Risperdal
General Information about Risperdal
Schizophrenia is a continual and extreme psychological disorder characterized by disordered thinking, conduct, and notion of reality. It impacts roughly 1% of the global population and is often identified in late adolescence or early adulthood. Individuals with schizophrenia may expertise hallucinations, delusions, disorganized thinking, and issue with concentration and motivation. Risperdal helps alleviate these signs by blocking the exercise of dopamine and serotonin, two neurotransmitters concerned in temper regulation and notion.
Like any treatment, risperidone might trigger unwanted effects, similar to drowsiness, dizziness, weight achieve, and increased threat of growing diabetes. It is essential to debate any potential unwanted effects with a physician before starting therapy. Long-term use of this medicine may result in a serious condition called tardive dyskinesia (TD), characterised by uncontrollable actions of the face and physique. It is important to frequently monitor for TD to forestall irreversible damage.
Risperdal is a generally prescribed treatment for the treatment of schizophrenia, bipolar mania, and irritability associated with autistic dysfunction. Also recognized by its generic name risperidone, this psychotropic agent has been on the market since 1993 and has been confirmed to effectively manage symptoms related to these conditions.
The use of risperidone has additionally been controversial, as it has been linked to an elevated risk of strokes and cardiac occasions, particularly in aged sufferers with dementia-related psychosis. The U.S. Food and Drug Administration (FDA) has issued a black field warning for these potential risks, and it's essential to make use of this medication with caution on this population.
It is value noting that Risperdal may interact with other medicines, together with antibiotics, antidepressants, and antihistamines. It is essential to inform a healthcare skilled about any current drugs or supplements earlier than starting treatment with risperidone.
Risperdal is available in numerous types, together with tablets, injections, and dissolving tablets, making it a versatile treatment option for various individuals' wants. The dosage and length of therapy differ and ought to be determined by a healthcare professional, considering an individual's medical history and symptoms' severity.
In conclusion, Risperdal is a well-established treatment for the remedy of schizophrenia, bipolar mania, and irritability related to autistic disorder. While it can successfully handle symptoms, it's not a remedy for these conditions. Like any treatment, its use should be intently monitored by a healthcare professional, and any potential side effects or interactions should be discussed brazenly. With correct medical care, people can experience improved quality of life and better management of their symptoms with the assistance of risperidone.
In latest years, risperidone has also gained recognition for its use in treating irritability associated with autistic disorder. Autism spectrum disorder (ASD) is a developmental dysfunction that impacts one in fifty nine children in the United States. Children with ASD often expertise difficulty with social interactions, communication, and repetitive behaviors. In some cases, they could also display aggressive and self-injurious behaviors, which may be challenging for folks and caregivers to handle. Risperdal has been shown to reduce the intensity and frequency of these behaviors, enhancing the general quality of life for these individuals and their households.
Bipolar dysfunction, also called manic-depressive sickness, is a mental dysfunction that causes excessive shifts in moods, energy and activity levels. Bipolar mania is the most typical form of this dysfunction and is characterized by intervals of elevated or irritable moods, increased vitality, and impulsive habits. Risperdal is often prescribed at the aspect of mood stabilizers to help handle manic episodes and forestall relapses.
