Procyclidine
General Information about Procyclidine
In conclusion, procyclidine, also called Kemadrin, is a medication used to deal with the signs of Parkinson's illness. By blocking acetylcholine, procyclidine helps to extend the levels of dopamine within the mind, thereby decreasing symptoms such as stiffness, tremors, and muscle spasms. While it could cause some unwanted facet effects, the advantages of procyclidine in improving the quality of life for individuals with Parkinson's disease cannot be overlooked. With proper use and monitoring, procyclidine may be an important device in managing this challenging condition. However, it's all the time important to seek the assistance of with a health care provider earlier than beginning any new medication.
Parkinson's illness is caused by a decrease in dopamine, a chemical messenger within the mind that's responsible for controlling movement. As dopamine levels decrease, the individual could experience issue with everyday duties such as walking, writing, and talking. This is as a end result of dopamine plays a key position in regulating the physique's motion and coordination.
One of the main advantages of procyclidine is its capability to alleviate the stiffness and tremors related to Parkinson's disease. These symptoms can greatly have an result on a person's high quality of life, making simple tasks difficult or impossible to finish. By lowering these symptoms, procyclidine may help people with Parkinson's disease to lead extra independent and fulfilling lives.
Procyclidine is out there in tablet form and is usually taken three to four times a day. The dosage could vary relying on the severity of the signs and the individual's response to the medication. It is important to follow the prescribed dosage and schedule as directed by a well being care provider to ensure the absolute best results.
Procyclidine works by blocking the consequences of acetylcholine, another chemical messenger in the brain that may worsen the symptoms of Parkinson's illness. By blocking acetylcholine, procyclidine helps to revive the stability between dopamine and acetylcholine, thereby reducing the symptoms of Parkinson's illness.
Procyclidine, additionally known by its model name Kemadrin, is a medicine primarily used to deal with the symptoms of Parkinson's illness. This condition is a neurodegenerative dysfunction that affects the central nervous system, inflicting problems with movement and coordination. Procyclidine helps to alleviate the signs of Parkinson's illness, similar to stiffness, tremors, muscle spasms, and poor muscle management.
It is essential to tell your doctor of any other drugs you're taking, as some could interact with procyclidine. This contains over-the-counter drugs, vitamins, and natural supplements. It can also be important to discuss any medical conditions you may have, as procyclidine will not be suitable for individuals with sure situations.
As with any medication, procyclidine may trigger unwanted aspect effects. These may include dry mouth, blurred imaginative and prescient, constipation, drowsiness, and urinary retention. However, these unwanted effects are usually gentle and might often be managed by adjusting the dosage or with other treatments.
In addition to its use in Parkinson's disease, procyclidine may be prescribed for different situations similar to dystonia, a movement disorder characterised by irregular muscle contractions, and drug-induced extrapyramidal symptoms, that are side effects of sure medications that have an result on motion and coordination.
This section provides an overview of major migratory pathways used by neural crest cells and introduces some of the extracellular cues that influence their migration patterns treatment room purchase 5 mg procyclidine otc. Neural crest cells emerge from the neural plate border Neural crest cells arise at the lateral edges of the neural plate-at the border that lies between the emerging neural and epidermal regions. In most vertebrates, the neural crest cells undergo a cell type transition, detaching from neuroepithelium to become loosely packed, unconnected mesenchyme cells. The individual cells reaggregate at later time points as they coalesce into new structures, such as ganglia. Several growth factors and transcription factors have been associated with inducing neural crest regions and specifying the neural crest cells as a separate cell population. These molecules also regulate additional proteins that impact further specification of neural crest regions. Transcription factors such as Pax3, Pax7, Zic1, Msx1, and Msx2 are up-regulated as the neural border is specified, thus delineating a region that is distinct from adjacent neural tube and nonneural ectoderm. Another group of transcription factors that includes Sox9, Sox10, and FoxD3 is up-regulated at the time the future neural crest region is identifiable as distinct from the other regions of the neural tube. For example, Snail2, a transcriptional repressor, represses the expression of various cadherins. During normal