Ramipril
General Information about Ramipril
Altace ought to be taken regularly for it to be efficient in controlling blood stress. If a dose is missed, you will want to take it as soon as remembered. However, whether it is virtually time for the next scheduled dose, do not take an additional dose to make up for the missed one.
Before starting ramipril, it is very important inform your doctor of any pre-existing situations or drugs you might be taking. It is especially essential to discuss any historical past of liver or kidney disease, diabetes, coronary heart illness, or any allergy symptoms. This will help the doctor determine if ramipril is a safe and suitable medication for you.
Ramipril is available in pill type and is usually taken as soon as a day, with or without meals. The dosage will depend upon the individual's blood stress levels and response to the treatment, and it may be adjusted by a health care provider over time.
High blood stress, if left untreated, can result in critical health consequences corresponding to heart illness, stroke, and kidney failure. Therefore, it is necessary to control it with the assistance of medicines like ramipril.
In conclusion, ramipril, bought as Altace, is a generally prescribed medicine for treating hypertension, but it additionally has additional benefits in decreasing the chance of heart disease. It is necessary to comply with the really helpful dosage and seek the advice of together with your physician to ensure its effectiveness and to manage any potential unwanted side effects. By working along with way of life changes, ramipril may be an efficient tool in controlling blood pressure and minimizing the chance of significant health issues.
Ramipril, bought underneath the brand name Altace, is a drugs used to deal with hypertension (hypertension). It belongs to a class of medicine generally recognized as ACE inhibitors, and works by enjoyable blood vessels and improving blood circulate, which helps to lower blood stress.
It is also necessary to monitor your blood pressure frequently whereas taking ramipril, as it could take a couple of weeks for the medication to reach its full effect. It just isn't uncommon for medical doctors to also recommend life-style modifications alongside treatment to manage hypertension, such as common train, a healthy diet, and limiting alcohol and salt consumption.
Some widespread side effects which will happen whereas taking ramipril embrace dizziness, tiredness, cough, and headache. These side effects are usually mild and may subside because the physique adjusts to the treatment. However, if they persist or turn out to be bothersome, it may be very important seek the guidance of a doctor. Rare but extra critical unwanted facet effects could embrace difficulty breathing, swelling of the face, lips, tongue, or throat, and chest pain. If any of these happen, search medical attention instantly.
Unlike other medicines for hypertension, ramipril not solely helps to decrease blood stress, nevertheless it also has additional benefits. It has been shown to decrease the risk of heart assault, stroke, and dying in patients with a history of heart disease or these at excessive risk for it. This makes ramipril a useful and commonly prescribed treatment for treating hypertension.
Ramipril can work together with other medications, including over-the-counter medication and herbal dietary supplements. It is necessary to tell your physician of all of the medications you take to keep away from any potential issues.
Because prevention is the cornerstone of maintaining musculoskeletal health prehypertension heart attack order ramipril no prescription, the care provided by hemophilia specialists is important to prevent and adequately treat bleeds and provide early recognition of musculoskeletal issues. Physiotherapy is required for recovery after musculoskeletal bleeds and to maintain muscle strength in individuals with established hemophilic arthropathy. A physiatrist can help provide patient education to prevent disabling injuries, care during bleeding episodes, long-term rehabilitation, and orthotics and shoe adaptations. The efficacy of joint aspiration along with adequate factor replacement is unclear. Theoretically, shortening the exposure of cartilage to blood might limit blood-induced damage. The most recent in vitro experimental data suggest that limitation of blood exposure to cartilage may prevent tissue damage later. Clearly, if the suspicion of infection is high, arthrocentesis is mandatory for diagnosis, but in general it should be avoided. According to the World Federation of Hemophilia guidelines, arthrocentesis may be considered in a bleeding, tense, and painful joint that shows no improvement 24 hours after conservative treatment and after exclusion of inhibitor development. In recurrent or massive bleeds that are unresponsive to appropriate clotting factor replacement, therapeutic embolization could be considered. Immobilization and avoiding or minimizing weight bearing on the affected joint is important