Secnidazole
General Information about Secnidazole
Secnidazole is an antimicrobial bactericide that belongs to the nitroimidazole class of drugs. It is a synthetic by-product of metronidazole, another generally used antibiotic. Secnidazole has a broad range of makes use of, particularly in the remedy of bacterial and protozoal infections.
In addition to intestinal amoebiasis, secnidazole can be generally used in the treatment of liver amoebiasis. This much less common type of amoebic an infection is caused by the same protozoan species however impacts the liver instead of the intestines. Secnidazole, together with other drugs, is commonly used to eradicate the parasite from the liver and forestall further injury.
One of the principle makes use of of secnidazole is in the therapy of urogenital infections such as urethritis and vaginitis. These conditions are attributable to micro organism or protozoa infecting the urinary or reproductive tracts. Secnidazole works by inhibiting the growth and spread of these microorganisms, in the end resulting in their elimination and the decision of signs.
It is crucial to take secnidazole as prescribed for the total period of treatment, even if signs enhance. This ensures complete eradication of the infection and helps stop the event of antibiotic resistance. It is also necessary to notice that secnidazole does not defend in opposition to sexually transmitted infections, and extra measures ought to be taken to forestall their unfold.
In conclusion, secnidazole is an efficient antimicrobial bactericide that is extensively used within the therapy of various bacterial and protozoal infections. It offers a broad spectrum of exercise and is well-tolerated by most sufferers. However, it is essential to use this medicine as directed and full the complete course of therapy to make sure successful recovery. As with any treatment, individuals ought to seek the guidance of their healthcare supplier before beginning secnidazole therapy.
Another situation that secnidazole is prescribed for is giardiasis, a common diarrheal sickness attributable to the protozoan Giardia lamblia. This an infection can be prevalent in areas with poor sanitation and could be simply transmitted via contaminated water or meals. Secnidazole is an efficient remedy choice for giardiasis, because it targets and eliminates the parasite from the digestive tract.
Intestinal amoebiasis, also called amoebic dysentery, is one other situation for which secnidazole is regularly prescribed. This infection is brought on by the protozoan species Entamoeba histolytica and is common in creating nations with poor sanitation. Secnidazole has shown to be highly efficient in treating intestinal amoebiasis, as it targets and kills the parasite liable for the infection.
One of the important thing benefits of using secnidazole is its high efficacy in opposition to a number of types of micro organism and protozoa. This makes it a versatile antibiotic and a very good alternative for treating various infections. Secnidazole also has a longer half-life in comparison with different antibiotics, that means that it remains within the physique for an extended period, allowing for less frequent dosing.
Secnidazole is generally well-tolerated, with few reported unwanted effects. Common side effects embrace nausea, vomiting, and complications. However, these are typically mild and resolve on their very own. In some uncommon instances, extra extreme side effects such as allergic reactions may happen, and patients ought to search medical attention if these happen.
However treatment bacterial vaginosis purchase secnidazole 500 mg free shipping, further studies are important to assess factors underlying its therapeutic effect. Subsequently, in 2014, Deer and coworkers2 reported on a further consensus statement on the clinical use of neuromodulation in chronic pain based on theoretical background, clinical data, and side effect of each method. Some studies have shown that 75% to 100% of patients with trigeminal neuropathic pain have excellent pain relief. Studies have reported promising results in small groups of patients with cluster headaches. Three patients had improvement of more than 90%, three of them had moderate improvement (40%-60%), and four patients had mild improvement (20%-30%). Interestingly, the combination of occipital and supraorbital neurostimulation in an uncontrolled series of 7 patients with chronic migraine produced a headache frequency improvement greater than 90% in all patients, but there was no significant response to either stimulation alone. In the three main trials treating a range of 13 to 15 patients, the success rate was slightly more than 60%. Their first review dealt with the pathophysiology, relative anatomy, theoretical mechanisms, and history of neurostimulation; and the second review focused on central stimulation and contained an overall analysis of efficacy, safety, cost, patient selection, and suggestions for further study based on available evidence. The investigators concluded that peripheral neurostimulation techniques carry an advantage over central neuromodulation. Percutaneous hybrid paddle leads, peripheral nerve field stimulation, nerve root stimulation, dorsal root ganglion, and high-frequency stimulation are actively being refined to address axial low back pain