Sildenafila
General Information about Sildenafila
Erectile dysfunction is a typical problem that impacts hundreds of thousands of males worldwide. It can have a significant impression on a person’s high quality of life, inflicting emotions of disgrace, embarrassment, and relationship issues. The most typical explanation for ED is decreased blood circulate to the penis, which could be as a outcome of bodily elements such as diabetes, high blood pressure, heart disease, or psychological elements corresponding to stress, despair, or nervousness.
Sildenafil belongs to a category of medication known as phosphodiesterase sort 5 (PDE5) inhibitors. It works by enjoyable the muscular tissues and growing the blood move to the penis, which helps to supply and preserve an erection. This mechanism of motion makes it an effective treatment for ED, the lack to get and keep an erection agency sufficient for sexual intercourse.
Since its approval, sildenafil has turn into the go-to remedy for ED in men. It is on the market in various doses (25mg, 50mg, and 100mg) and is usually taken about an hour earlier than sexual activity. The results of sildenafil can last up to four hours, permitting males to have a satisfying sexual experience. However, it is important to observe that the drug doesn't work with out sexual stimulation.
Sildenafil was first found by Pfizer scientists within the 1980s and was initially developed as a therapy for high blood pressure and angina, a kind of chest ache. However, during clinical trials, researchers observed that the drug had an unexpected side effect – it improved erectile operate in males. In 1998, the US Food and Drug Administration (FDA) accredited sildenafil for the therapy of ED, making it the first oral treatment for this situation.
While sildenafil has proven to be an effective therapy for ED and PAH, it is not with out its side effects. The most typical side effects embrace headache, flushing, indigestion, and stuffy or runny nostril. In rare circumstances, extra severe unwanted aspect effects similar to sudden vision or hearing loss, chest pain, or an erection lasting longer than four hours may occur. Therefore, it is important to consult a physician earlier than taking sildenafil, particularly in case you have underlying medical situations or are taking other drugs.
In conclusion, sildenafil, also identified as Viagra, is a extensively used medicine for treating erectile dysfunction and pulmonary arterial hypertension. Its discovery and approval have modified the lives of hundreds of thousands of males, permitting them to regain their sexual confidence and enhance their overall quality of life. However, like several medication, it is important to take it as prescribed, and if any side effects happen, seek the guidance of a physician instantly.
Apart from its main use for ED, sildenafil additionally performs a task within the treatment of PAH. PAH is a uncommon condition by which the blood vessels within the lungs turn out to be narrowed, making it tough for the center to pump blood by way of them. As a end result, the center has to work tougher, which can result in fatigue, shortness of breath, and chest pain. Sildenafil works by relaxing the blood vessels in the lungs, allowing for improved blood flow and lowering the workload on the heart.
Sildenafil, also called Viagra, is a drugs that has been widely used for treating erectile dysfunction (ED) in males. It can be used to deal with pulmonary arterial hypertension (PAH), a situation by which the blood stress within the arteries that supply the lungs becomes abnormally excessive.
The role of macronutrients in obesity has been examined in a variety of populations impotence blood pressure cheap sildenafila 100 mg visa, but the results of 1. The storage capacity for protein and carbohydrate is limited and converting these nutrients to a more readily stored form requires energy expenditure. Whey protein ingestion in elderly results in greater muscle protein accrual than ingestion of its constituent essential amino acid content. A high proportion of leucine is required for optimal stimulation of the rate of muscle protein synthesis by essential amino acids in the elderly. Diets with high or low protein content and glycemic index for weight-loss maintenance. Weight and metabolic outcomes after 2 years on a lowcarbohydrate versus low-fat diet: a randomized trial. Comparison of high protein and high fiber weight-loss diets in women with risk factors for the metabolic syndrome: a randomized trial. Obese patients have inadequate protein intake related to protein intolerance up to 1 year following Roux-en-Y gastric bypass. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. Endocrine and nutritional management of the post-bariatric surgery patient: an Endocrine Society Clinical Practice Guideline Clinical Practice Guideline. Consensus statement Academy of Nutrition and Dietetics and American Society for Parenteral and Enteral Nutrition: characteristics recommended for the identification and documentation of adult malnutrition. Carbohydrate-induced hypertriacylglycerolemia: historical perspective and review of biological mechanisms. Use of the glycemic index for weight loss and glycemic control: a review of recent evidence. Since protein intake stimulates the largest rise in energy expenditure due to the metabolic cost of protein synthesis, gluconeogenesis, and ureogenesis, a highprotein diet has the greatest thermic effect. The amount of protein in the diet was a stronger predictor of weight loss success than the glycemic index of carbohydrates consumed. Veldhorst M, Smeets A, Soenen S, Hochstenbach-Waelen A, Hursel R, Diepvens K, et al. Effect of dietary protein content on weight gain, energy expenditure, and body composition during overeating. Rates of urea production and hydrolysis and Leucine oxidation change linearly over widely varying protein intakes in healthy adults. In: Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids. The digestion rate of protein is an independent regulating factor of postprandial protein retention. Slow and fast dietary proteins differently modulate postprandial protein accretion. Failure to increase lipid oxidation in response to increasing dietary fat content in formerly obese women. Effects of isoenergetic, lowfat diets on energy metabolism in lean and obese women. Effects of gastric bypass and gastric banding on glucose kinetics and gut hormone release. Comparison of the dietary intake and clinical characteristics of obese and normal weight adults. Identification, Assessment, and Treatment of Vitamin and Mineral Deficiencies After Bariatric Surgery Margaret M. Identify and understand potential vitamin/mineral deficiencies seen among preoperative bariatric surgery patients, as well as most common deficiencies s/p weight loss surgery. Recognize appropriate laboratory analyses to assess for vitamin and mineral deficiencies after bariatric surgery. Describe guidelines for effective treatment of vitamin and mineral deficiencies after weight loss surgery. Although it is commonly known that bariatric surgery patients may be at risk for particular vitamin/mineral deficiencies associated with surgery, it may not be as clear that there are possible micronutrient deficiencies evidenced prior to surgery that bear mentioning. An overview of micronutrients most at risk after bariatric surgery is provided, as well as guidelines for the assessment and treatment of common vitamin/mineral deficiencies seen postoperatively. Introduction Although much remains to be established regarding the prevalence and etiology of vitamin and mineral deficiencies after bariatric surgery, this chapter serves as a guideline for the identification, assessment, and treatment of potential vitamin/mineral deficiencies after commonly performed bariatric surgery procedures. It included suggestions for preoperative and postoperative nutrition screening, assessment, and treatment of the bariatric patient, including vitamin and mineral deficiencies commonly seen after these procedures. In a subsample of 89 subjects, additional laboratory tests were performed, which included thiamin, niacin, vitamin A, vitamin E, selenium, and copper levels. Thiamin, copper, and vitamin A deficiencies were not demonstrated among these subjects [2]. Furtado authors strongly recommended a systematic assessment of the micronutrient status in all candidates for bariatric surgery. Vitamins and minerals serve as essential cofactors in a number of biological processes that may affect body weight regulation, including appetite, metabolic rate, nutrient absorption, thyroid and adrenal gland function, energy storage, glucose homeostasis, and neural activities [1]. Therefore, vitamin/mineral repletion and adherence is imperative for successful long-term weight management. The majority of B-complex vitamins, significant for proper metabolism of carbohydrates and integral in normal neural functions that regulate appetite, have been determined to be deficient among some preoperative patients with severe obesity [3]. These include iron deficiencies, which may diminish energy use and have been reported in approximately 50 % of preoperative bariatric patients with severe obesity. Additionally, zinc and selenium deficiencies have been reported, as well as suboptimal levels of vitamins A, C, and E all imperative for regulation of energy production and many other processes in the body related to body weight regulation [35].