neural crest development, the down-regulation of these adhesion molecules is necessary for the cells to migrate. Thus, a number of transcription factors and signaling cascades must be integrated during the early stages of neural crest specification and migration to ensure the cells exit the neural crest and enter the correct migratory stream. Neural crest cells from different axial levels contribute to specific cell populations There are four primary anatomical regions from which neural crest cells arise, and cells from each of these regions migrate along limited pathways in the embryo. For example, cells of the cranial neural crest originate between the midbrain and rhombomere 6 to give rise to structures associated with the head and neck. The remaining neural crest populations originate posterior to the hindbrain and are identified based on their corresponding somite level. Somites are paired blocks of mesoderm that are numbered sequentially from anterior to posterior. The somites are often used as anatomical landmarks to designate the axial level of other structures. For example, cells of the vagal neural crest arise from the region that extends from the posterior hindbrain to somite 7. The vagal neural crest produces cells that contribute to structures in both the head and trunk, including the sensory neurons of the glossopharyngeal and vagus cranial nerves and the sympathetic, parasympathetic, and enteric ganglia of the trunk. Trunk neural crest cells give rise to the sympathetic, parasympathetic, and dorsal root ganglia, as well as the adrenal chromaffin cells. Neural crest cells that arise posterior to somite 28 give rise to parasympathetic and enteric ganglia. In addition to specific cell types associated with each region, at all levels neural crest cells contribute melanocytes, glial Schwann cells, ganglion satellite cells, and endocrine cells. Many neural crest cells have the potential to become any one of a diverse set of neural crest derivatives; dn 5. Vagal neural crest cells give rise to neurons associated with cranial and trunk ganglia, including sensory neurons of the glossopharyngeal and vagus cranial nerves and the sympathetic, parasympathetic, and enteric ganglia of the trunk. Trunk neural crest cells give rise to the dorsal root ganglia and posterior regions of the sympathetic and parasympathetic ganglia, as well as to adrenal chromaffin cells. Cranial neural crest forms structures in the head the neural crest cells at the most anterior regions give rise to head structures, including cranial ganglia, endocrine cells, pigment cells, and cranioskeletal structures. The cranial neural crest cells are unique, in that they are the only crest cells to give rise to skeletal components under normal conditions. Skeletal derivatives of the cranial neural crest include the lower jaw (mandible), bones of the face, the hyoid bone of the neck, and the three bones of the middle ear: the malleus, incus, and stapes. Because so many facial structures arise from the cranial neural crest, altered neural crest development often leads to birth defects such as cleft palate. Although neural crest cells are multipotent, some populations appear to be more restricted in their fate options. For example, cranial neural crest cells transplanted to trunk regions can form sympathetic and dorsal root ganglia as well as cells of the adrenal medulla and Schwann cells. However, neural crest cells transplanted from the trunk region to the cranial region do not readily form cartilage. As described in the following sections and in Chapter 6, neural crest cells encounter a number of extracellular cues that not only direct the migration of the cells, but also regulate these cell fate options. The cranial neural crest cells are also the source of many of the neurons that comprise the cranial ganglia. Lens epithelia cells, olfactory, auditory, and vestibular sensory cells, as well as various supporting cell types associated with these structures, arise from their corresponding placodes. For example, the statoacoustic (also called the vestibulocochlear) ganglia of the eighth cranial nerve is derived from the otic placode. Among the cranial nerve ganglia with a mix of neural crest-derived and placodederived neurons are those associated with the trigeminal, facial, glossopharyngeal, and vagus nerves. In these cranial ganglia of mixed origin, the proximal regions of these ganglia are of neural crest origin (green), while the distal portions are of placode origin (purple). Thus, some cranial ganglia consist of both neural crest and placode-derived neurons. Placodes (purple) are patches of ectoderm located in the head region of the embryo. The otic placode gives rise to the embryonic inner ear (otocyst) as well as the associated statoacoustic (vestibulocochlear) ganglia of the eighth cranial nerve. Cranial crest cells migrate in lateral and ventral directions to form structures in the head and neck, while trunk crest cells migrate through or around somites to form melanocytes, peripheral ganglia, and related cells.
