be used during an acute attack. This is because it takes time for Probenecid to take impact and lower the levels of uric acid within the physique. The medicine is taken in pill form and is often given in combination with other gout medications, similar to NSAIDs or colchicine, to supply immediate relief throughout a gout flare-up.
Gout is a standard and painful situation that impacts millions of individuals worldwide. It is often seen in middle-aged adults, notably males, and is caused by an excess of uric acid in the blood. Uric acid is a pure by-product of the breakdown of purines, which are substances found in certain meals and drinks. Normally, uric acid is filtered out by the kidneys and eradicated from the physique within the urine. However, in individuals with gout, the amount of uric acid produced is too much for the kidneys to handle and it begins to build up within the joints, leading to irritation and ache.
This is the place Probenecid comes in. It is a medicine that has been particularly developed to stop the formation of uric acid by blocking its reabsorption in the kidney. This action will increase the quantity of uric acid that's excreted within the urine, which in flip, reduces its ranges within the blood. By decreasing the amount of uric acid in the physique, Probenecid helps to prevent gout assaults and likewise helps to dissolve present urate crystals, which may scale back joint harm and enhance symptoms.
Probenecid, also identified as Benemid, is a medication that has been used for many years to deal with a medical condition known as gout. This condition is a form of arthritis that is caused by the buildup of uric acid crystals in the joints. Probenecid is an effective anti-gout agent that works by stopping the formation of uric acid, which in flip, helps to alleviate the signs of gout and reduce the risk of future flare-ups.
More series are confirming results at least equivalent to open procedures wellness and pain treatment center tuscaloosa buy probenecid with american express, with similar complication rates. Arthroscopic débridement and osteocapsular resection is a procedure that adequately addresses the underlying pathologic processes and is associated with early return to activities, a durable result that does not preclude future reconstructive procedures, and minimal perioperative morbidity. Less frequently, patients who depend on wheelchairs or crutches for mobility, and who thus put increased forces across their elbow joints, may be afflicted. Progressive loss of motion and pain at the extremes of motion due to impingement of osteophytes are noted. Painful crepitus and catching or locking sensations may be noted with range of motion. Patients with contracture of the posterior capsule will lack flexion, whereas those with anterior contractures will lack extension. This should be documented and will contribute to decision making regarding the need for decompression or transposition. Radiographs may show joint space narrowing, hypertrophic bony osteophytes, loose bodies, and subchondral sclerosis typical of osteoarthritis. Bony osteophytes may develop, leading to impingement in flexion and extension in degenerative conditions. These two processes cause impingement and contribute to the third process, progressive joint contractures. Symptoms include loss of extension, pain at the end points of motion, and mechanical symptoms such as catching or locking. The patient is positioned laterally with the arm secured in a dedicated armholder. Physical examination will also exclude other painful elbow conditions, such as tendinitis, instability, or cubital tunnel syndrome. Preoperative Planning Careful physical examination with attention to neurovascular status should be documented. Positioning General endotracheal anesthesia is induced and the patient is placed in the lateral decubitus position. Positioning the elbow just higher than the shoulder allows free access to the elbow. A 70-degree arthroscope may likewise be used but is usually not necessary and may be awkward unless the surgeon has experience using this arthroscope. Retractors such as a Howarth elevator or a large blunt Steinmann pin make the procedure easier and enhance visualization. The portal sites and landmarks, including the radial head, medial and lateral epicondyles, capitellum, and olecranon, should be marked before insufflation of the joint, which may obscure landmarks. The ulnar nerve should be examined and its location marked; the surgeon should watch for a subluxating ulnar nerve. Approach Patients with lack of flexion will need to have the posterior aspect of the joint addressed; patients with lack of extension will require release and débridement anteriorly. The standard arthroscopic setup and equipment includes the 4-mm 30-degree arthroscope. From left: syringe for insufflation of the joint, spinal needle, knife, hemostat for spreading to establish portal site, blunt trocar and cannula, switching stick, and blunt trocar and cannula. Howarth elevators, retractors, and large Steinmann pins are useful for retraction. Portal sites are established according to the order preferred by the surgeon; the procedure described below is our preference. The blunt trocar and sleeve are then placed into the joint and exchanged for the arthroscope. This portal is established just anterior to the sulcus between the capitellum and the radial head. The anteromedial portal is established using an insideout technique with direct visualization. The arthroscope is removed and replaced with the blunt trocar, which is pushed directly across the joint until it tents the skin overlying the medial side of the elbow. The skin is incised over this region and the trocar pushed through the remaining soft tissue. A proximal anterolateral retraction portal may be established about 2 cm proximal to the lateral epicondyle. Drawing the portal sites and palpable landmarks as well as the ulnar nerve is useful before insufflation of the joint. The anteromedial capsule is then stripped off the humerus to expand space in the contracted joint. Osteophytes are removed with the shaver and burr from the coronoid and radial head fossae. After completion of the bony débridement, the anterior capsule is completely resected under direct visualization with the arthroscope in the lateral portal site. The biter is used to gain a free edge of the anterior capsule, proceeding from medial to laterally and halting when the fat pad anterior to the radial head is encountered. The arthroscope is placed in the medial portal and bony débridement and capsulectomy is completed. It is made with the elbow in a 90-degree flexed position and is placed at the lateral joint line at a level with the tip of the olecranon.
