Rumalaya
General Information about Rumalaya
Usage and Dosage:
Rumalaya is a potent blend of herbs like Boswellia, Guggulu, and Shallaki, which have anti-inflammatory properties. These herbs are known to reduce joint irritation and provide relief from ache and stiffness. The complement also contains Indian Bedellium, which is a pure analgesic, and Rasna, which helps with muscle and joint rest.
Benefits of Rumalaya:
Rumalaya works by targeting the basis cause of joint pain and stiffness – irritation. Inflammation can be attributable to various elements like age, overuse of joints, and chronic well being situations like arthritis. The lively components in Rumalaya assist reduce the production of inflammatory enzymes, thereby lowering irritation and ache. The herbs also stimulate the production of synovial fluid, which acts as a lubricant for joints, promoting higher motion and adaptability.
Rumalaya is on the market in tablet form and may be easily incorporated right into a day by day routine. It is recommended to take one tablet twice a day after meals for a minimal of three months to see desired results. However, it's at all times advisable to seek the assistance of a healthcare skilled earlier than beginning any new complement.
Although Rumalaya is a natural supplement, it is important to take certain precautions earlier than starting the course. Pregnant and breastfeeding women should consult a well being care provider earlier than using the product. Additionally, people with pre-existing medical circumstances like diabetes, hypertension, and bleeding disorders also wants to seek the advice of their physician before beginning the complement.
In conclusion, Rumalaya is a highly effective solution for sustaining healthy joints and decreasing joint pain and stiffness. Its pure composition, coupled with its potent anti-inflammatory properties, makes it a safe and dependable alternative for individuals of all ages. Whether you're an athlete seeking to improve joint operate or an growing older adult looking to maintain joint health, Rumalaya is an ideal option to maintain your joints healthy and pain-free.
Rumalaya has a variety of benefits in relation to joint health. Its highly effective anti-inflammatory properties make it an effective solution for reducing joint ache, swelling, and stiffness. It can even assist in bettering joint mobility and flexibility, making daily duties easier for individuals with joint problems. The complement may also be used to stop age-related joint issues by sustaining the well being of cartilage and connective tissues.
The Basics of Rumalaya:
In at present's world, where we are continually juggling a number of responsibilities and main an lively lifestyle, joint health is often neglected. Joint ache and stiffness could make even the best tasks seem difficult and have an result on our general well-being. This is where Rumalaya comes into the picture.
Rumalaya is a natural supplement that has been particularly formulated to advertise joint well being and alleviate joint pain. It is a singular combination of Ayurvedic herbs which have been used for centuries to improve joint operate and mobility. Let's dive deeper and understand what makes Rumalaya a go-to resolution for sustaining wholesome joints.
Precautions:
How Does Rumalaya Work?
In addition to this, Rumalaya has additionally proven promising leads to managing continual situations like osteoarthritis, rheumatoid arthritis, and spondylosis. The pure components in Rumalaya do not pose any opposed side effects and can safely be used for a chronic interval.
Multiple sclerosis can be classified as relapsing-remitting (the most common form) symptoms magnesium deficiency 60 pills rumalaya with mastercard, which is characterized by episodic neurologic symptoms with onset over hours to days and improvement over weeks to months, or primary progressive, which is characterized by progressive neurologic disability without relapses. Symptoms of multiple sclerosis include fatigue, depression, vision loss, double vision, stiffness or weakness, sensory loss and paresthesias, imbalance or incoordination, and bowel and bladder dysfunction with urgency and incontinence. Neurologic examination: A complete neurologic examination should be performed looking for abnormalities. Mental status: Cognitive testing may show impairments in all domains, but commonly executive function or attention. Sensory: Decreased sensation of pinprick, cold, proprioception, and vibration sensation. T2-weighted image in another patient shows small periventricular plaques (solid arrows) as well as an area of left parietal infarction (open arrow). Definition A brain abscess is a collection of infection/pus in the brain parenchyma. A brain abscess can develop due to direct spread of infection from a local infection. Less commonly, a brain abscess can develop from the hematogenous seeding of an infection from a distant site. The microorganism involved depends on the source of infection and is most commonly bacterial. Source of Infection Common Microorganisms Sinuses/dental Ears Head trauma/neurosurgical procedure Endocarditis lmmunocompromised host Streptococcus, Haemophilus, Bacteroides, Fusobacterium, and Prevote//a species Enterobacteriaceae, Pseudomonas aeruginosa, Streptococcus and Bacteroides species Staphylococcus aureus, P. Symptoms of a brain abscess are variable and include severe headache (75%) that is worse with lying flat, nausea, vomiting, drowsiness, weakness, numbness, and difficulty speaking. Other vital signs are generally normal, but if there is a systemic infection, hypotension and tachycardia may be present. Neurologic examination: No specific exam maneuvers exist for a brain abscess, but a complete neurologic examination should be performed to assess for abnormalities. Nuchal rigidity/meningismus (neck stiffness) may be present if there is rupture of the brain abscess into the ventricular system and/or coexisting meningitis. Motor/sensory/coordination: Any focal neurologic deficit may be present depending on the location of the abscess. Definition Meningitis is inflammation of the leptomeninges, which includes the dura, arachnoid, and pia mater that surround the brain and spinal cord. Meningitis is typically caused by infections and can be classified as bacterial meningitis (Table 7. Aseptic meningitis refers to meningitis in which routine bacterial cultures are negative. Aseptic meningitis may be caused by viral, fungal, and mycobacteria infections, as well as malignancy, inflammation, or drugs. Neck stiffness, headache, and fever: the differential diagnosis includes subdural/epidural empyema, brain abscess, and encephalitis. Common organisms causing meningitis Type of Infection Bacterial Microorganism Streptococcus pneumoniae, Neisseria meningitides, Haemophilus influenzae, Listeria monocytogenes (in neonates and elderly), S. Given the systemic infection, individuals may also have hypotension, tachycardia, and tachypnea. General inspection: Petechia and purpura may be present, particularly in cases of N. Special Tests Nuchal rigidity: Neck stiffness is detected with passive neck flexion (Sn 0. Kernig sign: With the patient supine and hip flexed to 90 degrees, the clinician attempts to fully extend the knees. The clinician flexes the leg at the hip and knee and then attempts to straighten the knee. Prior to the development of these symptoms, her primary care provider had diagnosed her with a viral upper respiratory tract infection. Rhinosinusitis is described by the sinuses involved (maxillary, ethmoid, frontal, or sphenoid sinuses), etiology (viral, bacterial, or fungal), presence of extrasinus involvement (complicated or uncomplicated), and aggravating factors. Furthermore, the clinical course of rhinosinusitis can be divided into five subtypes (Table 7. The majority of acute rhinosinusitis cases are caused by viral infection, specifically rhinovirus. Although rhinosinusitis occurs frequently in healthy patients, a number of local, regional, and systemic conditions may predispose a patient to developing rhinosinusitis (Table 7. Rhinitis and facial pain: the differential diagnosis includes allergic fungal rhinosinusitis, allergic rhinitis, invasive fungal rhinosinusitis, vasomotor rhinitis, trigeminal neuralgia, migraine or headache disorder, and temporomandibular joint dysfunction. Subtypes of rhinosinusitis Rhinosinusitis Task Force (2007) Clinical Classification Scheme Acute rhinosinusitis Recurrent rhinosinusitis Subacute rhinosinusitis Chronic rhinosinusitis Acute exacerbation of chronic rhinosinusitis Symptoms lasting <4 wk with complete resolution:2:4 episodes of acute rhinosinusitis per year with symptom-free intervals Symptoms lasting 4-12 wk Symptoms lasting:2:12 wk Sudden worsening of baseline chronic rhinosinusitis with return to baseline What symptoms might be observed Major symptoms of rhinosinusitis include congestion, facial pain/pressure, nasal obstruction, and purulent/colored nasal discharge. Minor symptoms include frontal headache, halitosis, dental pain, otalgia, and cough. Inspection: the anterior nasal mucosa may demonstrate edema, purulent discharge, and polyps. The oral cavity and oropharynx may demonstrate erythema from postnasal drip or poor dentition.