during active bleeding and might be helpful in protecting against cartilage damage. Performing orthopedic surgery in hemophilic patients requires a large supply of clotting factor and intensive rehabilitation. With use of conservative procedures, remarkable benefit can be achieved and surgical interventions can be postponed. For pain relief, adequate analgesic treatment, manual traction of the joint, and in some cases transcutaneous electrical nerve stimulation are indicated. In patients with involvement of more than one joint, hydrotherapy enables functional training with minimal weight bearing. Orthotics and shoe adaptations provide immobilization, support, stability, compensation for deformities, and reduced weight bearing. Different surgical options could be considered depending on the joint or specific condition requiring correction. Joint replacement therapy of the knee and hip and less commonly of the elbow and shoulder and ankle arthrodesis are the most performed procedures. Joint replacement therapy is very successful in relieving pain and increasing functional activities and participation. Drawbacks of arthrodesis are the loss of mobility of the joint and the possibility of overloading other joints of the lower limb/foot, necessitating surgical repair of other joints. Higher rates of aseptic loosening and deep infections due to poor bone quality and increased risk of micro-bleeds at the prosthesis-bone interface are concerns. Other procedures performed in end-stage arthropathy or in case of severe contractures include soft tissue contracture release, arthroscopic débridement for intra-articular adhesions and impingement, tendon reconstruction, osteotomy to correct angular deformity, and radial head excision combined with synovectomy if enlargement and erosion of the radial head cause mechanical blockage of forearm rotation. Major orthopedic procedures can be performed safely and successfully, even in patients with inhibitors. This goal might be achieved by (more intensive) prophylactic clotting factor concentrate replacement for 6 to 8 weeks combined with active physiotherapy and cooling. If conservative measures fail and chronic synovitis persists with frequent recurrent bleeding, synovectomy might be indicated either surgically, arthroscopically, or through intra-articular injection of radiopharmaceutical agents or chemicals. Radioisotopic synovectomy using a pure beta emitter (yttrium-90 or phosphorus-32) is preferred because it is minimally invasive and requires little factor replacement and less intense rehabilitation afterward. This procedure is very successful in reducing hemarthroses; 60% to 100% are reduced in the majority of patients. However, potential direct harmful effects to cartilage in the long term should be taken into consideration. In patients who have arthropathy of more than one joint of the lower extremities, multiple procedures could be combined during one in-hospital stay, either in a single session or staged. Careful assessment by a multidisciplinary team is a prerequisite to ensure that recovery will not be compromised for any of the procedures. Patients with severe hemophilia who receive intermediate dose prophylaxis still experience 0. Diagnostic strategies are needed to detect early changes within a joint and to evaluate joint damage progression regularly; biochemical markers of joint tissue damage are very promising in this respect. Gene therapy to "cure" hemophilia faces many challenges regarding efficacy and safety. Specific therapies opposing inflammatory cytokines117,118 or reducing synovial iron deposition119 to limit synovitis and cartilage damage and procedures aiming at cartilage restoration112,120 in overt joint damage may become plausible new approaches, although introduction of these therapeutic strategies into clinical practice remains challenging. In the meantime, emphasis should be placed on preventing hemarthrosis by clotting factor replacement, education, adequate pain relief, physical therapy, and maintaining physical activity to reduce development of end-stage arthropathy. Shaerf D, Banerjee A: Assessment and management of posttraumatic haemarthrosis of the knee. Fischer K, Collins P, Bjorkman S, et al: Trends in bleeding patterns during prophylaxis for severe haemophilia: observations from a series of prospective clinical trials. Brinkmann T, Kahnert H, Prohaska W, et al: Synthesis of tissue factor pathway inhibitor in human synovial cells and chondrocytes makes joints the predilected site of bleeding in haemophiliacs. Nieuwenhuizen L, Roosendaal G, Coeleveld K, et al: Haemarthrosis stimulates the synovial fibrinolytic system in haemophilic mice. Balkan C, Kavakli K, Karapinar D: Iliopsoas haemorrhage in patients with haemophilia: results from one centre. Iorio A, Fabbriciani G, Marcucci M, et al: Bone mineral density in haemophilia patients. Barnes C, Wong P, Egan B, et al: Reduced bone density among children with severe hemophilia. Beeton K, de Kleijn P, Hilliard P, et al: Recent developments in clinimetric instruments.
