Ranitidine
General Information about Ranitidine
Ranitidine is a medication generally used for the remedy of conditions that trigger the body to supply excessive amounts of stomach acid. This medicine is used to relieve signs related to conditions such as Zollinger-Ellison syndrome, gastroesophageal reflux illness (GERD), and abdomen ulcers. It belongs to a class of drugs known as H2 blockers, which work by reducing the amount of acid produced by the abdomen.
Like any medicine, Ranitidine could cause unwanted facet effects in some people. These might embody headache, dizziness, diarrhea, constipation, and rash. It is necessary to seek the assistance of together with your doctor when you expertise any of those unwanted effects or another uncommon symptoms.
Additionally, Ranitidine may interact with other drugs similar to anticoagulants, anti-seizure medication, and sure antibiotics. Therefore, it is essential to inform your physician of any other medicines you take before starting Ranitidine therapy.
In conclusion, Ranitidine is a generally used treatment for the remedy of circumstances that cause excessive stomach acid production. It can present relief from signs similar to heartburn, stomach ache, and ulcers. Like any treatment, you will need to comply with proper dosage instructions and inform your doctor of another drugs you are taking. By doing so, you can effectively handle your situation and improve your general well being and well-being.
Stomach ulcers, also called peptic ulcers, are open sores that develop on the liner of the stomach and may cause symptoms similar to bloating, stomach pain, and nausea. Ranitidine may help heal these ulcers by decreasing the quantity of acid in the stomach, allowing the lining to heal and stopping additional harm.
Zollinger-Ellison syndrome is a rare dysfunction during which tumors in the pancreas or small gut cause the body to produce large amounts of abdomen acid, resulting in abdomen ulcers and other digestive issues. In these cases, Ranitidine is used to manage the surplus acid manufacturing and supply reduction from symptoms such as heartburn, abdomen ache, and diarrhea.
Ranitidine is out there in each prescription and over-the-counter types. Prescription power Ranitidine is often taken a couple of times a day, and over-the-counter types are taken as needed for reduction of symptoms. It is beneficial to follow the directions of your healthcare supplier or the medication label when taking Ranitidine to make sure the right dosage and length of remedy.
While most people can safely take Ranitidine, there are some who ought to avoid it. This consists of people who've a historical past of allergy symptoms to any of the elements within the medicine, those with kidney or liver illness, and pregnant or breastfeeding girls. It is important to seek the guidance of with your doctor if you fall into any of those classes before starting Ranitidine treatment.
In patients with GERD, a persistent condition where abdomen acid regularly flows again into the esophagus, Ranitidine can help alleviate signs such as heartburn, chest pain, and issue swallowing. It works by reducing the amount of acid within the stomach, which in flip reduces the irritation and harm to the esophagus attributable to the abdomen acid.