The septate uterus is the most common uterine anomaly in the general population as well as in women with recurrent pregnancy loss medicine and health purchase rumalaya 60 pills with visa. Women with uterine anomalies have higher rates of first- and second-trimester miscarriages compared to women with a normal uterus. The benefits of hysteroscopic septoplasty have not yet been assessed by a randomized trial. A transfundal metroplasty technique originally described by Strassmann may be the appropriate surgical procedure for unification in women with a bicornuate uterus who have a history of recurrent pregnancy loss or previable birth. Cervical cerclage may improve pregnancy outcomes in women with bicornuate uteri and in women with a unicornuate uterus or uterus didelphys who have a history of latetrimester pregnancy loss. Bider and coworkers reported that when cervical cerclage was used to treat women with a bicornuate uterus and recurrent pregnancy loss, the incidence of viable pregnancies markedly increased. In one series of 41 women with bicornuate uteri and recurrent abortion, 85% had a successful pregnancy outcome after cervical cerclage and the other 18 women had a term delivery following hysteroscopy (Bider, 1992). Sonographic measurements of cervical length help distinguish which patients may benefit from cerclage. Diethylstilbestrol can lead to uterine malformations, including hypoplastic cavity, T-shaped uterus, constriction bands, a wide lower segment, and irregular borders. The consequent lack of support of the fetal membranes leads to their prolapse and rupture, which is usually followed by expulsion of the fetus and placenta. The incidence of this problem was previously estimated to vary from 1 in 57 to 1 in 1730 pregnancies. It is believed that most cases occur as a result of surgical trauma to the cervix from conization, loop electrosurgical excision procedures, mechanical dilation of the cervix during pregnancy termination, or obstetric lacerations. Cytogenetic analysis of miscarriages from couples with recurrent miscarriage: a case control study. A review by Grimbizis and colleagues found a high rate of miscarriage in women with septate (n = 499, 44. Several imaging modalities may be used to evaluate the uterus, including hysterosalpingogram, transvaginal ultrasonography, and sonohysterography. Hysteroscopic septoplasty is the treatment of choice for women with a septate uterus and a history of pregnancy loss, with laparotomy reserved for exceptional and complicated anomalies. March and Israel initially reported that it was possible to incise the septum, even those thicker than 1 cm, of all of the 82 women with recurrent abortion studied, using the hysteroscope. Cervical incompetence rarely causes recurrent miscarriage, as it is treated after the first occurrence of loss. The diagnosis is usually made by obtaining a history of second-trimester pregnancy loss without contractions or labor and in the absence of other clear etiology. Many times the patient will have mild contractions shortly before expelling the pregnancy or before an examination that finds the cervical dilatation to be advanced. Commonly, the cervix is noted to be unexpectedly dilated at the time of a mid-trimester ultrasound. Ultrasound diagnosis of cervical shortening has been shown to be a marker of preterm birth rather than cervical insufficiency. Women who are found to have cervical dilation either from digital or speculum exam at less than 24 weeks of gestation are candidates for examination-indicated cerclage, known as emergency or rescue cerclage. The benefit of a rescue cerclage in these women has only been demonstrated from one small randomized trial and retrospective studies. Cerclage placement consists of a concentric nonabsorbable suture as close to the level of the internal os as possible. However, if the criteria for diagnosis are less certain, in several randomized clinical trials, there is only a slight increase in the incidence of term deliveries after cerclage is performed. An ultrasound examination should be performed before the cerclage is placed to document that a normal gestation is present. Occasionally, if there is a markedly shortened cervix or placement of a cerclage has failed to maintain the pregnancy, a transabdominal cerclage may be performed. If the suture is buried as in the Shirodkar procedure, then elective cesarean delivery at or beyond 39 weeks of gestation may be considered. Large arrow to small area denotes canal from external os to internal os, respectively. Leiomyomas that distort the uterine cavity, including submucosal or intramural with an intracavitary component, may result in decreased pregnancy and implantation rates as well increased risk of miscarriage. Although a causal relationship is difficult to establish, studies have shown a significant reduction in miscarriage rates following an abdominal myomectomy. In a major review published in 1981, Buttram and Reiter reported that when abdominal myomectomy was performed in a total of 1941 women, the rate of spontaneous abortion was reduced from 41% to 19% (Buttram, 1981). A more recent, smaller study by Marchionni and colleagues showed that miscarriage rates decreased from 69% to 25% postmyomectomy (Marchionni, 2004). These data indicate that fibroids are associated with miscarriage, particularly those that distort the uterine cavity, and that a myomectomy may confer reproductive benefits. Subserosal fibroids, with greater than 50% of their mass outside the myometrium are unlikely to cause adverse pregnancy outcomes. Recurrent miscarriage is a more acceptable indication for myomectomy than a single loss. Uterine polyps are a rare cause of miscarriage based on observational studies and are found and treated hysteroscopically. This view was seen on transabdominal scan (small arrows, internal os; large arrow, external os).