and foot pain. Although all medicine based on science has some degree of empirical support, evidence-based medicine goes further, classifying evidence by its epistemologic strength and requiring that only the strongest evidence (coming from metaanalyses, systemic reviews, and randomized controlled trials) can yield strong recommendations; weaker evidence (such as from case-control studies) can yield only weak recommendations. Evidence quality can be assessed according to the source type as well as other factors, including statistical validity, clinical relevance, currency, and peer-reviewed acceptance. Evidence-based medicine categorizes different types of clinical evidence and rates or grades them according to the strength of their freedom from the various biases that beset medical research. Several organizations have developed grading systems for assessing the quality of evidence. Dramatic results in uncontrolled trials might also be regarded as this type of evidence. As a result, effectively no level I studies have been performed on these procedures. Taking into account the studies on neurostimulation as a treatment for pain, we can conclude that there are data and studies supporting the use of neurostimulation as a treatment method in special cases of pain but that further studies are needed to support an epistemologic and clear conclusion concerning the efficacy and importance of neurostimulation as a treatment method for pain. The appropriate use of neurostimulation: stimulation of the intracranial and extracranial space and head for chronic pain. The appropriate use of neurostimulation of the spinal cord and peripheral nervous system for the treatment of chronic pain and ischemic diseases: the neuromodulation appropriateness consensus committee. A multicenter, prospective trial to assess the safety and performance of the spinal modulation dorsal root ganglion neurostimulator system in the treatment of chronic pain. Neuromodulation of chronic headaches: position statement from the European Headache Federation. The appropriate use of neurostimulation: avoidance and treatment of complications of neurostimulation therapies for the treatment of chronic pain. The appropriate use of neurostimulation: new and evolving neurostimulation therapies and applicable treatment for chronic pain and selected disease states. The appropriate use of neurostimulation of the spinal cord and peripheral nervous system for the treatment of chronic pain and ischemic diseases: the Neuromodulation Appropriateness Consensus Committee. Intermittent stimulation of nucleus ventralis posterolateralis for intractable pain. Chronic self-stimulation of the medial posterior inferior thalamus for the alleviation of deafferentation pain. Long Term Results of Intermittent Stimulation of the Sensory Thalamic Nuclei in 67 Cases of Deafferent Pain. Clinical results and physiological basis of thalamic relay nucleus stimulation for relief of intractable pain with morphine tolerance. Pain relief by electrical stimulation of the central gray matter in humans and its reversal by naloxone. Tryptophan loading may reverse tolerance to opiate analgesics in humans: a preliminary report. Stimulation of human periaqueductal gray for pain relief increases immunoreactive beta-endorphin in ventricular fluid. Enkephalin-like material elevated in ventricular cerebrospinal fluid of pain patients after analgetic focal stimulation. Alterations of immunoreactive beta-endorphin in the third ventricular fluid in response to electrical stimulation of the human periaqueductal gray matter. Initial and long-term results of deep brain stimulation for chronic intractable pain. Analgesia produced by stimulation of various sites in the human beta-endorphin system. Deep brain and motor cortex stimulation for poststroke movement disorders andpoststroke pain. Deep brain stimulation for control of intractable pain in humans, present and future: a ten-year follow-up. Treatment of chronic pain by deep brain stimulation: long term follow-up and review of the literature. Comparative Study of Electrical Stimulation of Posterior Thalamic Nuclei, Periaqueductal Gray and Other Midline Mesencephalic Structures in Man.
More severe injury involves the brainstem in addition to the structures mentioned earlier and is called a "global" pattern of injury with a grave prognosis medicine 6 year secnidazole 500mg low cost. Infants with watershed injury, especially if not associated with basal ganglia injury, have a more favorable outcome. Both whole-body cooling and selective head cooling resulted in reduction in the risk of death or major neurodevelopmental disability. Common side effects identified in clinical studies include sinus bradycardia, mild hypotension requiring inotropic support, and mild thrombocytopenia. Advances in newborn medicine and marked improvements in the survival of very preterm and highrisk infants, however, have resulted in a host of neurological injuries associated with prematurity, multiparity, and extremely low birth weight. Moreover, many infants who suffer neonatal brain injuries now survive through adulthood, frequently with residual cognitive or functional disability and/or conditions requiring long-term neurosurgical care. This chapter considers neonatal brain injuries in three broad etiologic categories: hypoxic/ischemic, hemorrhagic, and