From a flow perspective treatment uveitis order risperdal once a day, it has been proved that independent catheter lines offer more consistently adequate and high flow than the attached lines. Ultrasonography- or fluoroscopy-based methods to locate prior insertion and/or to guide the vein cannulation have reduced the incidence of failure, the time spent in catheterization, and the incidence of traumatic complications. In brief, a direct venipuncture of femoral vein is performed and a souple metallic guidewire is passed through the needle. After the needle is removed, vein dilation is performed by means of a large catheter dilator (or desilet). Large-bore dual-lumen catheter placement then is performed after removing the desilet over the metallic guidewire left in the vein. In brief, the jugular vein is punctured with a large-bore needle, and then two metallic guidewires are introduced successively into the vessel. Thereafter, twice in a row a nonpeelable introducer dilator catheter is introduced into the vein over the guidewire, permitting the insertion of the cannulas. After each procedure, the introducer dilator is removed while the catheter is left in the vein and clamped. In that case, twice in a row, cannulas are stowed securely on tunneler, passed downward under the skin, and exited 10 to 15 cm from cervical entrance. The third step consists in customizing the catheter length to patient anthropometrics and ensuring subcutaneous anchorage. Briefly, cannula lengths are adjusted and cut to position catheter tips 1 to 2 cm apart at the junction of superior vena cava and right atrium. Thereafter, cannulas and extension pieces are strap stowing, pushed back under skin, and anchored either by purse-string along subcutaneous track or Dacron patch fixed in the subcutaneous tunnel. A peelable introducer-dilator then is inserted into the vein over the guidewire to prepare dual-lumen catheter introduction; the second step consists of passing upward the double-lumen catheter (bottom-up) under the skin chest by means of a peelable tunneler catheter; the third step consists in grabbing the catheter tip exiting from subcutaneous tunnel at the neck base and then passing the guidewire exiting from the vein (upside down) through the catheter to its hub. The double-lumen catheter then is pushed back through the sheath over the guidewire into the vessel. During this procedure, the step-by-step dialysis catheter is pushed back while the sheath is peeled away progressively and finally removed. Internal jugular vein access is preferable in the absence of life-threatening conditions; it uses an easily accessible vein that gives access for transjugular renal biopsy at the same time if needed. In these cases, a nontunneled double-lumen polyurethane catheter inserted in the femoral vein with local anesthesia is usually the best option. In these cases, a tunneled soft polyurethane or silicone rubber double-lumen catheter or duo-catheter inserted in the internal jugular vein is considered the best option38. Femoral vein access represents a primary option in emergency conditions and a secondary option in patients who are bedridden with severe neurologic disorders, are receiving ventilatory assistance (tracheotomy), or have multiple-organ failure. A double-lumen semirigid polyurethane catheter is the best catheter for starting the dialysis. The insertion site is located approximately 1 to 2 cm below the crural arcade and 1 cm medial to the femoral artery. The incidence of deep venous thrombosis and stenosis is reduced with use of the internal jugular vein, in comparison with that of femoral and subclavian catheter use. Straight or kinked double-lumen catheters exiting in an unfavorable area (middle or upper neck) are uncomfortable, difficult to fix, protected by dressing, and more exposed to infections. Tunneled soft polyurethane and silicone rubber catheters (double-lumen catheter, use of two catheters, split catheter) inserted into the internal jugular vein are clearly preferable to reduce the infectious risk, to improve patient comfort, and to facilitate care. Percutaneous catheter insertion into the internal jugular vein in a low position is suitable to prevent catheter kinking and dysfunction. The left internal jugular approach should be used only when the right vein is not possible. Subclavian vein cannulation for hemodialysis should no longer be used or should be regarded as the last resort. Subclavian placement of a catheter entails a major risk of stenosis or thrombosis of the host vein, compromising the chance of creating a fistula in case of no recovery of acute kidney injury. In that case, soft catheters made of silicone rubber are preferred for the subclavian approach. The right subclavian vein is preferable to reduce catheter length and improve flow performances. Short, soft cannulas (2025 cm) are indicated to prevent cardiac trauma (atrial and ventricular perforation). Correct positioning of the distal tip is essential to prevent catheter dysfunction. The tip of a chest catheter passing through the superior vena cava system should be located at the junction of the superior vena cava and the right atrium. Fluoroscopy or chest radiograph is needed to check the correct position of the catheter and tip after insertion and before use. For a thoracic catheter inserted on the right side in an adult patient, 20 to 25 cm is the optimal length; 3 or 4 cm more are required when a catheter is inserted on the left side. The tip of a femoral catheter accessing the inferior vena cava system should be positioned in the central lumen of the inferior vena cava. For a femoral catheter to reach the inferior vena cava in an adult 30 to 35 cm is the length needed. Strict aseptic conditions and maximal sterile barrier precautions in catheter handling must be used at all times. The use of a transparent plastic dressing has been reported to facilitate monitoring of the catheter exit site and to reduce infection risk.