Aypar E et al: the efficacy of tissue Doppler imaging in predicting myocardial iron load in patients with beta-thalassemia major: correlation with T2* cardiovascular magnetic resonance gastritis lasting weeks purchase ranitidine with paypal. Chakraborty I et al: Non-haem iron-mediated oxidative stress in haemoglobin E beta-thalassaemia. It is unusual for the occiput to show the predominant involvement in thalassemia, but that is the case here. The paranasal sinuses, which should be aerated by this age, are quite solidly replaced by marrow. The expansion of paranasal sinuses in this disease leads to a distortion of the facial features, which is typical of thalassemia and is known as rodent facies. All the bones show squaring, or loss of their normal morphology, due to marrow packing. This is reminiscent of the Erlenmeyer flask appearance of Gaucher, a storage disease. Interestingly, bone infarcts are much less frequent in this disease than sickle cell anemia. The paraspinal soft tissue masses represent extramedullary hematopoiesis, also typical of thalassemia. This mass is a focus of site of extramedullary hematopoiesis in a patient with thalassemia and is found in the most common location for this process. The mass was subtle when the patient was 1st seen at age 9, but is much larger and more obvious 12 years later. The process is prominent in this case; the bones in cases of early myelofibrosis may appear normal. Kröger N et al: Impact of allogeneic stem cell transplantation on survival of patients less than 65 years with primary myelofibrosis. The vertebrae are lower signal than the intervertebral discs, except for residual fat around the vertebral veins. The homogeneity of the marrow changes and lack of enhancement after gadolinium administration distinguish this case from diffuse marrow replacement by tumor. The abnormality predominantly involves the medullary space, without thickening of the endosteal cortex. This is typical of myelofibrosis, which results from replacement of the fatty marrow with fibrous tissue. There is soft tissue swelling at the 1st metatarsophalangeal joint as well as both marginal and juxtaarticular erosions. This patient has developed gout secondary to the increased cellular turnover of his underlying disease process. Pseudotumor of hemophilia has a different distribution, seen most frequently in the femur/thigh and pelvis. Note also the enlargement of the femoral condyles (ballooning) relative to the femoral diaphysis. The process is relatively early, since cartilage narrowing and erosions have not yet developed. The findings are typical of either hemophilic arthropathy or juvenile idiopathic arthritis; the patient is known to be hemophilic. Given the morphology and patient gender, diagnosis of hemophilic arthropathy is probable. This is indicative of hemosiderin deposits and proves the diagnosis of hemophilic arthropathy. On these coned images, the degree of overgrowth is not apparent, but the cartilage narrowing and erosive disease is impressive. There is large subchondral cyst formation, widened trochlear notch, and significant overgrowth of the radial head. This strongly supports the diagnosis of hemophilic arthropathy with hemosiderin deposition. This is typical of hemophilic pseudotumor, despite the extensive destructive change. The mass extends into soft tissues as multiple lobulated fluid collections with enhancing rims. The soft tissue mass scallops the adjacent bone; the osseous destruction is geographic with transverse osseous excrescences. This is a typical appearance, 2° to repeated bleeding, pressure erosion, and periosteal lifting. This could be due to recurrent bleeding but biopsy showed transformation to malignant hemangioendothelioma. T2 and postcontrast imaging demonstrated nonspecific hyperintensity and enhancement, respectively (not shown). It occurs in diabetic patients (note the vascular calcification) and is very difficult to treat. Although bone may show reactive edema to nearby soft tissue infection and may be difficult to differentiate from osteomyelitis, the sinus track leading to confluent marrow abnormality is diagnostic. There is deossification both on the femoral head (note that the cortex has lost its crisp distinctness) and acetabulum. There is also destruction of the talonavicular joint and debris contained within a large joint effusion. These findings are typical of Charcot joint; talonavicular is a common site in diabetic patients.
However gastritis upper gi bleed ranitidine 150 mg buy with amex, in research settings, potentially promising candidates do exist for disease prevention. Immunosuppression the earliest studies of therapies to prevent beta-cell destruction used immunosuppressive agents. The combination of inability to cure diabetes and toxicities associated with cyclosporine (in particular, nephrotoxicity and concern about increased risk of malignancy) ruled out its acceptance for use. Other immunosuppressive agents used in subsequent studies, such as prednisone and azathioprine, demonstrated relatively little effect in disease intervention. However, even when efficacious, for the majority of subjects, the beneficial effect was not durable. C-Peptide Loss After Hyperglycemia After diabetes is diagnosed, levels of C-peptide can be used to assess remaining beta-cell function. C-peptide levels are usually measured in the fasting state, after