This level of data compatibility from different phases of care is especially important to determine the effects of certain interventions on long-term outcome blood pressure normal ki dua ramipril 5 mg order with amex. Constant system evaluation is necessary to identify where the system falls short operationally and stimulate strategies for improvements in system design. Because each of these, and many subcomponents thereof may fall within the purview of different stakeholder groups, and may require special data security arrangements, this process should be defined as part of the regional trauma system plan. The American College of Surgeons Committee on Trauma has developed multiple programs and quality assessment processes that can guide this program as well as provide objective external review. The most common scientific approaches include panel review of preventable death studies, trauma registry performance comparisons, and population-based studies. Panel review studies are conducted by experts who review trauma-related deaths to determine preventability. Well-defined criteria and standardized definitions regarding preventability have been used, but significant methodological problems can lead to inconsistencies in the results and interpretation of the data. According to Mann et al, review of the published literature in preparation for the Skamania Symposium supported the conclusion that the implementation of trauma systems decreases hospital mortality of severely injured patients. Mortality decreased as seen in other regions, and inpatient preventable mortality decreased significantly. The participants of the Skamania symposium also emphasized that not only mortality but also functional outcomes, financial outcomes, patient satisfaction, and cost-effectiveness should be evaluated in future prospective, well-controlled studies. The advantages of registry-based studies include a detailed description of injury severity and physiologic data acquired by trained registrars. The disadvantages are related to inconsistency of data submission, and the need to account for missing data using imputation and often propensity scoring in many multi-institutional analyses. These methods of data collection and analysis are important to evaluate changes in outcome before and after, or at different time periods following the implementation of trauma systems in a defined region. Because this is administrative and/or claims related information there is little or no information on physiologic data, injury severity, and treatment. The limitations of the most commonly used databases in population-based studies are described in Table 4-5. Despite differing approaches to study design one area of rising interest has been comparison of outcomes of inclusive and exclusive systems. As described previously, in an inclusive system, care is provided to all injured patients and involves all acute care facilities, whereas in exclusive systems specialized trauma care is provided only in high-level trauma centers that deliver definitive care. In inclusive systems, patients may be transferred to a higher level of care (trauma center) after initial stabilization based on the availability of resources and expertise in the initial treating facility. No long-term or functional outcomes data available underscores the importance of accurate triage and affirms that excessive overtriage makes treatment of minor injury inappropriately expensive and potentially disruptive of the process of care for more severely injured patients. The greatest modern challenge for which careful system performance monitoring will be critical is management of the elderly. As the American population ages the proportion of patients over 65 years who sustain significant injury continues to increase. These individuals represent a small volume of the overall trauma patient population, yet generate a disproportionate share of the cost of care. Despite being more active than their predecessors, most of these patients are afflicted with the usual comorbid conditions associated with aging. The desire to be treated by the physicians or health system with which they are familiar often results in inappropriate triage. Inability to determine whether the patient is at risk because of being injured and elderly versus elderly and acutely injured often results in delayed management of injuries or incomplete assessment deteriorating chronic comorbid conditions. Transformation of a reasonably healthy, active senior citizen to an impaired dependent is yet another burden of the disease of injury, and demands careful planning, comprehensive case management and compassionate counseling of victims and their families. They concluded that severely injured patients are more likely to survive in states with the most inclusive trauma system, independent of the triage system in place. A possible explanation for these findings includes better initial care in referring hospitals. Major advances have occurred in management of traumatic brain injury, including the benefit of high volume experience in terms of patient survival and quality of recovery. Racial and social disparity studies have defined specific issues that directly impact outcomes in these populations, and more importantly document no discriminatory barrier to trauma system access. Because any injury represents a failure of prevention, the scope of effort has broadened to the concept of an inclusive trauma system that enhances prevention education and integrates all resources into a population based, coordinated enterprise. This culture of outcome oriented performance improvement has become the model for similar efforts across all aspects of American health care. As the American health care system continues its transformation and as the clinical data ecosystem evolves to a level that supports the full gamut of health care delivery, system performance and clinical outcome measurement will drive better patient care, more efficiency, and improved population wellness. The following items are some of the major factors which will be measured and will drive continuous quality improvement for the entire trauma system. It must reflect continued focus on elimination of preventable death and optimization of potential recovery for all injury victims. This includes effective prevention of any injury, expeditious care for those at risk, and comprehensive long-term support through full reintegration into society. Trauma system function is predicated on the availability of extensive and expensive resources. Just as the commitment to quality and optimal patient care forged by trauma systems has become a model for clinical care in general, so also has the trauma system collaborative infrastructure that coordinates availability and deployment of critical resources from disparate emerged as the infrastructure that will support effective disaster response. The Donabedian model of performance assessment defines the items below as the critical factors necessary to address the statements above in a manner that defines trends and identifies opportunities for system improvement. Table 4-6 identifies multiple aspects of trauma system function and theoretical metrics that could be developed to generate a data driven, objective process for continuous performance improvement.