Solute clearance can be expressed in the following ways: whole blood medicine questions buy risperdal overnight, blood water, plasma, dialysateside, and whole body. Blood flow is paramount with respect to the diffusive and convective removal capacity of a dialyzer. Special blood ports are created to achieve a uniform distribution of the flow inside the blood compartment and to obtain full utilization of the membrane surface. All of the components described play a role in the final efficiency of the system and help explain the mechanisms operating in different techniques, such as hemodialysis (prevalently diffusion-based with low-flux membranes), high-flux dialysis (mixed diffusion and convection with internal filtration and backfiltration), and hemodiafiltration (mixed diffusion and convection with reinfusion external to the filter). Evolution of synthetic membranes for blood purification: the case of the Polyflux family. Permeability and secondary membrane formation of a high flux polysulfone hemofilter. Blood and dialysate flow distributions in hollow-fiber hemodialyzers analyzed by computerized helical scanning technique. Chapter 150 / Solute and Water Transport in Hemodialysis: Dialyzers, Flow Distribution, and Cross-Filtration 918. What clinically important advances in understanding and improving dialyzer function have occurred recently A new hemodialysis treatment associating a membrane highly permeable to middle molecules with a closed circuit dialysate system. New polyether sulfone dialyzers attenuate passage of cytokine-inducing substances from pseudomonas aeruginosa contaminated dialysate. Renal versus continuous versus intermittent therapies for removal of uremic toxins. Creatinine transfer between red cells and plasma: a comparison between normal and uremic subjects. Enhancement of convective transport by internal filtration in a modified experimental hemodialyzer: technical note. Dialysate flow distribution in hollow fiber hemodialyzers with different dialysate pathway configurations. A new scintigraphic method to characterize ultrafiltration in hollow fiber dialyzers. Present the fundamentals of biocompatibility of membranes and other factors contributing to the biocompatibility of dialysis. Discuss the findings of meta-analyses concerned with the effect of biocompatibility on treatment outcomes. From a clinical perspective, it is appropriate to classify dialysis membranes according to permeability and biocompatibility characteristics. On the basis of chemical composition, membranes are grouped in those made of unmodified cellulose (Cuprophan), those in which the cellulose structure is modified by replacing hydroxyl ions with hydrophobic substances and those based on synthetic polymers. Hydrophobic polymers require to be rendered hydrophilic for improving solute transport, either by blending with hydrophilic agents. However, reactivity to blood contact is exhibited by all membranes to some extent, Biocompatibility may be defined as "the ability of a biomaterial to perform its desired function with respect to a medical therapy, without eliciting any undesirable local or systemic effects in the recipient of that therapy, but generating the most appropriate beneficial response (. Contact with these materials may activate a variety of biological responses, involving humoral and cellular pathways, with clinical sequelae. Initially, biocompatibility studies mainly focused on the interaction between blood and dialysis membranes. To date, the concept of biocompatibility has greatly evolved and it may be regarded as the sum of interactions and biological responses elicited with blood exposure to all components of the hemodialysis system. This definition also includes the effects induced by manufacturing processes, sterilization modes, contaminants, leachables and particles. In this chapter we discuss the available evidence on the main issues related to the biocompatibility of the dialysis Chapter 151 / Biocompatibility of the Dialysis System because a universal biocompatibility does not exist: the absence of response in a single biological pathway does not automatically avoid activation of others. Protein adsorption is a complex phenomenon governed by hydrophobic and electrostatic interactions, hydrogen bonding and Van der Waals forces. Furthermore, it is influenced by several factors related to blood composition, chemical properties of proteins, physicochemical membrane characteristics (surface roughness, thickness, porosity, composition, hydrophobicity and charge) and operating conditions within the dialyzer (blood flow dynamics and temperature). The second is a dynamic adsorption of low and medium molecular weight proteins within the membrane, which is dependent upon membrane characteristics and limited by its permselectivity46. Adsorption of plasma proteins on dialysis membranes is of critical importance for their biocompatibility. Once adsorbed, proteins undergo conformational changes with possible autoactivation. Adsorbed proteins also modulate the membrane bio-reactivity, by triggering the humoral and cellular pathways. It has been shown indeed that protein layers with a low albumin/fibrinogen ratio may increase the thrombogenicity, by enhancing platelet adhesion to different membranes. Finally, protein adsorption may either modulate the biocompatibility of some synthetic membranes with great absorptive capability, by removing cytokines, anaphylatoxins and complement factor D, or impair both diffusive and convective transport, by forming a secondary resistance to mass transfer58. Complement Activation the complement system is a potent mechanism for the initiation and amplification of anaphylactic, oxidative and inflammatory responses. In the 1970s, Craddock and colleagues first proved that the transient leukopenia, observed with Cuprophan membranes, was due to pulmonary vascular leukostasis resulting from complement activation16. Thereafter, the system converges on a common pathway where C5 is cleaved into C5a and C5b, via the classical or alternative C5 convertase. Finally, C5b recruits other components to form the terminal complement complex C5b-9, which causes cellular lysis, once inserted in cell membranes. Complement activation also releases the anaphylatoxins C3a and C5a, which bind to specific receptors on leukocytes, mast cells and endothelial cells. Anaphylatoxins may induce vasodilation, chemotaxis, mast cell degranulation and leukocyte activation. C5a and soluble C5b-9 activate platelets and up-regulate the expression of adhesion molecules, thereby promoting interactions between leukocytes and endothelial cells9,17. Finally, animal models on the pathogenesis of acute lung injury have implicated the role of anaphylatoxins and soluble C5b-918,19.