Abnormal changes may be part of a generalized lymphadenopathy or represent a local reaction to pathology (inflammation or neoplasm) in regions whose lymphatic drainage is to the groin pain syndrome treatment cheap probenecid 500 mg on line. An assessment of inguinal lymphadenopathy must therefore include a review of constitutional symptoms and a thorough examination of the drainage basins of the inguinal lymph nodes (lower torso, lower extremity, perineum, anus, external genitalia) as well as other lymph node groups (neck, axillae). The ongoing inflammation in cases of bacterial lymphadenitis may result in the formation of an abscess. In rare cases, the retroperitoneal purulent process may dissect along the tissue planes into the groin, and mimic primary groin pathology or even a perirectal abscess. Inadequate healing and closure of the umbilical ring leads to hernia formation, which represents the most common umbilical pathology. Umbilical hernias and conditions that occur in neonates, including omphalocele (exomphalos) and neonatal omphalitis, are discussed elsewhere in the text. Inflammation of the umbilicus occurs in the setting of obesity, dermatitis, intertrigo, bacterial or fungal infections. It is primarily due to poor hygiene, but may occasionally be caused by excessive manipulation and cleansing of the umbilicus. Hernias Inflammation Umbilical Fistulas and Related Conditions Both congenital and acquired conditions can present with umbilical drainage or infection. Embryologically, the omphalomesenteric duct, connected to the midgut, and the urachus, connected to the bladder, are the elements of the umbilical cord. A patent urachus presents with intermittent drainage and occasionally urinary tract infections. The umbilicus is a weaker area of the abdominal wall through which various inflammatory processes can drain and give rise to acquired fistulas. Aetiologies described include gallstones, retained foreign bodies, fistulas from a perforated viscus and tuberculous peritonitis. Apart from post-operative enterocutaneous fistulas, this pathology is now rarely seen. The umbilicus is subject to a wide range of congenital and acquired lesions (Table 33. Umbilical Concretions and Inflammation Umbilical concretions are common in those who are obese or elderly. They are typically composed of dirt and desquamated epithelium, and their extent varies. Although much less common than in the sacrococcygeal region, pilonidal disease can affect the umbilicus and manifest with hair protruding from the sinus tract. Similar to the more common sacrococcygeal disease, the typical patient is a hirsute young man. Granulation tissue forms at the site of cord separation secondary to inflammation and usually responds to topical silver nitrate treatment. These benign lesions are firm nodules composed of residual omphalomesenteric duct epithelium and, less commonly, urachal uroepithelium; they can be diagnosed by a biopsy. Superior vena cava syndrome is accompanied by dyspnoea, oedema of the face and head fullness, which is worse in the dependent position. In rare cases when the venous collaterals become prominent on the torso, they are located on the chest and the upper abdomen, and drain inferiorly. In cases of portal venous hypertension, the blood flow is directed into the normally obliterated umbilical vein, leading to a radial engorgement of the periumbilical venous plexus (caput medusae). In portal hypertension, the direction of the venous flow on the abdomen is typically otherwise unchanged. Although it is not always accurate in mixed conditions, determining the direction of flow in a dilated vein located below the umbilicus can frequently help with the differential diagnosis: away and inferiorly from umbilicus in portal hypertension, and superiorly in inferior vena cava syndrome. A simple technique is to compress the vein with the index fingers of both hands and slide the fingers apart to empty the segment. The direction of the venous flow corresponds to the direction of the faster refill. Key Points the abdominal wall has a complex anatomy and an important physiological function. The differential diagnosis of abdominal wall lesions should include infections, hernias, haematomas, tumours and varicose veins. Benign subcutaneous tumours are typically well circumscribed and mobile relative to the underlying abdominal wall musculature and deep fascia. Malignant tumours and tumours arising from the musculoaponeurotic layers appear fixed to the abdominal wall. While periumbilical varices (caput medusae) are pathognomonic of portal hypertension, varicosities of the abdominal wall may develop secondary to occlusion of the superior or inferior vena cava. The lymphatics of the supraumbilical skin drain primarily to the axillary lymph nodes, and those of the infraumbilical regions drain to the superficial inguinal lymph nodes. Cancer of the anorectal region below the dentate line metastasizes to the superficial inguinal lymph nodes. Thus, the lower extremities, torso, anorectal area and external genitalia must be examined in cases of inguinal lymphadenopathy. Answer e Infectious and malignant lymphadenopathy cannot be differentiated based on the size and mobility of the enlarged lymph nodes. Although most rectus sheath haematomas develop in the absence of a traumatic episode, the vast majority of such patients receive some form of anticoagulation or antiplatelet therapy. Given the location under the anterior rectus sheath, bleeding may be physiologically significant and haematomas may reach a significant size even without any obvious overlying skin discoloration.