intravenous glucagon, or with a standard liquid meal. Such measurements are primarily of importance for trials of therapies to alleviate loss of insulin secretion after diagnosis. Determination of the C-peptide concentration provides the best current measure for assessing the impact of new therapies. The usual history is one of severe stress associated with hyperglycemia that resolves within days to 1 month. Concerns related to the activation of Epstein-Barr virus infection, the duration of C-peptide preservation, and the protocol by which the drugs are administered have further limited their development. Much of the excitement derives from the specificity of the therapy and the relatively low risk compared with immunosuppression. The basic concept behind most such therapies is the induction of lymphocytes that target a given beta-cell antigen and, on encountering the target antigen. The results of the parenteral trial did not demonstrate a reduction in the risk of developing diabetes. Perhaps for these reasons, along with improvements in facets directed at improving diabetes management, it appears the procedure peaked in the mid- to late 2000s, with declines in the number of procedures performed in the United States thereafter. Yet until studies emanated from Edmonton, Canada, in the early 2000s, the results of islet transplantation were-with full transparency with regard to their efficacy-considered poor by many over a period of 2 decades. This so-called Edmonton protocol has subsequently been tested in a series of specialized centers throughout North America and Europe. It is clear that in many centers, albeit with varying degrees of success, islet cell transplant can prove effective. For most of the patients who achieve insulin independence, resumption of use of low doses of insulin is necessary within 2 years and by 5 years, the benefits of the form of therapy wane. In addition, the increasing use of long-term continuous glucose monitoring combined with improvements in modes of insulin delivery. The usual mode of therapy for such situations consists of substituting the type or formulation of insulin, administration of oral antihistamines for immunoglobulin Emediated local reactions, followed by insulin desensitization or addition of small amounts of glucocorticoids to the insulin injected for local delayed hypersensitivity reactions. This syndrome is quite rare, is often associated with nonorganspecific autoimmunity, and treatments usually involve various forms of immunosuppression. Interestingly and for reasons unknown, the disease occurs most commonly in persons of Asian descent. The symptoms and signs are related to the presence of hyperglycemia and the resulting effects on fluid and electrolyte balance; they include polyuria, polydipsia, polyphagia, weight loss, and blurred vision. In children in particular, the onset of symptoms can occur over a brief period, and families may be able to date the onset with considerable accuracy. Variable effects on mental status may be seen, ranging from slight drowsiness to profound lethargy and even coma if the condition has been untreated for a significant period. Laboratory Findings Plasma glucose concentrations at presentation are elevated, usually in the range of 300 to 500 mg/dL. If the presentation is uncomplicated, the remainder of the fluid and electrolyte measurements may be completely normal. At presentation the C-peptide level (a surrogate marker for insulin secretion) is generally in the low normal range and declines over time. However, residual C-peptide may be detected throughout the natural history of diabetes. In reference laboratories, pancreatic autoantibodies are present in ~98% of individuals at diagnosis, but most commercial laboratories do not provide either the full spectrum of assays or equivalently sensitive or specific assays, resulting in both false negative and positive assays (discussed previously). Furthermore, antibody titers diminish over time and may be less prevalent in certain ethnicities. Intensive therapy consisted of insulin administration by an external pump or by three or more daily insulin injections. The dosage was adjusted according to the results of self-monitoring of blood glucose performed at least four times per day as well as dietary intake and anticipated exercise. Patients in the intensive treatment group visited their centers each month and had more frequent contacts with a member of the health care team, usually weekly, to review and adjust their regimens. Conventional therapy consisted of one or two daily injections of insulin, including mixed intermediate and rapid-acting insulins, daily self-monitoring of urine or blood glucose, and education about diet and exercise. The goals of conventional therapy included absence of symptoms of hyperglycemia; absence of ketonuria; maintenance of normal growth, development, and ideal body weight; and freedom from frequent severe hypoglycemia. Although only 5% of the subjects in the intensive treatment group were able to sustain the goal of a normal HbA1c over time, they nevertheless did have significantly lower average values (approximately 7%) over time than the subjects in the conventional treatment group (approximately 9%). Average capillary blood glucose profiles in the intensive treatment group were 155 ± 30 mg/dL, compared with 231 ± 55 mg/dL in the conventional therapy group (p < 0.
