Slip Inn
General Information about Slip Inn
Slip Inn is generally well-tolerated and has minimal unwanted effects. However, some individuals could expertise gentle side effects corresponding to headaches, dizziness, and upset abdomen. These unwanted side effects are uncommon and often subside over time.
Valerian root additionally has a similar chemical structure to benzodiazepines, which are generally prescribed for sleep problems. However, in contrast to prescription treatment, valerian root doesn't cause drowsiness or dizziness the following day, making it a preferred alternative for lots of.
It is important to notice that Slip Inn just isn't recommended for pregnant or breastfeeding women, kids, or these with liver disease. If you are presently taking any treatment, it is best to seek the guidance of with your healthcare provider earlier than including Slip Inn to your routine.
Moreover, Slip Inn is a pure supplement, making it a safer possibility than prescription medicine, which can have undesirable side effects. It additionally doesn't trigger dependence or tolerance, meaning it may be used long-term with out the chance of dependancy.
One of the main benefits of Slip Inn is its capacity to improve sleep quality. Studies have shown that valerian root can increase the period of sleep and cut back the variety of instances a person wakes up in the course of the night. This makes it an effective therapy for insomnia and different sleep issues.
Valerian root has been extensively studied for its results on sleep and has been proven to significantly enhance sleep quality. It incorporates compounds that act on the mind and nervous system, selling relaxation and inducing sleep. These compounds increase the degrees of gamma-aminobutyric acid (GABA) in the brain, a neurotransmitter that helps to calm the mind and reduce anxiousness.
Slip Inn can additionally be a handy possibility for many who have hassle falling asleep. Its compact measurement and ease of use make it suitable for on-the-go use, making it a perfect selection for frequent travelers.
Slip Inn works by enhancing the production of GABA in the mind, which helps to loosen up the physique and calm the thoughts, making it easier to go to sleep. It additionally increases the levels of serotonin, a hormone that regulates mood and promotes a way of well-being. This might help to reduce nervousness and melancholy, which are widespread causes of sleep disturbances.
Slip Inn is a pure sleep assist that makes use of the facility of valerian root to advertise relaxation and enhance sleep quality. It is a protected and effective various to prescription medicine for these fighting sleep disorders. With its natural components and handy kind, Slip Inn may be the key to getting a restful night time's sleep. However, it is necessary to talk to your doctor earlier than starting any new complement to ensure it's safe for you to use.
Slip Inn is a sleep assist complement that contains a potent extract of valerian root. This plant is native to Europe and Asia and has been used in traditional medicine for its sedative and tranquilizing results. The supplement is out there in pill or liquid type and is commonly used as a pure different to prescription medication for sleep.
In addition, Slip Inn additionally accommodates different pure components similar to magnesium and chamomile, which have been proven to have a relaxing impact on the physique and promote sleep. These elements work collectively to supply a synergistic impact, making Slip Inn a robust sleep aid.
Slip Inn is a well-liked natural complement that has gained attention for its use as a pure sleep assist. Its primary ingredient, valerian, has been used for tons of of years as a remedy for sleep disorders and anxiousness. In this article, we will discover the benefits of Slip Inn and how it works to enhance sleep quality.