Conversely medications lexapro cheap procyclidine 5 mg buy online, if arterial pressure suddenly decreases, there is less stretch on the arterioles, causing them to relax and arteriolar resistance to decrease. Thus constant flow can be maintained in the face of increased or decreased arterial pressure by changing arteriolar resistance. One can also think about the myogenic mechanism in terms of maintaining arteriolar wall tension. Blood vessels, such as arterioles, are built to withstand the wall tensions they normally "see. Thus in response to the stretch, arteriolar vascular smooth muscle contracts, decreasing the arteriolar radius and returning wall tension back to normal. This relationship is explained by the law of Laplace for a cylinder, which states that T = P × r. If pressure (P) increases and radius (r) decreases, then wall tension (T) can remain constant. The metabolic hypothesis can be invoked to explain each of the phenomena of local control of blood flow. The basic premise of this hypothesis is that O2 delivery to a tissue can be matched to O2 consumption of the tissue by altering the resistance of the arterioles, which in turn alters blood flow. As a result of metabolic activity, the tissues produce various vasodilator metabolites. The greater the level of metabolic activity, the greater the production of vasodilator metabolites. These metabolites produce vasodilation of arterioles, which decreases resistance and therefore increases flow to meet the increased demand for O2. The following two examples illustrate how the metabolic hypothesis explains active hyperemia: (1) the first example considers strenuous exercise. During strenuous exercise, metabolic activity in the exercising skeletal muscle increases and production of vasodilator metabolites, such as lactate, increases. Initially, the increased pressure will increase blood flow, which will deliver more O2 for metabolic activity and "wash out" vasodilator metabolites. As a result of this washout, there will be a local dilution of vasodilator metabolites, resulting in arteriolar vasoconstriction, increased resistance, and a compensatory decrease in blood flow back to the normal level. Neural and Hormonal Control of Blood Flow the most important example of neural (extrinsic) control of regional blood flow involves the sympathetic innervation of vascular smooth muscle in some tissues. For example, blood vessels of the skin and skeletal muscle have a high density of sympathetic nerve fibers, whereas coronary, pulmonary, and cerebral vessels have little sympathetic innervation. It is important to note whether sympathetic innervation is absent or present and also, when present, whether it produces vasoconstriction or vasodilation (see Table 2. In skeletal muscle, when the sympathetic nervous system is activated, there can be vasoconstriction (sympathetic nerve fibers, 1 receptors) or vasodilation (epinephrine from adrenal medulla, 2 receptors). Other vasoactive substances include histamine, bradykinin, serotonin, and prostaglandins. Simultaneously, it causes dilation of arterioles and constriction of venules, with the net effect being a large increase in Pc, which increases filtration out of capillaries, and local edema. Bradykinin, like histamine, causes dilation of arterioles and constriction of venules, resulting in increased filtration out of capillaries and local edema. Serotonin is released in response to blood vessel damage and causes local vasoconstriction (in an attempt to reduce blood flow and blood loss). Serotonin has been implicated in the pathophysiology of vascular spasms that occur in migraine headache. Prostacyclin and the prostaglandin-E series are vasodilators in many vascular beds. Coronary Circulation Blood flow through the coronary circulation is controlled almost entirely by local metabolites, with sympathetic innervation playing only a minor role. For example, if there is an increase in myocardial contractility, there is increased O2 demand by the cardiac muscle and increased O2 consumption, causing local hypoxia. This local hypoxia causes vasodilation of the coronary arterioles, which then produces a compensatory increase in coronary blood flow and O2 delivery to meet the demands of the cardiac muscle. An unusual feature of the coronary circulation is the effect of mechanical compression of the blood vessels during systole in the cardiac cycle. Cerebral Circulation the cerebral circulation is controlled almost entirely by local metabolites and exhibits autoregulation and active and reactive hyperemia. It is interesting that many circulating vasoactive substances do not affect the cerebral circulation because their large molecular size prevents them from crossing the blood-brain barrier. Pulmonary Circulation the regulation of pulmonary circulation is discussed fully in Chapter 5. The effect of O2 on pulmonary arteriolar resistance is the exact opposite of its effect in other vascular beds: In the pulmonary circulation, hypoxia causes vasoconstriction. Briefly, regions of hypoxia in the lung cause local vasoconstriction, which effectively shunts blood away from poorly ventilated areas where the blood flow would be "wasted" and toward well-ventilated areas where gas exchange can occur. Renal Circulation the regulation of renal blood flow is discussed in detail in Chapter 6. Briefly, renal blood flow is tightly autoregulated so that flow remains constant even when renal perfusion pressure changes. Renal autoregulation is independent of sympathetic innervation, and it is retained even when the kidney is denervated. Autoregulation is presumed to result from a combination of the myogenic properties of the renal arterioles and tubuloglomerular feedback (see Chapter 6). Skeletal Muscle Circulation Blood flow to skeletal muscle is controlled both by local metabolites and by sympathetic innervation of its vascular smooth muscle. At rest, blood flow to skeletal muscle is regulated primarily by its sympathetic innervation. Vascular smooth muscle in the arterioles of skeletal muscle is densely innervated by sympathetic nerve fibers that are vasoconstricting (1 receptors).
