Proventil
General Information about Proventil
In conclusion, Proventil is an effective and safe treatment for the treatment and prevention of bronchospasm in people with reversible obstructive airway disease. Its fast-acting nature and minimal side effects make it a well-liked choice amongst patients and healthcare suppliers. However, it is crucial to make use of this medicine as prescribed and seek medical advice if any concerns come up. With correct use and monitoring, Proventil can present aid and improve the standard of life for people with bronchospasm.
Individuals with a historical past of coronary heart problems, hypertension, diabetes, and thyroid problems should seek the assistance of their healthcare provider earlier than using Proventil. It is also important to inform your physician of another drugs or supplements you're at present taking to avoid potential drug interactions.
Bronchospasm is a condition where the muscles across the airways tighten, causing the airways to turn into narrower and making it troublesome to breathe. This can be attributable to varied components similar to allergic reactions, asthma, and persistent obstructive pulmonary disease (COPD). Proventil supplies reduction by relaxing these muscular tissues, allowing the airways to open up and enhance breathing.
Proventil can also be used as a preventative measure for people who experience exercise-induced bronchospasm (EIB). This situation is widespread among athletes and individuals who engage in bodily actions. By utilizing Proventil before exercising, it could help forestall bronchospasm and enhance total performance. It is essential to follow the beneficial dosage and directions when using Proventil for EIB to avoid any potential side effects.
Proventil is a popular medicine used to treat or stop bronchospasm in people who have reversible obstructive airway disease. This medicine is a quick-relief inhaler that works by opening up the air passages in the lungs, making it simpler to breathe.
One of the most important benefits of Proventil is its fast onset of motion. It starts working within minutes after using it and supplies relief from bronchospasm for up to four to 6 hours. This makes it an excellent medicine for people who experience sudden flare-ups of respiration difficulties.
One of the numerous advantages of Proventil is its safety profile. It is mostly well-tolerated and has a decrease incidence of side effects when in comparability with different medications used to deal with bronchospasm. However, as with every treatment, some mild unwanted effects could happen in some people, together with trembling, nervousness, headache, and elevated heart rate. These side effects are normally momentary and will subside after a few doses. However, if they persist or become worse, it is essential to consult a healthcare professional.
Proventil is a brand name for the generic drug albuterol. It falls beneath the class of medicines generally known as short-acting beta-agonists (SABAs). It is available in the type of an inhaler, which delivers the medicine on to the lungs for faster reduction.
Proventil should not be used as a long-term remedy for persistent circumstances such as asthma and COPD. It is primarily meant to supply quick reduction throughout sudden episodes of bronchospasm. For long-term administration of those conditions, your doctor could recommend different medicines.
A clinician judging the impact of an operation may want to know that a woman has a noncoital pain disorder such as vulvodynia only to be able to counsel that she is unlikely to be cured of this complaint by her prolapse surgery asthma definition 8 parts purchase proventil 100 mcg visa. The words used in the items need to be appropriate to ask or identify the same aspect of behavior that the clinician is interested in. The shared understanding may need to be tested in focus groups, particularly with respect to sex where both clinicians and patients use surrogate phrases. An example may be the use of the word libido that for many lay people means all aspects of sexual function-desire, arousal, and erection. Simpler, shorter questions with depersonalized answers to sensitive issues are more likely to produce answers that patients are willing to divulge. Further validation is recommended in distinct cultural groups since sex/sexual relationship is especially culturally determined. Generic the Derogatis inventory of sexual functioning [37] and the Golombok Rust inventory of sexual satisfaction [38] are earlier measures designed to capture the essence of sexual behavior and sexual dysfunction in both men and women. It covers a wide range of concepts and assesses the two main sexual dysfunctions-desire and arousal-but validation of the measure is questionable. A follow-up study by Mazer has produced a new scoring algorithm