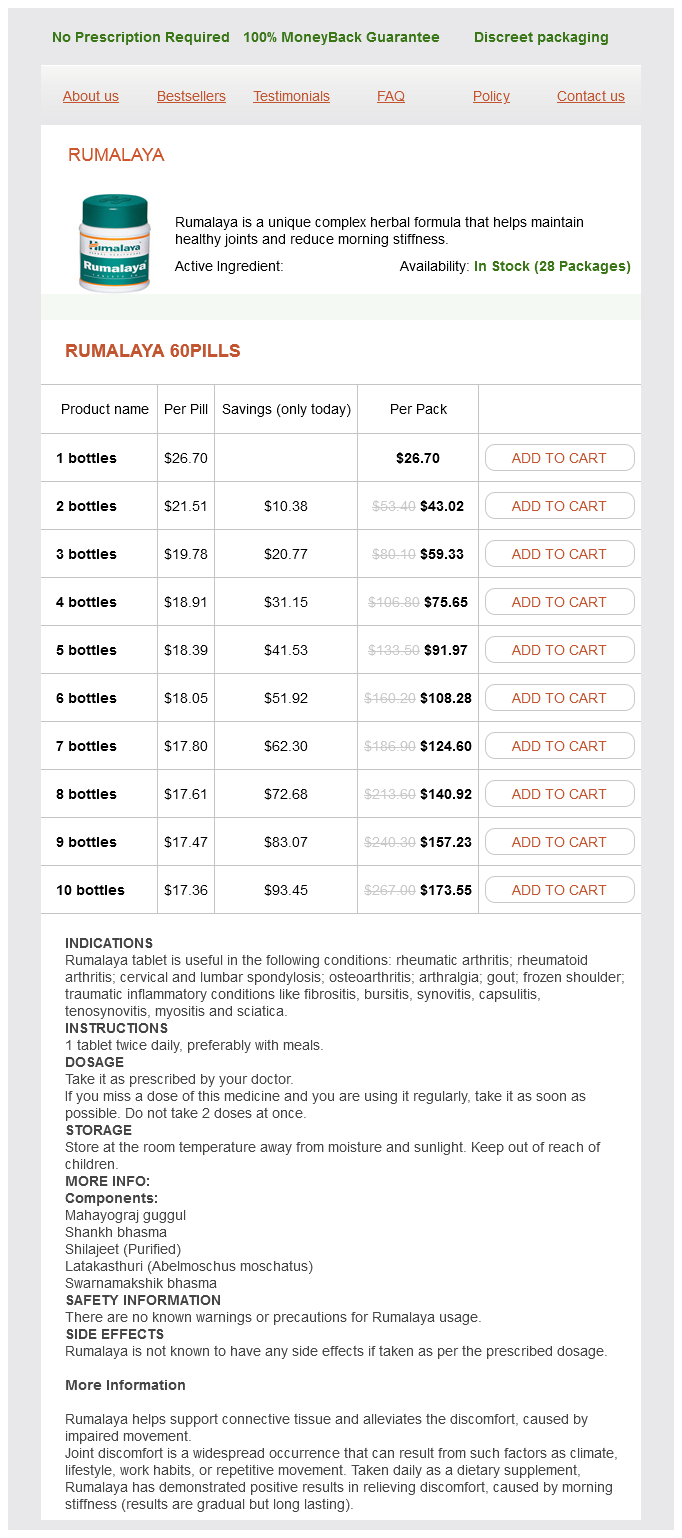
Rumalaya Dosage and Price
Rumalaya 60pills
- 1 bottles - $26.70
- 2 bottles - $43.02
- 3 bottles - $59.33
- 4 bottles - $75.65
- 5 bottles - $91.97
- 6 bottles - $108.28
- 7 bottles - $124.60
- 8 bottles - $140.92
- 9 bottles - $157.23
- 10 bottles - $173.55
Risk factors can be stratified into (1) major factors that increase relative risk greater than two times normal and (2) minor factors (see Table 15 medications you cant drink alcohol discount rumalaya 60 pills visa. Additionally, within the latter group a very high-risk group is identified for purposes of prophylactic options (Table 15. Women of average risk have a personal risk of about 12% of developing breast cancer, the risk of the general population. In the moderate risk group, women have personal risks from 12% to 15% of developing breast malignancy during their lifetime and have one or more minor risk factors. The risk of developing breast carcinoma is consistent with a linear dose-response relationship. Other historical Very high risk >20% Obstetrics & Gynecology Books Full 15 Breast Diseases in the moderate risk category do not need any changes from those of the general population in screening recommendations. Women at high risk include those who have greater than a 15% personal risk of developing breast cancer, usually from a major risk factor. The model was developed in white women, taking into account age, race, age of menarche, number of births, number of first-degree relatives with breast cancer, and number of breast biopsies that have shown atypia. It is not applicable to women with more than two first-degree relatives with breast cancer and does not consider more distant relatives, the age at which relatives developed breast cancer, or a family history of ovarian cancer. It is not useful for women with a strong family history of breast cancer on the paternal side. The Clauss model, developed by Elizabeth Clauss in 1994, uses data from the Cancer and Steroid Hormone Study. This model uses first- and second-degree relatives, both maternal and paternal, to calculate risk but does not use risk factors beyond family history and also is not as robust in nonwhites. The Clauss model provides the lifetime risks for a woman over any given decade of her life. Reasons for referral to a genetic counselor for hereditary cancer risk evaluation include patients with a female breast cancer diagnosed at a young age (<50 years), a triple-negative receptor tumor, two or more synchronous primary breast cancers, male breast cancer, or invasive ovarian/fallopian tube/primary peritoneal cancer. Pre-andpostgenetic counseling is essential and includes discussing the issues and implications of the results, legal and insurance aspects, noninformative results, and choices for chemoprevention or surgical prophylaxis. The benefits of screening have been emphasized by major health societies and professional organizations (Table 15. The updated recommendations are as follows: (1) routine screening of average-risk women should begin at age 50, (2) routine screening should end at age 74, (3) women should get screening mammograms every 2 years, and (4) recommend against teaching breast selfexamination. These recommendations were based on evidence that shows the value of mammography increases with age, with women ages 50 to 74 benefiting the most. In this age group screening is most beneficial and has the least amount of harm