Unfortunately impotence for males discount 100 mg sildenafila with amex, the literature is only beginning to identify the parent and family characteristics of the obesogenic family environment and specifically that of the adolescent with extreme obesity considering or undergoing bariatric surgery. Further, mothers who reported their own psychological distress were more likely to have obese adolescents who reported greater depressive symptoms [16]. Thus, the family environment may be characterized not only by a shared disease (obesity) but potentially dysfunction. Two studies to date have examined family factors in the context of adolescent bariatric surgery [3, 11]. While direct comparisons of these findings prove difficult due to use of different assessment tools, both suggest that the degree of general family dysfunction is variable and certainly not universal for the adolescent patient. For example, Sysko and colleagues [11] utilized presurgery psychiatric evaluation data and found that for a small group of adolescents presenting with high levels of psychopathology. In contrast, a second study [3] found limited family or caregiver dysfunction at the time of surgery and no detectable change in these family factors across the initial 12 months following surgery. Thus, as the adolescent undergoes significant change in weight and psychosocial health, the family appears to remain stable. Remarkably absent in the adolescent bariatric literature are assessment tools that would allow the characterization of more "condition-specific" family factors that may impact bariatric surgery outcomes, be they physical or psychosocial. The adult literature has demonstrated a strong family history for extreme obesity among adult family members [42, 43]. At the same time, a recent study suggested that bariatric surgery may render an additional benefit. Future research needs to explore whether bariatric surgery will emerge as a family weight loss tool and whether having a caregiver who has also undergone bariatric surgery presents unique benefits and/or challenges for the adolescent patient. High-Risk Contexts Childhood Trauma Increasing evidence suggests an association between childhood trauma, including child abuse and neglect, and the development of obesity [4547]. Noll and colleagues presented the first evidence for the prospective longitudinal association of childhood sexual abuse with the subsequent development of obesity by young adulthood [45]. Retrospective reports of childhood sexual abuse history from adult bariatric candidates have ranged from 16 % [48] to 69 % [49]. To date, there have been no studies that have addressed the impact of childhood trauma on the psychosocial functioning of obese youth or the prevalence of childhood trauma in adolescents who undergo bariatric surgery. The broader developmental literature suggests there are several psychosocial impairments that are both sequelae of childhood trauma and correlates of childhood and adolescent obesity. Further, high-risk behaviors such as substance abuse and dependence, delinquency, and highrisk sexual behaviors have also been cited as short- and longterm sequelae of childhood trauma [52, 53]. Thus, the consequences of abuse may amplify or exacerbate the psychosocial risks associated with extreme obesity and be negatively related to the level of psychosocial improvement that follows bariatric surgery. Socioeconomic Status Socioeconomic status, at the family or even neighborhood level, has great potential to negatively affect adolescent health. Childhood obesity has been linked to a number of related family socioeconomic factors, including lower family household income, single-parent status, lower parental education, poor living conditions, and lack of neighborhood safety [54]. However, these types of associations have not been assessed or are less consistent for obese adolescents [55, 56]. The range of socioeconomic status of youth presenting for laparoscopic gastric banding at one institution suggests variability, with a reported median family income of approximately $49,000, with 14. Reiter-Purtill High-Risk Behaviors Adolescence is a developmental period characterized by an increased willingness to engage in behaviors considered to be risky, harmful, or even antisocial. Alcohol, tobacco, and illicit drug use are often initiated during this time period, as is sexual activity. Adolescence is also a developmental period known for increased risk for the first onset of nonfatal suicidal behaviors. While arguably the initiations of such behaviors are seen as "normative," these behaviors are not always benign. For example, adolescence/emerging adulthood is also a period of risk for progression to abusing or becoming dependent on substances [58, 59] or acquiring a sexually transmitted infection [60, 61]. Until quite recently, prevalence rates of these high-risk behaviors in extremely obese adolescents were unknown. Specifically, these national data suggested that while adolescent girls with extreme obesity were less likely than healthy weight girls to have had sexual intercourse, if they had, it was more likely to have happened under the influence of alcohol or drugs, a known context of increasing risk. Also, extreme adolescent obesity was associated with greater likelihood of smoking, and for boys, initiation of smoking before the age of 13, a known predictor of increased risk of tobacco dependence. These national data suggest that relative to healthy weight youth who accurately perceived their weight, adolescents at any level of excess weight who also accurately perceived themselves as "overweight" had greater odds of engaging in suicidal ideation, whereas if inaccurate, had no greater odds. Findings regarding actual nonfatal suicide attempts were less straightforward and varied based on actual weight/weight perception accuracy and race/ethnicity. To fully understand the impact of bariatric surgery on the psychosocial health outcomes of adolescents, the frequency of their engagement in such high-risk behaviors must be considered. Furthermore, in light of an emerging adult bariatric literature examining links between bariatric surgery and alcohol use/abuse or other addictive behaviors, as well as associations with increased risk of death by suicide, understanding the high-risk behaviors of the adolescent patient becomes increasingly paramount. From a developmental perspective, evidence of psychosocial health impairments without effective intervention places an adolescent who carries their obesity burden forward at risk for continued poor psychosocial health and development as they transition to adulthood. Certainly the available adult obesity literature leads us to predict an otherwise bleak picture of health and well-being. Initial adolescent bariatric psychosocial outcome data indicating improvements in multiple domains are impressive, although as previously mentioned are limited to single-site studies of small sample size, with follow-up extending to only the 24-month time-point.