Such patients require emergent chemotherapy with adjunctive leukapheresis as mortality approaches 40% in the first 48 hours rumi herbals pvt ltd purchase generic slip inn on-line. On examination, patients appear pale and have purpura and petechiae; signs of infection may not be present. Stomatitis and gum hypertrophy may be seen in patients with monocytic leukemia, as may rectal fissures. The first step in treatment is to obtain complete remission, defined as normal peripheral blood with resolution of cytopenias, normal bone marrow with no excess blasts, and normal clinical status. This therapy will produce complete remissions in 8090% of patients under age 60 years and in 5060% of older patients (see Table 394). Patients with a favorable genetic profile can be treated with chemotherapy alone or with autologous transplant with cure rates of 6080%. Patients who do not enter remission (primary induction failure) or those with high-risk genetics have cure rates of less than 10% with chemotherapy alone and are referred for allogeneic stem cell transplantation. Patients over age 60 have had a poor prognosis, even in first remission, when treated with standard chemotherapy approaches, and only 1020% become long-term survivors. The use of reduced-intensity allogeneic transplant has improved the outcome for such patients, with studies suggesting that up to 40% of selected patients may be cured. Patients should also receive central nervous system prophylaxis so that meningeal sequestration of leukemic cells does not develop. After achieving complete remission, patients may be treated with either additional cycles of chemotherapy or high-dose chemotherapy and stem cell transplantation. Adults younger than 39 years have uniformly better outcomes when treated under pediatric protocols. Intermediate-risk patients have a 3050% chance of cure with chemotherapy, and high-risk patients are rarely cured with chemotherapy alone. High-risk patients with adverse cytogenetics or poor responses to chemotherapy are best treated with allogeneic transplantation. Minimal residual disease testing early on can also identify high-risk patients who will not be cured with chemotherapy alone. For patients with relapsed disease, the bispecific antibody blinatumomab has shown remarkable response rates as a bridge to es kerrs oo k eb oo e//eb /t. Reducedintensity allogeneic transplantation is increasingly being utilized in order to improve on these outcomes. Patients with adverse cytogenetics, poor response to chemotherapy, or older age have a much lower chance of cure (cure rates of 2040%). The disease is usually indolent, with slowly progressive accumulation of long-lived small lymphocytes. Hypogammaglobulinemia is present in 50% of patients and becomes more common with advanced disease. Immunodeficiency is also related to inadequate antibody production by the abnormal B cells. Other lymphoproliferative diseases such as Waldenström macroglobulinemia, hairy cell leukemia, or lymphoma (especially mantle cell) in the leukemic phase are distinguished on the basis of the morphology and immunophenotype of circulating lymphocytes and bone marrow. On examination, 80% of patients will have lymphadenopathy and 50% will have enlargement of the liver or spleen. The morphology of the latter is different, characterized by larger and more immature cells. In approximately 5% of cases, while the systemic disease remains stable, an isolated lymph node transforms into an aggressive large-cell lymphoma (Richter syndrome). The white blood cell count is usually greater than 20,000/mcL (20 × 109/L) and may be markedly elevated to several hundred thousand. Lymphocytes appear small and mature, with condensed nuclear chromatin, and are morphologically indistinguishable from normal small lymphocytes, but smaller numbers of larger and activated lymphocytes may be seen. Indications for treatment include progressive fatigue, symptomatic lymphadenopathy, anemia, or thrombocytopenia. The latter combination is better tolerated and associated with fewer adverse events but results in a shorter time to progression (see Table 3911). The Bruton tyrosine kinase inhibitor ibrutinib is a well-tolerated, oral agent given at 420 mg daily; it has shown remarkable activity and duration of response in the front-line setting and is another option for those patients who wish to avoid chemotherapy. For older patients or young patients with significant comorbidities, chlorambucil, 0. However, ibrutinib has become the standard of care in the United States for these patients. The novel monoclonal antibody obinutuzumab, in combination with chlorambucil, produces a significant number of responses (75%) including elimination of disease at the molecular level (in 17%) and offers another well-tolerated choice in this patient population. Both of these agents can be associated with marked lymphocytosis due to release of tumor cells from the lymph nodes into the peripheral blood. This results in a significant early reduction in lymphadenopathy but a potentially misleading, more delayed clearance of peripheral blood and bone marrow. There are risks for colitis, liver injury, and fatal infectious complications in patients treated with idelalisib. Patients should be given antimicrobial prophylaxis and monitored closely while taking idelalisib. In patients with deletion of chromosome 17p, treatment with ibrutinib can result in a sustained duration of response (85% at 2 years), a breakthrough in this disease. However, it can be associated with tumor lysis and neutropenia, and patients may require hospitalization for initial therapy. Associated autoimmune hemolytic anemia or immune thrombocytopenia may require treatment with rituximab, prednisone, or splenectomy.