but needs further validation. The female version comprises 35 items, forming five domains: sexual desire/frequency, sexual desire/interest, sexual pleasure, sexual arousal, and sexual orgasm. A short form (14 items) was developed and validated to allow easier use in clinical practice [44]. The measure was subsequently validated in a group of sexually active women, women with a sexual 220 dysfunction, and women attending a psychiatric clinic [52]. However, the number of subjects was small, n = 115, n = 17, and n = 16, respectively, and particularly draws into question the robustness of the cutoff score to indicate sexual dysfunction. Additionally, the interviews were conducted across seven countries (the United Kingdom, the United States, Australia, the Netherlands, Denmark, France, Italy) to determine whether cultural background affected the way women described their sexual health/function; consistency of reporting was found. The confirmation of the pain cutoff scores is required because there were few women with sexual pain used in the assessment. The profile of female sexual dysfunction was developed through patient interviews and focus groups with women from Europe and North America and who were either naturally or surgically postmenopausal and had low desire [56]. Item analysis resulted in seven domains (sexual desire, arousal, orgasm, sexual pleasure, sexual concerns, sexual responsiveness, and sexual self-image) across 37 items. The 12-item measure was developed from 10 interviews with women, which led to domains of receptivity, arousal, lubrication, sexual pleasure, sexual satisfaction, and orgasm. The validation was conducted in pre- and postmenopausal women who were dissatisfied with their sexual function. Reliability of the orgasm and receptivity domains were not ideal and should be explored further. General questionnaires will analyze function in general populations but may not be sensitive enough to detect subtle changes. Confounders such as age and menopausal status need to be accounted for and could alter the suitability of a particular instrument. Many studies using non-disease-specific tools have shown no change, which may be in part due to their lack of sensitivity or could really suggest limited change with surgery. Normative scores with general population testing established a mean score of 94, maximum being 124. The authors suggest one problem replaces another-altered vaginal anatomy before surgery to dyspareunia postsurgery. This has led to the use of the Sexual Distress Scale that measures distress due to the inhibition of sexual function and can be used to measure impact of the disease process on sexuality and benefit of intervention over time, without a need for engagement in sexual activity of any kind [64]. This may be particularly important for women with pain syndromes such as chronic bladder pain syndrome that disproportionately affects younger women and their sex lives. Overall, the use of nonvalidated and generic questionnaires makes urogynecological studies of sexual function difficult to compare and the results, if contradictory, are inconclusive. Therefore, when determining the right tool to be used, the outcomes of value should be carefully considered to ensure that these are adequately captured. For instance, if the measure is to be used in clinical practice to monitor patient outcome, then a short instrument would be more realistic to mitigate the time burden for both clinician and patient. The use of a disease-specific tool validated in the appropriate population with a representative recall period 222. Regardless of setting, when choosing a measure, ensuring appropriate information of interest is obtained is essential. Then, an assessment of the measures validity and reliability in the population of interest to the clinician should be evident. The distress caused by these difficulties and its alleviation by urogynecological interventions are the information sought by clinicians and that should guide the management of patients. In the area of sexual function, the only reproducible and consistent method of reporting these outcomes is with welldesigned, validated questionnaires. Practice patterns of physician members of the American urogynecologic society regarding female sexual dysfunction: Results of a national survey. Problems with sexual function in people attending London general practitioners: Cross sectional study. Secular trends in self reported sexual activity and satisfaction in Swedish 70 year olds: Cross sectional survey of four populations, 19712001. Report of the international consensus development conference on female sexual dysfunction: Definitions and classifications.