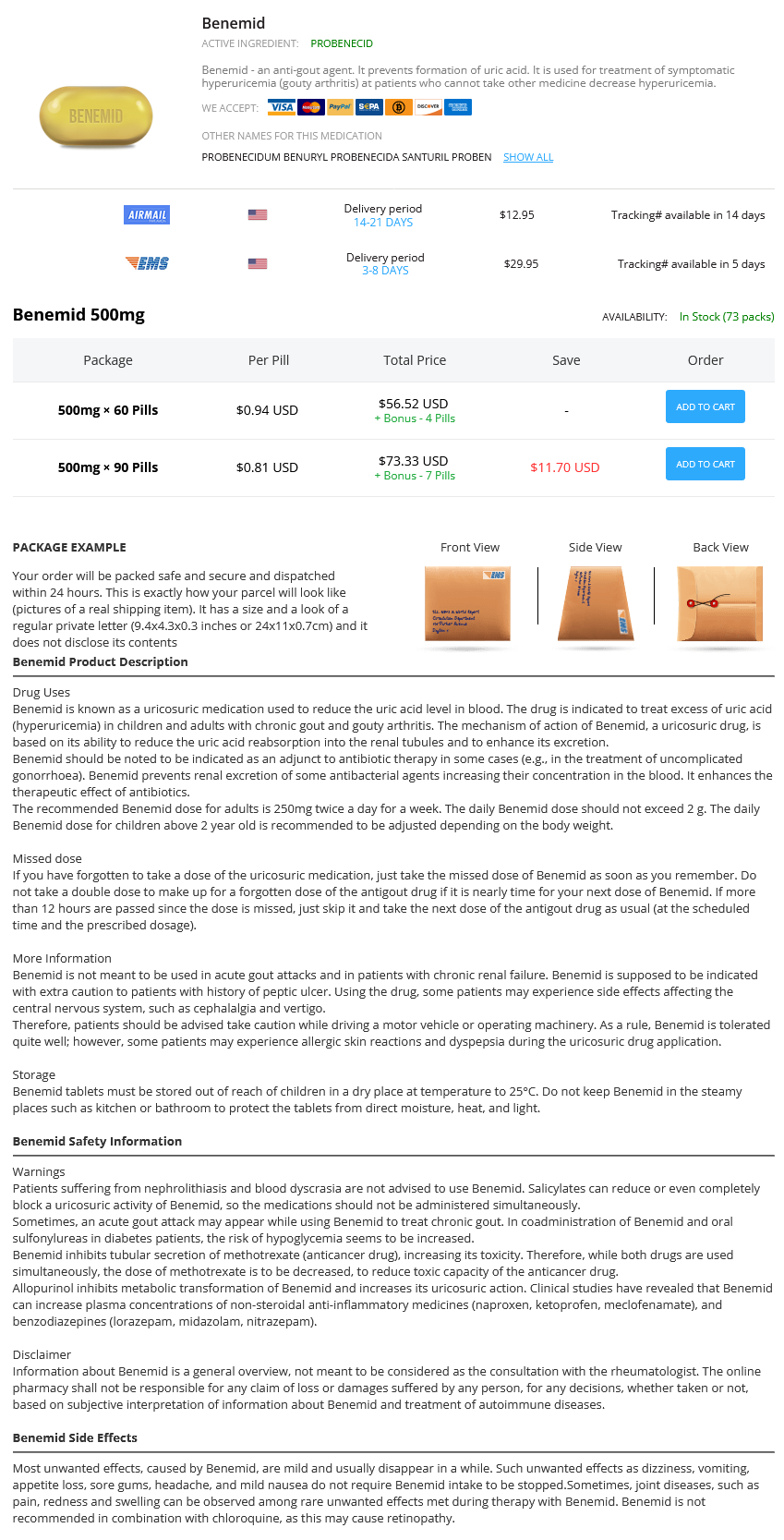
Probenecid Dosage and Price
Benemid 500mg
- 60 pills - $56.52
- 90 pills - $73.33
The bone block is inlayed into the tibial tubercle and fixed with screws or staples pain management treatment goals order probenecid on line. The soft tissue end of the graft is sutured into the patella with suture anchors and into the quadriceps with heavy nonabsorbable sutures. Reattachment of the patella tendon into its anatomic footprint on the patella is essential for re-establishing normal patellofemoral kinematics. Maximum allowed knee flexion angle without repair gap formation is determined immediately after repair. Early flexion allowances are determined intraoperatively by the quality of the tendon tissue and repair. Active-assisted range of motion is advanced as tolerated with the goal of 90 degrees of flexion by 4 to 6 weeks and full motion by 10 to 12 weeks after repair. Strengthening is initiated immediately with isometric quadriceps contractions and progressed to straight-leg raises at 6 weeks. Lindy et al8 reported excellent results in 24 patients repaired acutely and augmented with Mersilene tape placed in a looped configuration. They noted that the augmentation device allowed for early mobilization and good functional outcome. Two recent biomechanical studies show that an augmented repair is stronger than an unaugmented repair11 and that suture anchor repair is at least as strong as repair through drill holes. Residual quadriceps weakness and extensor lag are more common with repairs of chronic injuries. Reconstruction of the extensor apparatus of the knee with the Leeds-Keio ligament. Semitendinosus augmentation of acute patellar tendon repair with immediate mobilization. Ruptures usually occur transversely through the tendon at a pathologic area approximately 2 cm proximal to the superior pole of the patella, and then progress obliquely into the medial and lateral retinacula based on the amount and duration of force. Ruptures can occur at the bonetendon interface (older patients), or at the midtendinous or musculotendinous area (younger patients). Rupture can be due to trauma, use of corticosteroids, and systemic diseases (eg, gout, pseudogout, systemic lupus erythematosus, renal failure, hyperparathyroidism, diabetes mellitus). Loss of extension (straight leg raise) indicates lack of continuity of the extensor mechanism (note: ability to extend may be due to intact retinacula). Suprapatella gap (ie, soft tissue defect proximal to the superior pole of the patella) is indicated by loss of continuity of