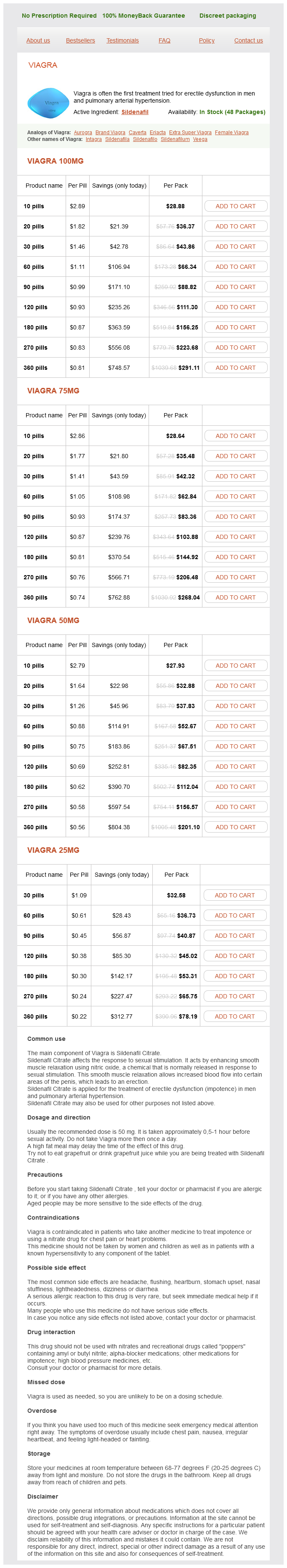
Sildenafila Dosage and Price
Viagra 100mg
- 10 pills - $28.88
- 20 pills - $36.37
- 30 pills - $43.86
- 60 pills - $66.34
- 90 pills - $88.82
- 120 pills - $111.30
- 180 pills - $156.25
- 270 pills - $223.68
- 360 pills - $291.11
Viagra 75mg
- 10 pills - $28.64
- 20 pills - $35.48
- 30 pills - $42.32
- 60 pills - $62.84
- 90 pills - $83.36
- 120 pills - $103.88
- 180 pills - $144.92
- 270 pills - $206.48
- 360 pills - $268.04
Viagra 50mg
- 10 pills - $27.93
- 20 pills - $32.88
- 30 pills - $37.83
- 60 pills - $52.67
- 90 pills - $67.51
- 120 pills - $82.35
- 180 pills - $112.04
- 270 pills - $156.57
- 360 pills - $201.10
Viagra 25mg
- 30 pills - $32.58
- 60 pills - $36.73
- 90 pills - $40.87
- 120 pills - $45.02
- 180 pills - $53.31
- 270 pills - $65.75
- 360 pills - $78.19
In order to reduce liver size prior to surgery impotence at 46 buy cheap sildenafila 75 mg on line, a short-term, 710 days, liquid diet is often prescribed. Fris demonstrated a highly significant reduction in liver size in patients consuming a 2-week, low-energy liquid diet prior to bariatric surgery [7]. In diabetic individuals for whom you are prescribing preoperative low-energy-density liquid diets, adjustments in their insulin requirements and oral hypoglycemic medications may be necessary to prevent hypoglycemia. In addition, medications, anesthesia, postoperative dehydration, and increased protein consumption can further precipitate that risk. Preoperative Colonic Preparations By and large, routine preoperative colon cleansing is not indicated nor warranted. This chronic constipation is further exacerbated by anesthesia, narcotics for pain control, and postoperative high-protein liquid diets. These patients can develop a megacolon-like picture with colonic distention and significant fecal impaction. A regular bowel regimen with isotonic polyethylene glycol solution may be beneficial prior to surgery and postoperatively as needed [9]. Preoperative Pulmonary Training Postoperative atelectasis in the bariatric surgery patient is common and can lead to pneumonic processes and hypoxemia. Anesthesia, pain causing splinting, and somnolence can all exacerbate this process. Early aggressive pulmonary toilet, mobilization, and lung expansion maneuvers are critical to maintain normal respiratory function and decrease postoperative pulmonary complications [13]. However, pain, somnolence from anesthesia, and inadequate pain control can interfere with proper teaching of incentive spirometry Preoperative Medication Adjustments Although there is a paucity of level 1 evidence of preoperative medication adjustments prior to bariatric surgery, best practice outcomes have recommended various medication adjustments or cessation prior to surgery. To alleviate this, providing the patient with an incentive spirometer device with instruction at the surgical history and physical outpatient visit can allow the patient to familiarize themselves with the device and provide inspiratory muscle training prior to surgery. In summary, obstructive sleep apnea is a common comorbid medical problem in the bariatric surgery population. Many of these patients require noninvasive positive pressure devices for varying severities of obstructive sleep apnea. In the postoperative period, hypoventilation and hypoxemia with hypercarbia are not uncommon due to residual influence of general anesthesia, postoperative atelectasis, postoperative analgesia, and pain. As weight loss ensues, patients often complain of ill-fitting masks and pressure settings too powerful. For the bariatric surgery patient specifically, there are no concrete recommendations. A reasonable recommendation would be to continue prescribed beta blockers, anti-reflux medications, thyroid replacements, arrhythmic medication, psychiatric medications, and inhalers, which should be safe to