Translation and validation of the Japanese version of the fecal incontinence quality of life scale asthma treatment 1930s cheap 100 mcg proventil. Bowel disturbances are the most important risk factors for late onset fecal incontinence: A population-based case-control study in women. Biofeedback therapy plus anal electrostimulation for fecal incontinence: Prognostic factors and effects on anorectal physiology. The role of an intra-anal tampon for faecal incontinence: Preliminary results of a prospective study. Management of obstetric anal sphincter injury: A systematic review & national practice survey. A randomized clinical trial comparing primary overlap with approximation repair of third-degree obstetric tears. Long-term outcome of delayed primary or early secondary reconstruction of the anal sphincter after obstetrical injury. Early results of immediate repair of obstetric third-degree tears: 65% are completely asymptomatic despite persistent sphincter defects in 61%. Long-term results of total pelvic floor repair for postobstetric fecal incontinence. Electrical stimulation of sacral spinal nerves for treatment of faecal incontinence. Alterations of cortical electrical activity in patients with sacral neuromodulator. Sacral nerve stimulation and rectal function: Results of a prospective study in faecal incontinence. Short-term sacral nerve stimulation for functional anorectal and urinary disturbances: Results in 40 patients: Evaluation of a new option for anorectal functional disorders. Determination of therapeutic threshold in sacral nerve modulation for faecal incontinence. Sacral nerve stimulation for fecal incontinence: External anal sphincter defect vs. Effects of short term sacral nerve stimulation on anal and rectal function in patients with anal incontinence. Neuromodulation for fecal incontinence: Outcome in 16 patients with definitive implant. Sacral nerve modulation and other treatments in patients with faecal incontinence after unsuccessful pelvic floor rehabilitation: A prospective study. Sacral nerve stimulation is more effective than optimal medical therapy for severe fecal incontinence: A randomized, controlled study. Meta-analysis: Sacral nerve stimulation versus conservative therapy in the treatment of faecal incontinence. Sacral nerve stimulation for faecal incontinence: Results from a single centre over a 10-year period. Evaluation of the use of posterior tibial nerve stimulation for the treatment of fecal incontinence: Preliminary results of a prospective study. Percutaneous tibial nerve stimulation for the treatment of urge fecal incontinence. Peripheral neuromodulation via posterior tibial nerve stimulation-A potential treatment for faecal incontinence Clinical, physiological, and radiological study of a new purpose-designed artificial bowel sphincter. The Secca procedure for the treatment of fecal incontinence: Definitive therapy or short-term solution. Temperature-controlled radio frequency energy delivery (Secca procedure) for the treatment of fecal incontinence: Results of a prospective study. Radiofrequency energy delivery to the anal canal: Is it a promising new approach to the treatment of fecal incontinence Does the radiofrequency procedure for fecal incontinence improve quality of life and incontinence at 1-year follow-up Polytetrafluoroethylene injection for the treatment of partial fecal incontinence. Systematic review on the efficacy and safety of injectable bulking agents for passive fecal incontinence. Its incidence increases with age and is higher in those of lower socioeconomic class and with lower educational status [2]. These include dietary factors, toileting habits, medications, underlying medical conditions, psychological problems, organic diseases of the gastrointestinal tract (Table 63. The primary function of the colon is the absorption of water from the small bowel effluent, leaving 100150 mL of water in feces. A secondary function is to enable bacteria to ferment undigested fiber; the rectum stores feces until defecation takes place. The colon, rectum, and internal anal sphincter (continuation of the smooth muscle) are extrinsically innervated by the autonomic nervous system. The sympathetic innervation via the coeliac, superior, and inferior mesenteric plexus and hypogastric nerves (T11L2) inhibits peristalsis and are sensitive to distension. The parasympathetic innervation by preganglionic vagal fibers and S24 splanchnic nerves increases peristalsis, contracts rectum, and relaxes internal anal sphincter to assist defecation. The intrinsic enteric nervous system (submucosal and myenteric plexuses) influences contractions and tone while the cells of Cajal are pacemakers. In order to be considered of medical significance, symptoms must be present for at least 3 months with onset of symptoms 6 months before diagnosis [5]. Subtypes of Constipation Constipation can be divided into the following subtypes: 1. Motility disorder: Decreased high-amplitude peristaltic contraction causing slow transit constipation.