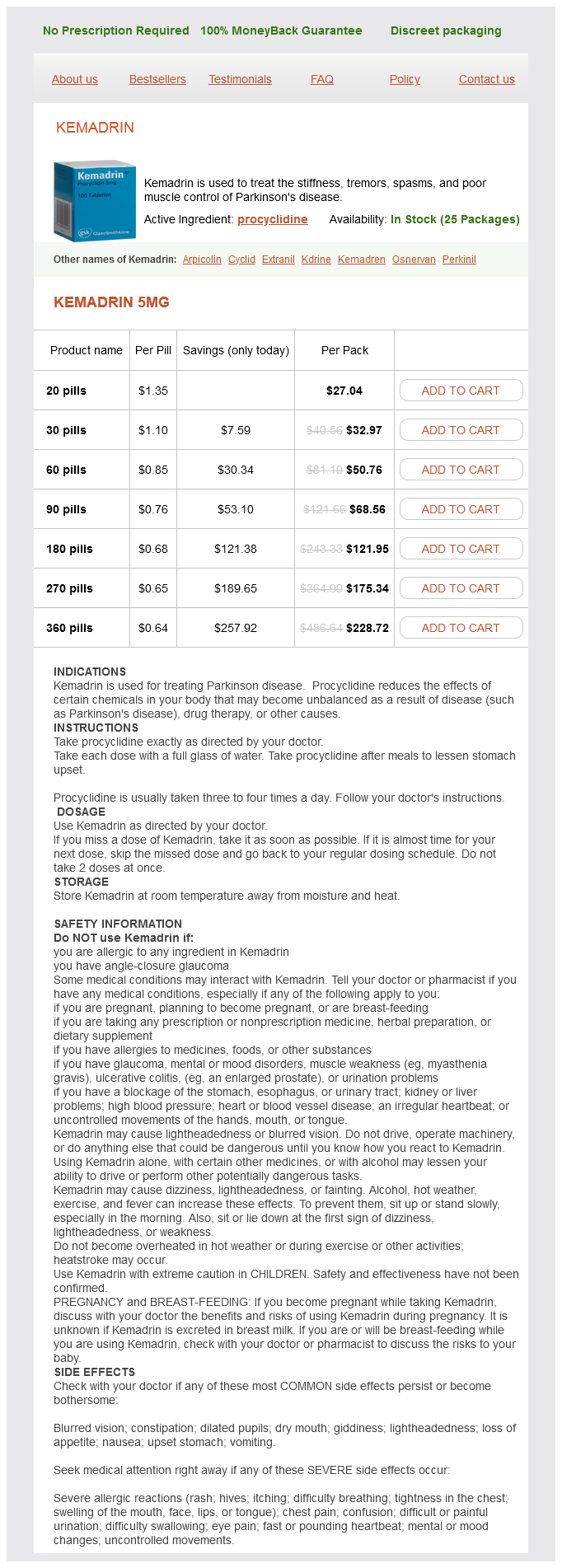
Procyclidine Dosage and Price
Kemadrin 5mg
- 20 pills - $27.04
- 30 pills - $32.97
- 60 pills - $50.76
- 90 pills - $68.56
- 180 pills - $121.95
- 270 pills - $175.34
- 360 pills - $228.72
Axons carry action potentials between the neuron cell body and the targets of that neuron symptoms gastritis procyclidine 5 mg buy fast delivery, either other neurons or muscle. Axons may be insulated with myelin (see Chapter 1), which increases conduction velocity; breaks in the myelin sheath occur at the nodes of Ranvier. When the action potential transmitted down the axon reaches the presynaptic terminal, neurotransmitter is released into the synapse. The transmitter diffuses across the synaptic cleft and binds to receptors on the postsynaptic membrane. In this way, information is transmitted rapidly from neuron to neuron (or, in the case of the neuromuscular junction, from neuron to skeletal muscle). Some glial cells of the adult brain have the properties of stem cells and thus can give rise to new glial cells or even new neurons. Microglial cells proliferate following neuronal injury and serve as scavengers to remove cellular debris. Although the details of each system will vary, these features can be appreciated as a set of recurring themes throughout neurophysiology. Synaptic Relays the simplest synapses are one-to-one connections consisting of a presynaptic element. In the nervous system, however, many synapses are more complicated and use synapses in relay nuclei to integrate converging information. Relay nuclei contain several different types of neurons including local interneurons and projection neurons. The projection neurons extend long axons out of the nuclei to synapse in other relay nuclei or in the cerebral cortex. Almost all information going to and coming from the cerebral cortex is processed in thalamic relay nuclei. For example, in the somatosensory system, a somato topic map is formed by an array of neurons that receive information from and send information to specific locations on the body. The topographic coding is preserved at each level of the nervous system, even as high as the cerebral cortex. In the visual system, the topographic representation is called retinotopic, in the auditory system it is called tonotopic, and so forth. Decussations Almost all sensory and motor pathways are bilaterally symmetric, and information crosses from one side (ipsilateral) to the other (contralateral) side of the brain or spinal cord. Thus sensory activity on one side of the body is relayed to the contralateral