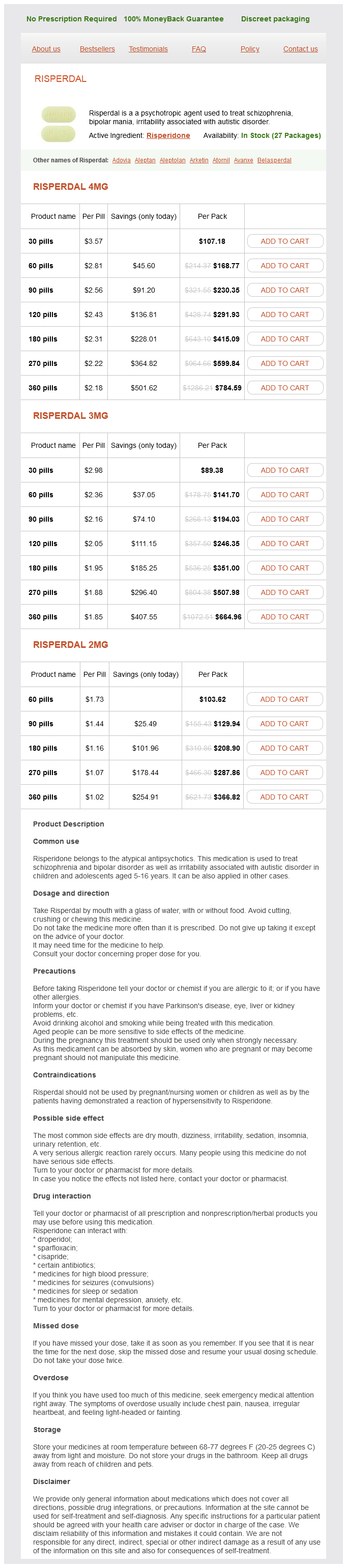
Risperdal Dosage and Price
Risperdal 4mg
- 30 pills - $107.18
- 60 pills - $168.77
- 90 pills - $230.35
- 120 pills - $291.93
- 180 pills - $415.09
- 270 pills - $599.84
- 360 pills - $784.59
Risperdal 3mg
- 30 pills - $89.38
- 60 pills - $141.70
- 90 pills - $194.03
- 120 pills - $246.35
- 180 pills - $351.00
- 270 pills - $507.98
- 360 pills - $664.96
Risperdal 2mg
- 60 pills - $103.62
- 90 pills - $129.94
- 180 pills - $208.90
- 270 pills - $287.86
- 360 pills - $366.82
A meta-analysis of the relative efficacy and toxicity of single daily dosing versus multiple daily dosing of aminoglycosides treatment 11mm kidney stone risperdal 2 mg order with amex. Propensity-based study of aminoglycoside nephrotoxicity in patients with severe sepsis or septic shock. Evaluating real-life clinical and economical burden of amphotericin-B deoxycholate adverse reactions. Incidence, Predictors, and Impact on Hospital Mortality of Amphotericin B Nephrotoxicity Defined Using Newer Acute Kidney Injury Diagnostic Criteria. Amphotericin B lipid complex in the management of invasive fungal infections in immunocompromised patients. Safety and efficacy of low-dose liposomal amphotericin B as empirical antifungal therapy for patients with prolonged neutropenia. Comparison of nephrotoxicity associated to different lipid formulations of amphotericin B: a real-life study. Amphotericin B deoxycholate versus liposomal amphotericin B: effects on kidney function. Interaction between fluids and vasoactive agents on mortality in septic shock: a multicenter, observational study. Effect of administration route on the renal safety of contrast agents: a meta-analysis of randomized controlled trials. Nephropathy after administration of iso-osmolar and low-osmolar contrast media: evidence from a network meta-analysis. Prevention of contrastinduced nephropathy with sodium bicarbonate: a randomized controlled trial. Sodium bicarbonate therapy for prevention of contrast-induced nephropathy: a systematic review and meta-analysis. Comparison of usefulness of sodium bicarbonate versus sodium chloride to prevent contrastinduced nephropathy in patients undergoing an emergent coronary procedure. Sodium bicarbonate for the prevention of contrast induced-acute kidney injury: a systematic review and meta-analysis. Sodium bicarbonate versus sodium chloride and oral N-acetylcysteine for the prevention of contrast-induced nephropathy in advanced chronic kidney disease. Chawla management, avoidance of nephrotoxic agents, hemodynamic management, and renal replacement therapy. In addition, there has been in the past decade recent efforts aimed at looking at fluids and their impact on kidney function. Recent data have emerged that implicate chloride in the development of acute kidney injury. These efforts have yielded new information as to pathophysiology at the cellular and subcellular level. Much