the extensor mechanism at the quadriceps tendon attachment. Patella baja (ie, patella of the injured knee more inferior than the contralateral knee) is indicated by loss of proximal extensor mechanism. Arthrography is invasive; however, it is positive with extravasation of contrast dye from the suprapatellar pouch and along the tendon sheath of the tendon. Notable findings include focal tendon discontinuity, increased signal in the tendon, wavy patella tendon, as well as possible pre-existing pathology. A bump under the ipsilateral hip can prevent external rotation of the operative leg. If an examination under anesthesia is necessary, care must be taken not to convert a partial tear to a complete rupture. For the first 6 weeks, the knee is immobilized in extension to assist with tendon healing and maintenance of tendon length. This can be done with a long-leg brace locked in extension or with a long-leg cylinder cast. In the next phase, regaining flexion is emphasized and the brace is unlocked to allow restoration of normal gait. Patients can return to activity once full range of motion and strength are restored, usually in 4 months. Any partial rupture that has progressed to a complete rupture should also be repaired as soon as diagnosed. A trough is made at the superior pole of the patella to assist with tendon reattachment. Holding the sutures provisionally, knee flexion is evaluated with patellar tracking and rotation. Patellar positioning, tracking, and tensioning of the repaired tendon are evaluated. The position of knee flexion at which tension begins on the repair should be noted, because this will determine the amount of maximum knee flexion allowed in postoperative rehabilitation. Confirmation that there is no excess tension on reapproximation for tendon repair. Placement of a continuous running stitch, beginning laterally and exiting back at the free edge of the tendon. Four sutures from the free edge of the quadriceps tendon brought inferiorly through three longitudinal drill holes in the patella. Sutures are secured with their continuous loop mate-first the lateral set, followed by the medial set. The tendon edge of necrotic and degenerative tissue is débrided down to normal-appearing healthy tendon tissue. Tendon edges are reapproximated by provisionally tensioning sutures together and evaluating knee flexion with patellar tracking and rotation. The position of knee flexion at which tension on the repair begins should be noted, because this will determine the amount of maximum knee flexion allowed in postoperative rehabilitation.