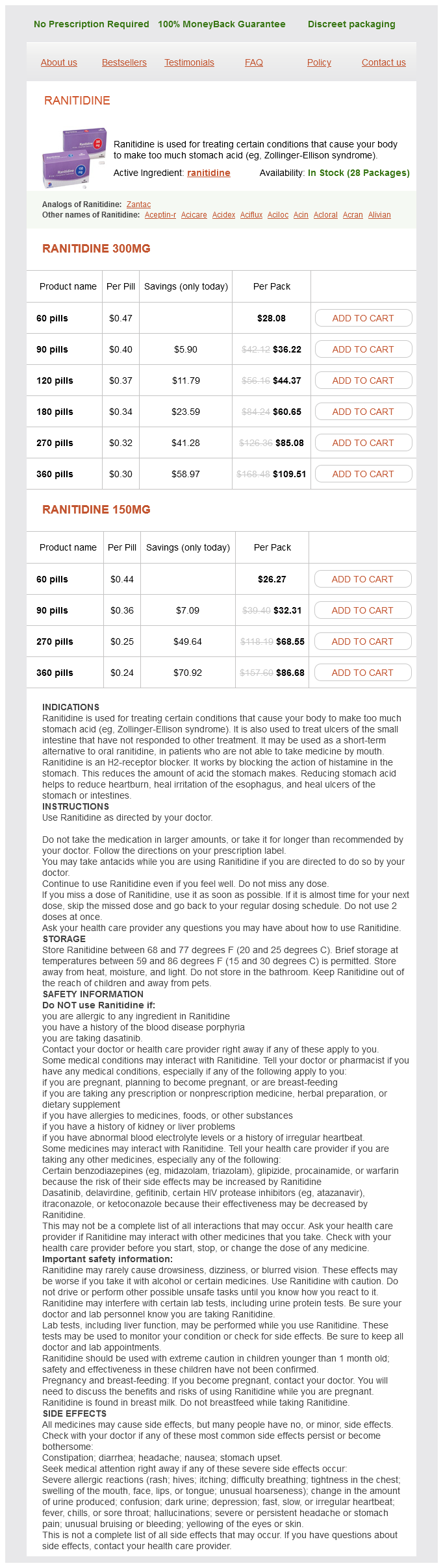
Ranitidine Dosage and Price
Ranitidine 300mg
- 60 pills - $28.08
- 90 pills - $36.22
- 120 pills - $44.37
- 180 pills - $60.65
- 270 pills - $85.08
- 360 pills - $109.51
Ranitidine 150mg
- 60 pills - $26.27
- 90 pills - $32.31
- 270 pills - $68.55
- 360 pills - $86.68
Prepatellar and pretibial bursitis gastritis not going away purchase discount ranitidine line, 836839 - diagnostic checklist, 837 - differential diagnosis, 837 - prognosis, 837 Presternal dislocation, 53 Prominent medial head of triceps, anconeus epitrochlearis vs. Pronator teres, 321 Proximal fibula fracture, proximal tibiofibular joint and, 658661 - diagnostic checklist, 659 - prognosis, 659 - staging, grading, & classification, 659 Proximal hamstring injury, 600605 - diagnostic checklist, 602 - differential diagnosis, 601 - prognosis, 602 - staging, grading, & classification, 602 Proximal humerus fracture. Pseudo-Boutonnière deformity, collateral ligament injury, finger and thumb, 457 Pseudoaneurysm, wrist and hand, 479 - aneurysm vs. Pulley injury, flexor tendon injury, wrist and fingers, 463, 464 Pulley system, flexor tendon injury, wrist and fingers, 463 Pump bump. Radiation osteitis, fracture from, 13 Radiculopathy, lumbar, piriformis syndrome and nerve injuries of pelvis vs. Radiographic union, 7 Radiography - knee injury, 636 - traumatic injury, 5 Radiolunate fracture. Radioulnar joint instability, distal, 398401 - diagnostic checklist, 400 - isolated, without fracture, 400 - normal motion, 399 - prognosis, 400 - proper positioning, 399 - signs/symptoms, 400 - staging, grading, & classification, 400 Radioulnar ligament, dorsal, 446 Radius fracture - distal, 380385 associated abnormalities, 381 classifications, 382 diagnostic checklist, 382 postoperative imaging, 390393 complications, 391 diagnostic checklist, 391 prognosis, 391 treatment options, 391 prognosis, 382 staging, grading, & classification, 381382 - distal metaphyseal, trauma-related osteolysis, pediatric wrist vs. Rotator cuff denervation syndromes, 220223 - diagnostic checklist, 222 - differential diagnosis, 221 - prognosis, 222 - staging, grading, & classification, 222 Rotator cuff impingement, 102107 - adhesive capsulitis vs. Salter-Harris fracture, 1823 - ankle, 942945 diagnostic checklist, 943 differential diagnosis, 943 staging, grading, & classification, 943 - diagnostic checklist, 20 - juvenile distal forearm, 375, 378 - malleolus fracture vs. Sever disease, 10401041 - associated abnormalities, 1041 - diagnostic checklist, 1041 - differential diagnosis, 1041 - prognosis, 1041 Severe developmental dysplasia, hip dislocation vs. Shoulder impingement, internal, 208213 - associated abnormalities, 210 - diagnostic checklist, 210 - differential diagnosis, 209 - prognosis, 210 - staging, grading, & classification, 210 Shoulder instability - microinstability, 214215 associated abnormalities, 215 diagnostic checklist, 215 differential diagnosis, 215 internal impingement, shoulder vs. Snapping hip syndrome, 592595 - diagnostic checklist, 593 - differential diagnosis, 593 - externally, ligamentum teres vs. Spring ligament injury, foot, 958, 962965 - associated abnormalities, 