when performed every 2 years. The updated recommendations are as follows: (1) regular screening mammography starting at age 45 years, (2) annual screening Box 15. Preventive Services Task Force, 2015 None stated None stated Screening recommended to age 74 y Evidence insufficient for age 75 y 1 y for all ages 1 y for all ages 2 y for age 50-74 y Table 15. Four trials compared tamoxifen with placebo, two trials compared raloxifene with placebo, and one trial compared raloxifene with tamoxifen. Theoccurrence of breast cancer is rare before age 20 years and uncommon before age 30 years. For women who are high risk, endocrine therapy should be discussed to reduce the risk of invasive or in situ breast cancers. Selection criteria in identifying women who would benefit from endocrine therapy include age >60 years, age over 35 years with a history of lobular carcinoma in situ, ductal carcinoma in situ or atypical proliferative lesion of the breast (atypical ductal or lobular hyperplasia), women 35 to 59 years with a Gail model risk of breast cancer 1. Tamoxifen and raloxifene, both selective estrogen receptor modulators, are proved options that can decrease the risk of breast cancer in high-risk women (Table 15. The trial was closed prematurely because of a large discordance between the two groups. Tamoxifen significantly reduced the incidence of breast cancer in this population of patients by 49% compared with controls (P <. Although treatment with tamoxifen compared with placebo is associated with an increased incidence in thromboembolic events and an increased incidence of endometrial cancer, the overall incidence of adverse events is small. A reduced incidence of thromboembolic events and endometrial cancer was noted in the raloxifene group compared with tamoxifen. In an 81-month median follow-up analysis, long-term raloxifene retained 76% of the effectiveness of tamoxifen in preventing invasive disease and grew closer over time to tamoxifen in preventing noninvasive disease. Less toxicity in regard to the development of endometrial cancer, uterine hyperplasia, and thromboembolic events was observed in the raloxifene group. However,musculoskeletalsideeffects,vaginaldryness, and vasomotor symptoms were significantly greater in the anastrozole group. Though these medications are effective, many women do not want to take them because of the side effects related to premature or perimenopausal symptoms. In a retrospective cohort of 639 patients, Hartmann was able to demonstrate a 90% breast cancer risk reduction for the patient with a high risk of breast cancer after prophylactic bilateral mastectomy. Although prophylactic bilateral mastectomy provides the greatest risk reduction, it is usually reserved for the very high-risk patient because of the associated physiologic and complicated psychological consequences. Although most women who have undergone prophylactic bilateral mastectomy do not regret having undergone the procedure, approximately 5% to 20% report dissatisfaction. However, a significant number are also noted during patient or clinician breast examination, and up to 15% of women are diagnosed with breast cancer not detected on mammography. Breast cancer is usually asymptomatic prior to the development of locally advanced disease. Approximately 10% of women with early breast carcinoma experience breast pain that is associated; however, focal mastalgia is usually associated with a benign condition.