traumatic, each of which is important to neurosurgeons either in the acute treatment of the injuries themselves or in the long-term management of survivors of these injuries. Ten percent to 40% of affected infants do not survive, and nearly 1 in 3 exhibit long-term neurodevelopmental delay. In severe cases, there is an initial phase of primary neuronal death due to exhaustion of cellular metabolites and an influx of sodium and water with resultant cell death. This initial phase of "primary energy failure" is followed by a latent period that varies from 6 to 12 hours when the metabolic milieu normalizes. Clinically, the secondary energy failure phase is associated with worsening encephalopathy and onset of electrographic seizures. The clinical syndrome of neonatal encephalopathy is defined by American College of Obstetricians and Gynecologists5 as "disturbed neurologic function in the earliest days of life in an infant born at or beyond 35 weeks of gestation, manifested by a subnormal level of consciousness or seizures, and often accompanied by difficulty with initiating and maintaining respiration and depression of tone and reflexes. Seizures in the immediate newborn period do not typically manifest as the classic generalized tonic-clonic activity seen in older children and adults, largely owing to incomplete myelination of the corticospinal tract and a higher threshold for secondary generalization. Levetiracetam is increasingly being used as a second-line drug in the treatment of neonatal seizures, although its efficacy has yet to be tested in a phase 3 clinical trial. The recognition of neonatal seizures in the preterm population has only lately been reported. The presence of seizures has also been associated with a lower language score at 2 years, even after adjustment of data for family social risk. Of all early neonatal deaths not related to congenital malformations, 28% are due to preterm birth. The overall cost burden in the United States alone was estimated on the order of $26. Preterm births in the United States peaked in 2007 and have since been on a slow decline; however, the rate remains high, with a rate of 11. Overall, children who required shunts were more likely to have cerebral palsy, neurodevelopmental impairment, and lower mental and psychomotor development indices than those without shunts. The germinal matrix is most prominent along the thalamostriate groove at or just posterior to the foramen of Monro, and it is the most common site for hemorrhage. Active cell proliferation occurs within the germinal matrix, producing neuroblast and glial progenitor cells, which form the overlying cortex and white matter. A progressive involution of the germinal matrix occurs until the late preterm period, from an average of 2. First, the matrix is richly vascularized by arterial branches from the internal carotid, anterior cerebral, and middle cerebral arteries. The recurrent artery of Huebner, the anterior choroidal artery, and perforating lenticulostriate arteries are particularly important, contributing to a capillary bed within the germinal matrix that is composed of primitive endotheliumlined vessels without surrounding connective tissue. These proliferative, immature vessels are friable and, owing to still-developing cerebral autoregulation, are vulnerable to systemic variations in cerebral blood flow and pressures, and thus may hemorrhage. When hemorrhage does occur, the site of origin appears to be along the primitive capillary-like vessels of the matrix or along the capillary-venule junction, and not from arterioles. It has been shown that the hemorrhage follows the distribution of fan-shaped medullary veins that funnel into bilateral terminal veins, which then run through the germinal matrix. The terminal veins then empty into the internal cerebral veins and the vein of Galen. Therefore, it is generally thought that the necrosis associated with germinal matrix hemorrhage is actually a venous infarction due to obstruction of the medullary and terminal veins. Postnatally, muscle paralysis with pancuronium has been investigated in infants being mechanically ventilated for respiratory distress syndrome; in infants who had spontaneous breathing asynchronous with the ventilator, paralysis seemed to have had a beneficial effect. However, this effect was not borne out when pancuronium was used routinely in all ventilated infants. It is generally recommended that all preterm infants weighing less than 1500 g undergo cranial ultrasound examination within the first 48 hours of life. A, T1-weighted axial image showing high signal in the thalamus, putamen, and globus pallidus. Other signs and symptoms typically associated with hydrocephalus, including, lethargy, vomiting, and impaired upgaze ("setting sun" sign), may be absent or difficult to appreciate in these critically ill infants. At present, there remains a dearth of evidence-based information to inform treatment decisions, and there is wide variation in clinical practice. A, A small area of cystic encephalomalacia (arrow), likely the result of a previous grade I germinal matrix hemorrhage, in the left caudate nucleus. D, Ventricular dilation due to intraventricular hemorrhage (not fully visible in this section). E, Subsequent decompression after placement of a right-sided ventricular reservoir.