963 - deltoid ligament injury vs. Stener lesion, hand and wrist - collateral ligament injury, finger and thumb, 457 - definition, 371 Stenosing tenosynovitis, 1047 Sternoclavicular joint dislocation, clavicle fracture vs. Straddle fractures, isolated pelvic injuries, traumatic, 525 Strawberry picker palsy. Stress injury, leg, 672677 - diagnostic checklist, 674 - differential diagnosis, 673674 - prognosis, 674 - staging, grading, & classification, 674 Stress/insufficiency fractures, 861. Subluxation tendinopathy, biceps, 147 Subperiosteal new bone formation, 25 Subscapularis, 48 - biceps tendon dislocation anterior to , 155 Subscapularis recess effusion, subscapularis tear vs. Supinator fat pad sign, positive, radial head/neck, 263 Supinator injury, brachialis injury vs. Synovial fringe, elbow, 336337 - diagnostic checklist, 337 - differential diagnosis, 337 - prognosis, 337 Synovial hemangioma, intraarticular bodies of elbow vs. Thompson system, scapula trauma, 66 Thoracic cage muscle injury, abdominal muscle injury vs. Tibial tendon pathology, posterior, flexor hallucis longus tendon tear, impingement, and tendinopathy vs. Tibiofemoral dislocation, 652657 - associated abnormalities, 653 - diagnostic checklist, 654 - differential diagnosis, 653 - prognosis, 654 - staging, grading, & classification, 653654 Tibiofibular joint, proximal, and proximal fibula fracture, 658661 - diagnostic checklist, 659 - prognosis, 659 - staging, grading, & classification, 659 Tibiofibular joint dislocation, proximal, proximal tibiofibular joint and proximal fibula fracture, 659 Tibiospring ligament tears, 998 Tietjen classification, pectoralis injury, 93 Tillaux fracture, pilon fracture vs. Tug lesion - humerus, 8889 diagnostic checklist, 89 differential diagnosis, 89 prognosis, 89 - pelvis. Ultrasound, 4 - knee, 637 - shoulder, 47 Unicameral bone cyst, 13 - Sever disease vs. Volar ligaments, 403, 446 Volar perilunate dislocation, 415 Volar plate injury, 434 - collateral ligament injury, finger and thumb, 457 Volar radioulnar ligament, 446 Volkmann contracture, 236 - carpal instability, 450455 diagnostic checklist, 452 differential diagnosis, 452 prognosis, 452 staging, grading, & classification, 452 - collateral ligament injury, fingers and thumb, 456461 diagnostic checklist, 458 mechanisms of injury, 458 prognosis, 458 staging, grading, & classification, 458 - die-punch fracture, 386387 diagnostic checklist, 387 differential diagnosis, 387 distal radius, 384 prognosis, 387 staging, grading, & classification, 387 - distal radioulnar joint instability, 398401 diagnostic checklist, 400 isolated, without fracture, 400 natural history & prognosis, 400 normal motion, 399 proper positioning, 399 signs/symptoms, 400 staging, grading, & classification, 400 - distal radius fracture, 380385 postoperative imaging, 390393 complications, 391 diagnostic checklist, 391 prognosis, 391 treatment options for, 391 - extensor tendon injury, 468473 anatomic zones, 470 diagnostic checklist, 470 mechanisms of injury, 470 prognosis, 470 - extrinsic (capsular) ligaments, 360 - finger fracture and dislocation, 432437 diagnostic checklist, 434 mechanisms of injury, 434 prognosis, 434 