be taken the morning of surgery. Depending on the surgical start time, holding or modifying the dose of antidiabetic medications may be warranted. Intraoperatively From a medical standpoint, an important factor influencing postoperative morbidity and length of stay is perioperative glycemic control. Obese diabetics, and even obese nondiabetics, require higher insulin requirements than expected. Anesthesiologists and surgeons are understandably cautious about treating hyperglycemia in patients with or without a diagnosis of diabetes using standardized protocols due to ensuing adverse hypoglycemic effect. Continuous insulin infusion protocols are available for a wide variety of patients with varying degrees of insulin infusions. Early ambulation is critical for thromboembolic prevention and should be encouraged the night of the surgery. If the patient is unable to get out of bed and ambulate that evening, sitting up over the side of the bed for a bedside dangle is beneficial in preventing venostasis. Not surprisingly, significant improvement was seen in arterial hypertension with less hypoxemia, hypercapnia, and improvement in spirometry. Of the 30 patients requiring noninvasive ventilation devices, all but four patients had their devices withdrawn. Since patients have varying degrees of obstructive sleep apnea and the rate of weight loss differs between patients, no clear-cut timeframe from surgery or specific weight loss thresholds should negate the need for a follow-up polysomnogram on average of 710 months postoperatively. Although there are recommendations for prolonged thromboprophylaxis in major abdominal, pelvic, orthopaedic, and trauma patients [2022] the important question, which has not been well studied to date, is the duration of thromboprophylaxis following bariatric surgery. Postoperative Medication Administration Considerations After Bariatric Surgery Following bariatric surgery, proper medication adjustments are crucial to adequately dose patients without under- or overdosing based on their new altered anatomy. Which surgical procedure is performed will dictate how much, if any, medication adjustment is required. A purely restrictive procedure, like the adjustable gastric band, may not require any medication adjustment, whereas Roux-en-Y gastric bypass or duodenal switch procedures, based on their altered anatomy, do require administration considerations following bariatric surgery. This is due to nearly all oral agents being maximally absorbed in the small intestine, which is bypassed in several bariatric procedures. Delayed gastric emptying, diminished opportunity for mucosal exposure, and changes in drug dissolution and solubility resulting from alterations in intestinal pH are additional factors that may potentially impair drug absorption [25]. Despite the growing number of bariatric surgeries being performed in the United States, with Roux-en-Y gastric bypass being the most frequently performed, there is a paucity of pharmacokinetic studies of drug absorption following bariatric surgery. Inherently, with the altered anatomy following bariatric surgery, reduced and augmented absorption is not surprising. Reasonable contraindications include known medication allergy or adverse reaction, heparin-induced thrombocytopenia, coagulation disturbance, the presence of active bleeding, or clinic concern for high risk of bleeding. With greater than 90 % of all bariatric surgeries performed laparoscopically, improved clinical pathways, and 18 the Perioperative and Postoperative Medical Management of the Bariatric Surgery Patient 179 Diabetic Medications Bariatric surgery, specifically the Roux-en-Y gastric bypass, has shown to be safe and effective treatment for patients suffering from type 2 diabetes. Continued administration of pre-op diabetic medication without adjustment usually results in unwarranted hypoglycemia.