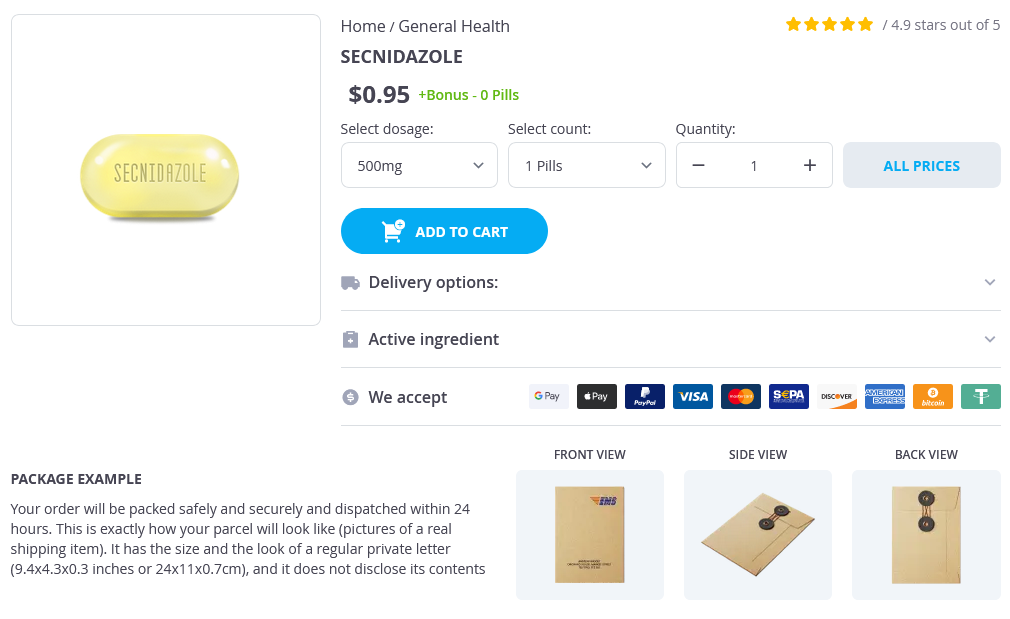
Secnidazole Dosage and Price
Secnidazole 500mg
- 1 pills - $1.05
Secnidazole 1gr
- 12 pills - $40.95
- 24 pills - $64.95
- 36 pills - $78.95
- 60 pills - $111.95
- 120 pills - $155.95
As new technology becomes available medicine river 500mg secnidazole overnight delivery, the contribution to outcome of poorly characterized physiologic variables, such as autoregulation of cerebral blood flow, will be better understood. New strategies to optimize patient management through implementation of evidence-based best clinical practices will pave the way for future clinical trials of pharmacological neuroprotective and rehabilitation interventions. Resuscitation of blood pressure and oxygenation and prehospital brain-specific therapies for the severe pediatric traumatic brain injury patient. Brain injuries and neurological system failure are the most common proximate causes of death in children admitted to a pediatric intensive care unit. Variation in intracranial pressure monitoring and outcomes in pediatric traumatic brain injury. Craniocervical arterial dissection in children: clinical and radiographic presentation and outcome. Pediatric neurocritical care: a neurology consultation model and implication for education and training. Emerging subspecialties in neurology: building a career and a field: pediatric neurocritical care. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Effect of implementation of a paediatric neurocritical care programme on outcomes after severe traumatic brain injury: a retrospective cohort study. Multimodal monitoring in traumatic brain injury: current status and future directions. Brain tissue oxygen monitoring after severe traumatic brain injury in children: relationship to outcome and association with other clinical parameters. Transcranial Doppler-based assessment of cerebral autoregulation in critically ill children during diabetic ketoacidosis treatment. Cerebral hyperemia measured with near infrared spectroscopy during treatment of diabetic ketoacidosis in children. The epidemiology of vasospasm in children with moderate-to-severe traumatic brain injury. Optic nerve sheath diameter as a marker for evaluation and prognostication of intracranial pressure in Indian patients: an observational study. Tissue oxygen index: thresholds for cerebral ischemia using near-infrared spectroscopy. Acute care clinical indicators associated with discharge outcomes in children with severe traumatic brain injury. Incidence of hypo- and hypercarbia in severe traumatic brain injury before and after 2003 pediatric guidelines. Cerebrovascular response in infants and young children following severe traumatic brain injury: a preliminary report. Part 1: relation to age, Glasgow coma score, outcome, intracranial pressure, and time after injury. Childhood arterial ischaemic stroke incidence, presenting features, and risk factors: a prospective population-based study. Intelligence after stroke in childhood: review of the literature and suggestions for future research. Neurologic outcome in survivors of childhood arterial ischemic stroke and sinovenous thrombosis. Report of the National Institute of Neurological Disorders and Stroke workshop on perinatal and childhood stroke. A multispecialty pediatric neurovascular conference: a model for interdisciplinary management of complex disease. Use of alteplase in childhood arterial ischaemic stroke: a multicentre, observational, cohort study. Maternal and infant characteristics associated with perinatal arterial stroke in the infant. Stroke in children: the coexistence of multiple risk factors predicts poor outcome. Prospective assessment of risk factors for recurrent stroke during childhood-a 5-year follow-up study. Arteriopathy diagnosis in childhood arterial ischemic stroke: results of the vascular effects of infection in pediatric stroke study. Arterial ischemic stroke in neonates, infants and children: an overview of underlying conditions, imaging methods, and treatment modalities. Risk of recurrent childhood arterial ischemic stroke in a population-based cohort: the importance of cerbrovascular imaging. Ischaemic stroke from dissection of the craniocervical arteries in childhood: report of 12 patients. Prognosis of occlusive disease of the circle of Willis (moyamoya disease) in children. Lipoprotein (a) and genetic polymorphisms of clotting factor V, prothrombin, and methylenetetrahydrofolate reductase are risk factors of spontaneous ischemic stroke in childhood. Outcome following decompressive craniectomy for malignant middle cerebral artery infarction in children. Cerebral venous sinus thrombosis in children: risk factors, presentation, diagnosis and outcome. Cerebral venous sinus thrombosis presenting with excessive subarachnoid hemorrhage in a 14-yearold boy.