of the recent focus has been on inflammation, immune dysregulation, and oxidative injury. Review the current literature guiding fluid type and amount of resuscitation in treating acute kidney injury. Mainstays of therapy include volume 308 Section 11 / Prevention and Treatment: General Treatment Concepts research has focused on the types of fluids administered and kidney injury. Much of the recent effort has focused on the use of balanced versus chloride-rich solutions, colloids versus crystalloids, and synthetic colloids (starches). These new targets have been correlated to certain types of kidney injury, such as metalloproteinase, which are reflective of cellular dysfunction. Others include intermedin, adenosine, inducible nitric oxide synthase, vitamin D, and sphingosine 1 phosphate and are implicated variously in inflammation, apoptosis, and oxidative damage. There are, however, some candidate therapies that have been studied recently that show promise in certain types of kidney injury. Recently, research has focused on the types and amounts of fluids in the treatment of prerenal azotemia. The rationale for this strategy has been the restoration of cardiac output, improvement in systemic blood pressure, and the maintenance of renal perfusion via the augmentation of transglomerular pressure gradient. On a cellular level, fluid overload can lead to changes in microanatomy, defects in oxygen and metabolite transfer, and capillary and lymphatic congestion. Many authorities now endorse a guided approach to fluid management, although how this is achieved is still debated. Inflammation, immune hyperreactivity, and oxidative stress have been elucidated in renal ischemia/reperfusion injury, toxic insult, and sepsis. Alpha Lipoic Acid Endothelial dysfunction caused by oxidative stress has been implicated in kidney injury. A similar study from the same year evaluated more than 200 patients with baseline kidney dysfunction (defined as a creatinine clearance of less than 60 mL/minute) who were to undergo percutaneous coronary intervention and receive contrast intravenously. However, there is a considerable amount of ongoing and completed animal research that points to an improved surrogate and clinical outcomes, including in disease processes such as ischemia-reperfusion injury,30 sepsis,31 toxic injury,23,32 and obstructive aeropathy. Selenium administration was associated with improved metrics of serum creatinine, urea, and histopathologic evidence of injury in a rat model of cisplatin-induced kidney injury. An additional 36 patients were evaluated in a 2012 study for creatinine clearance and progression to renal replacement therapy. Secondary end points, consisting of levels of markers of inflammation, were also lower. Administered intravenously, it is filtered readily across the glomerulus and taken up by renal tubular cells within 30 minutes, where it is found in high concentrations.