cerebral hemisphere; likewise, motor activity on one side of the body is controlled by the contralateral cerebral hemisphere. For example, in the visual system, half of the axons from each retina cross to the contralateral side and half remain ipsilateral. Types of Nerve Fibers Nerve fibers are classified according to their conduction velocity, which depends on the size of the fibers and the presence or absence of myelination. The effects of fiber diameter and myelination on conduction velocity are explained in Chapter 1. Conduction velocity also is increased by the presence of a myelin sheath around the nerve fiber. Thus large myelinated nerve fibers have the fastest conduction velocities, and small unmyelinated nerve fibers have the slowest conduction velocities. Two classification systems, which are based on differences in conduction velocity, are used. The first system, described by Erlanger and Gasser, applies to both sensory (afferent) and motor (efferent) nerve fibers and uses a lettered nomenclature of A, B, and C. In the visual, taste, and auditory systems, the receptors are specialized epithelial cells. In the somatosensory and olfactory systems, the receptors are first-order, or primary afferent, neurons. Regardless of these differences, the basic function of the receptors is the same: to convert a stimulus. The conversion process, called sensory transduction, is mediated through opening or closing specific ion channels. Opening or closing ion channels leads to a change in membrane potential, either depolarization or hyperpolarization, of the sensory receptor. Such a change in membrane potential of the sensory receptor is called the recep tor potential. Information is transmitted, via a series of neurons, from receptors in the periphery to the cerebral cortex. Synapses are made in relay nuclei between first- and second-order neurons, between second- and third-order neurons, and between third- and fourth-order neurons. Second-order neurons cross the midline either in the spinal cord (shown) or in the brain stem (not shown) so that information from one side of the body is transmitted to the contralateral thalamus and cerebral cortex. The firstorder neuron is the primary sensory afferent neuron; in some cases (somatosensory, olfaction), it also is the receptor cell. When the sensory receptor is a specialized epithelial cell, it synapses on a first-order neuron. When the receptor is also the primary afferent neuron, there is no need for this synapse. The primary afferent neuron usually has its cell body in a dorsal root or spinal cord ganglion.