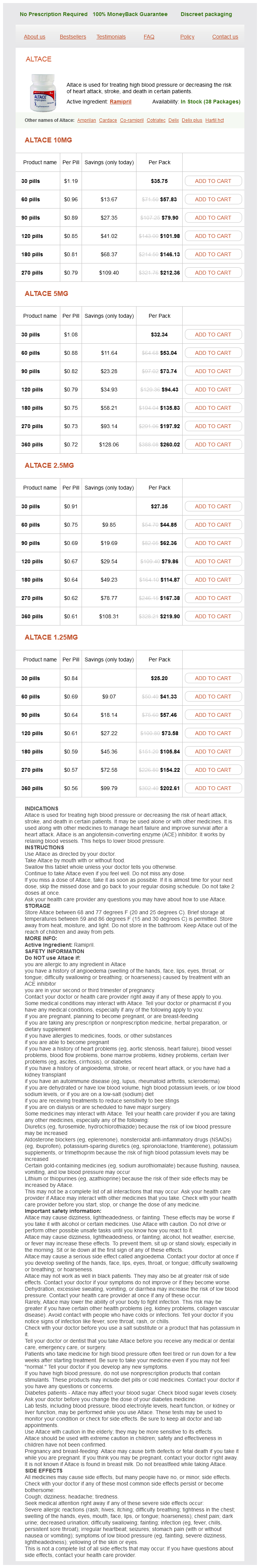
Ramipril Dosage and Price
Altace 10mg
- 30 pills - $35.75
- 60 pills - $57.83
- 90 pills - $79.90
- 120 pills - $101.98
- 180 pills - $146.13
- 270 pills - $212.36
Altace 5mg
- 30 pills - $32.34
- 60 pills - $53.04
- 90 pills - $73.74
- 120 pills - $94.43
- 180 pills - $135.83
- 270 pills - $197.92
- 360 pills - $260.02
Altace 2.5mg
- 30 pills - $27.35
- 60 pills - $44.85
- 90 pills - $62.36
- 120 pills - $79.86
- 180 pills - $114.87
- 270 pills - $167.38
- 360 pills - $219.90
Altace 1.25mg
- 30 pills - $25.20
- 60 pills - $41.33
- 90 pills - $57.46
- 120 pills - $73.58
- 180 pills - $105.84
- 270 pills - $154.22
- 360 pills - $202.61
Gastric bacterial numbers increase in the absence of gastric acid heart attack 35 buy genuine ramipril line, as in patients receiving proton pump inhibitors. Bacterial numbers are much higher in the small intestine and the density of bacteria increases from the duodenum to the terminal ileum. The presence of such large numbers is associated with very low oxygen tension, and 99. The urogenital, biliary, pancreatic ductal, and distal respiratory tracts are "sterile" in healthy individuals. In addition to the environmental factors and colonization resistance described earlier, crucial humoral and cellular host defense mechanisms exist that eliminate bacteria within sterile spaces. Initially, several primitive and relatively nonspecific host defenses including proteins such as lactoferrin, fibrinogen, and complement begin to act against invading microbes. Lactoferrin sequesters the critical microbial growth factor iron, thereby limiting microbial growth. Fibrinogen within the inflammatory fluid has the ability to trap large numbers of microbes during polymerization into fibrin. Activation of complement releases C3a and C5a, which are potent chemotaxins that recruit neutrophils and macrophages. These components enhance endothelial adhesiveness and increase vascular permeability. Complement activation can directly destroy microbial agents via formation of a membrane attack complex (composed of complement proteins C5C9) and enhance microbial phagocytosis by way of C1q and C3bi subunits. In vitro studies have shown that 5070% of a moderate inoculum is eliminated prior to the influx of phagocytic host cells. These include macrophages, dendritic cells, Kupffer cells, glial cells, mesangial cells, and alveolar macrophages. These mediators produce the signs and symptoms that we associate with infection (fever, tachycardia, tachypnea, leukocytosis, etc. The presence of endotracheal tubes, smoking, inhaled toxins, and some anesthetic agents interfere with mucocilliary clearance mechanisms, and this may predispose to pneumonia. Table 18-1 shows the most common infectious agents that cause trauma-associated infections at various anatomic sites. For traumatic injuries that involve the aerodigestive tract the most common isolates are E. A few infectious agents that can be Unfortunately, the same process that recruits