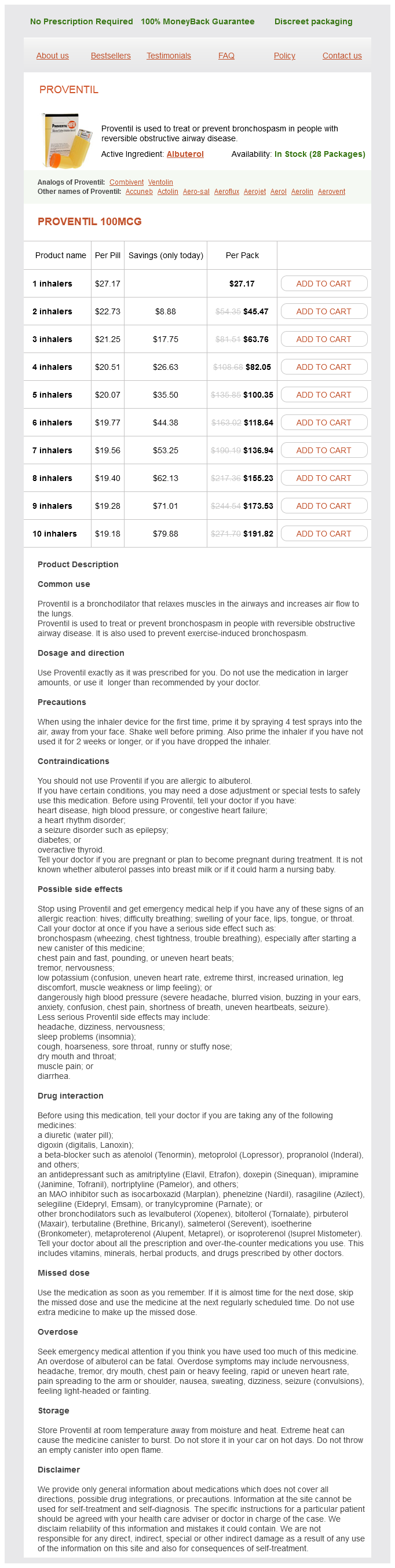
Proventil Dosage and Price
Proventil 100mcg
- 1 inhalers - $27.17
- 2 inhalers - $45.47
- 3 inhalers - $63.76
- 4 inhalers - $82.05
- 5 inhalers - $100.35
- 6 inhalers - $118.64
- 7 inhalers - $136.94
- 8 inhalers - $155.23
- 9 inhalers - $173.53
- 10 inhalers - $191.82
Autoradiographic localization of 5hydroxytryptamine1A asthma in kids 100 mcg proventil order with amex, 5-hydroxytryptamine1B and 5-hydroxytryptamine1C/2 binding sites in the rat spinal cord. Evidence for involvement of the subcoeruleus nucleus and nucleus raphe magnus in urine storage and penile erection in decerebrate rats. An unexpected association between urinary incontinence, depression and sexual dysfunction. Effects of gamma-aminobutyrate B receptor modulation on normal micturition and oxyhemoglobin induced detrusor overactivity in female rats. Gabapentin: A novel drug as add-on therapy in cases of refractory overactive bladder in children. Micturition in conscious rats with and without bladder outlet obstruction- 371 Role of spinal alpha(1)-adrenoceptors. Spinal and peripheral mechanisms contributing to hyperactive voiding in spontaneously hypertensive rats. Role of intrathecal tachykinins for micturition in unanaesthetized rats with and without bladder outlet obstruction. Effects of neurokinin receptor antagonists on L-dopa induced bladder hyperactivity in normal conscious rats. Role of supraspinal tachykinins for volume- and L-dopa-induced bladder activity in normal conscious rats. Efficacy and safety of repeated dosing of netupitant, a neurokinin-1 receptor antagonist, in treating overactive bladder. Bladder dysfunction and parkinsonism: Current pathophysiological understanding and management strategies. On the localization and mediation of the centrally induced hyperactive urinary bladder response to L-dopa in the rat. Dopamine receptor subtypes that induce hyperactive urinary bladder response in anesthetized rats. Brusa L, Petta F, Pisani A, Miano R, Stanzione P, Moschella V, Galati S, Finazzi Agrò E. Brusa L, Petta F, Pisani A, Moschella V, Iani C, Stanzione P, Miano R, Finazzi-Agrò E. Acute vs chronic effects of ldopa on bladder function in patients with mild Parkinson disease. Muscarinic receptors of the urinary bladder: Detrusor, urothelial and prejunctional. Signal transduction underlying carbachol-induced contraction of human urinary bladder. Expression and functional role of Rho-kinase in rat urinary bladder smooth muscle. Functional role of M-2 and M-3 muscarinic receptors in the urinary bladder of rats in vitro and in vivo. Muscarinic M2 receptors inhibit Ca2+-activated K+ channels in rat bladder smooth muscle. M2 muscarinic receptor contributes to contraction of the denervated rat urinary bladder. Interaction between muscarinic receptor subtype signal transduction pathways mediating bladder contraction. The M2 muscarinic receptor mediates in vitro bladder contractions from patients with neurogenic bladder dysfunction. Prejunctional muscarinic inhibitory control of acetylcholine release in the human isolated detrusor: Involvement of the M4 receptor subtype. Function, signal transduction mechanisms and plasticity of presynaptic muscarinic receptors in the urinary bladder. Change in muscarinic modulation of transmitter release in the rat urinary bladder after spinal cord injury. Urothelium-derived inhibitory factor(s) influences on detrusor muscle contractility in vitro. Qualitative and quantitative expression profile of muscarinic receptors in human urothelium and detrusor. Substance P-containing axon terminals in the mucosa of the human urinary bladder: Pre-embedding immunohistochemistry using cryostat sections for electron microscopy. Co-existence of nitrergic, peptidergic and acetylcholine esterase-positive nerves in the pig lower urinary tract. Alpha1-, alpha2- and beta-adrenoceptors in the urinary bladder, urethra and prostate. Increased contractile response to phenylephrine in detrusor of patients with bladder outlet obstruction: Effect of the alpha1A and alpha1D-adrenergic receptor antagonist tamsulosin. Effect of doxazosin on rat urinary bladder function after partial outlet obstruction. The forefront for novel therapeutic agents based on the pathophysiology of lower urinary tract dysfunction: Alpha-blockers in the treatment of male voiding dysfunction-How do they work and why do they differ in tolerability Tolterodine and tamsulosin for treatment of men with lower urinary tract symptoms and overactive bladder: A randomized controlled trial. A randomized double-blind placebocontrolled multicentre study to explore the efficacy and safety of tamsulosin and tolterodine in women with overactive bladder syndrome. The effect of terazosin on functional bladder outlet obstruction in women: A pilot study.