staging, grading, & classification, 434 - flexor tendon injury, 462467 anatomic zones, 462467 diagnostic checklist, 464 mechanisms of injury, 464 prognosis, 464 staging, grading, & classification, 463 - fractures, ossicle and sesamoid injury vs. Watson-Jones procedure, 1043 Weakness, depressor muscle, humeral head, rotator cuff partial-thickness tear, 118 Weinstabi classification, Achilles tendon tear and tendinopathy, 988 Wii-itis, 97 Wood, foreign body, 39, 41, 42 Wrist and hand - acronyms and eponyms, 370373 - anatomic considerations, 360 - carpal dislocation, 414419 associated fracture patterns, 415 carpal instability vs. Introduction to Arthritis Arthritis Classic Appearance of Arthritic Processes When an arthritic process is well established in a particular patient, it will usually achieve a typical appearance, which allows diagnosis by means of imaging. At such a moderately early or mid stage of disease, radiographs are usually sufficient to make the correct diagnosis. The diagnosis usually depends on the location of the joint abnormalities and a host of other radiographic characteristics. Location of involved joints can often eliminate some diagnoses and raise the probability of others. For example, distal interphalangeal joint disease is commonly seen in psoriatic arthritis, osteoarthritis, and erosive osteoarthritis. Common locations of joint involvement are illustrated in diagrammatic fashion in this section. Note the joints that are involved earliest and most commonly are distinguished from those involved less frequently or in endstage disease. While the location of the joints involved certainly contributes to establishing a list of reasonable diagnoses, the lists can be relatively long, as in the examples above. There are several other parameters that are useful in honing that list to a single diagnosis that are outlined in the tables that follow. Further explanation regarding some of these parameters may be helpful, as follows. There are a minimal number of arthritic processes that affect children (juvenile inflammatory arthritis, hemophilic arthropathy, inflammatory bowel disease arthropathy, and septic joint) and teenagers (in addition to those affecting children, early onset adult rheumatoid arthritis and ankylosing spondylitis). Some diseases are gender specific (hemophilic arthropathy and hemochromatosis), while others are found in one gender far more frequently (gout, ankylosing spondylitis, chronic reactive arthritis in males, and rheumatoid arthritis in females). Some arthritides are purely erosive; rheumatoid arthritis is the hallmark for this group. Other processes may be mixed, sometimes starting with erosions but progressing to osteophytes (as in pyrophosphate arthropathy or gout) or starting with periostitis and progressing to mixed erosions and osteophytes (as in psoriatic arthritis or chronic reactive arthritis). These processes tend to be distinctive for each type of arthritis by the time they are well established; between evaluating the character of the process and its primary location in an individual, the diagnosis can usually be secured. Rheumatoid arthritis is especially well known for appearing bilaterally symmetric.