neutrophils and stimulates phagocytosis and oxidative killing may also contribute to damage of host tissues. Specific anatomic locations have additional unique factors that defend against infection. Movement of the diaphragm "pumps" this fluid into the thoracic duct and from there it gains rapid access to the systemic circulation. Experimental studies show that labeled bacteria inoculated into the peritoneal cavity appear in the thoracic duct within 6 minutes and in the bloodstream within 12 minutes. Goblet cells within the respiratory mucosa secrete mucin that helps to trap bacteria. Staphylococcus aureus Methicillin-sensitive Methicillin-resistant Community pathogens Streptococcus pneumonia Haemophilus sp. We will also discuss some of the unique challenges and concerns that have been brought to the attention of surgeons during the Ebola outbreak of 2014. Rabies Rabies is a rare, potentially fatal, clinical disease caused by the rabies virus. Prior to the development of a vaccine by Louis Pasteur, bites from a rabid animal were uniformly fatal. In North America, raccoons, skunks, bats, foxes, coyotes, and bobcats are the primary reservoirs. Most patients with rabies have no documented exposure to a rabid animal, and the majority of these are associated with bat bites. Many victims underestimate the importance of a bat bite and a substantial portion do not even recall being bitten. Bats (Carnivora and Chiroptera) represent the ultimate zoonotic reservoir for the virus, as well. The rabies virus is highly labile and can be inactivated readily by ultraviolet radiation, heat, desiccation, and other environmental factors. The word "rabies" derives from the Latin rabere meaning "to rage" and refers to the clinical manifestations of the disease that include hyperactivity, disorientation, hallucinations, and bizarre behavior. Other hallmarks of the disease include an intense fear of suffocation (eg, hydrophobia and aerophobia) secondary to intense laryngeal and pharyngeal spasm. That said, it is important for the practitioner of emergency medicine/surgery to be knowledgeable about rabies since animal bites are encountered frequently in clinical practice. Humans are not routinely vaccinated against rabies, while domestic animals receive routine rabies vaccinations. The diagnosis of rabies can be made rapidly by identification of rabies virus in the brain of a potentially infected animal. This procedure can be performed most expeditiously by euthanizing the suspected animal. If the rabies test is negative, then no postexposure vaccination or prophylaxis is needed. The incidence of positive rabies tests ranges from as high as 610% in wild animals down to levels of ~1% in domestic pets. An acceptable alternative approach, if the suspected source is a domestic pet (dog, cat, ferret, etc. Immediate measures that should be taken to decrease the risk of rabies transmission include thorough washing of bite and scratch wounds with soap and water, followed by application of povidoneiodine or alcohol.