Prospective evaluation of the diagnostic accuracy of hepatic copper content himalaya herbals 100 tabletas order slip inn 1pack with amex, as determined using the entire core of a liver biopsy sample. Symptoms and Signs the presentation is most commonly subacute but may be fulminant, acute, or chronic. Clinical manifestations generally include tender, painful hepatic enlargement, jaundice, splenomegaly, and ascites. With chronic disease, bleeding varices and hepatic encephalopathy may be evident; hepatopulmonary syndrome may occur. Imaging studies show occlusion/absence of flow in the hepatic vein(s) or inferior vena cava. Clinical picture is similar in sinusoidal obstruction syndrome but major hepatic veins are patent. The screening test of choice is contrast-enhanced, color, or pulsed-Doppler ultrasonography, which has a sensitivity of 85% for detecting evidence of hepatic venous or inferior vena caval thrombosis. Direct venography can delineate caval webs and occluded hepatic veins ("spider-web" pattern) most precisely. The risk of hepatocellular carcinoma is increased; risk factors include cirrhosis, combined hepatic vein and inferior vena cava obstruction, and a longsegment interior vena cava block. Liver biopsy is often contraindicated in sinusoidal obstruction syndrome because of thrombocytopenia, and the diagnosis is based on clinical findings. Prompt recognition and treatment of an underlying hematologic disorder may avoid the need for surgery; however, the optimal anticoagulation regimen is uncertain, and anticoagulation is associated with a high risk of bleeding, particularly in patients with portal hypertension and those undergoing invasive procedures. Low-molecularweight heparins are preferred over unfractionated heparin because of a high rate of heparin-induced thrombocytopenia with the latter. Infusion of a thrombolytic agent into recently occluded veins has been attempted with success. The drug is given as an intravenous infusion every 6 hours for a minimum of 21 days. Serious adverse effects include hypotension and hemorrhage, and the drug is expensive. Balloon angioplasty, in some cases with placement of an intravascular metallic stent, is preferred in patients with an inferior vena caval web and is being performed increasingly in patients with a short segment of thrombosis in the hepatic vein. Patients with Budd-Chiari syndrome often require lifelong anticoagulation and treatment of the underlying myeloproliferative disease; antiplatelet therapy with aspirin and hydroxyurea has been suggested as an alternative to warfarin in patients with a myeloproliferative disorder. For all patients with Budd-Chiari syndrome, a poor outcome has been reported to correlate with Child-Pugh class C and a lack of response to interventional therapy of any kind. Incidence and risk factors of hepatocellular carcinoma in patients with hepatic venous outflow tract obstruction. In some cases, the precipitating event is arterial hypoxemia due to respiratory failure, sleep apnea, severe anemia, heat stroke, carbon monoxide poisoning, cocaine use, or bacterial endocarditis. Elevations of serum alkaline phosphatase and bilirubin are usually mild, but jaundice is associated with worse outcomes. The prothrombin time may be prolonged, and encephalopathy or hepatopulmonary syndrome may develop. The mortality rate due to the underlying disease is high (particularly in patients receiving vasopressor therapy or with septic shock, acute kidney disease, or coagulopathy), but in patients who recover, the aminotransferase levels return to normal quickly, usually within 1 week-in contrast to viral hepatitis. Serum alkaline phosphatase levels are normal or slightly elevated, and aminotransferase levels are only mildly elevated in the absence of superimposed ischemia. Hepatojugular reflux is present, and with tricuspid regurgitation the liver may be pulsatile. Ascites may be out of proportion to peripheral edema, with a high serum ascites-albumin gradient (greater than or equal to 1. The incidence and outcomes of ischemic hepatitis: a systematic review with meta-analysis. Pylephlebitis (septic thrombophlebitis of the portal vein) may complicate intra-abdominal inflammatory disorders such as appendicitis or diverticulitis, particularly when anaerobic organisms (especially Bacteroides species) are involved. Nodular regenerative hyperplasia results from altered hepatic perfusion and can be associated with collagen vascular diseases; myeloproliferative disorders; and drugs, including azathioprine, 5-fluorouracil, and oxaliplatin. The term "obliterative portal venopathy" is used to describe primary occlusion of intrahepatic portal veins in the absence of cirrhosis, inflammation, or hepatic neoplasia. Aside from splenomegaly, the physical findings are not remarkable, although hepatic decompensation can follow severe gastrointestinal bleeding or a concurrent hepatic disorder, and intestinal infarction may occur when portal vein thrombosis is associated with mesenteric venous thrombosis. Covert hepatic encephalopathy is reported to be common in patients with noncirrhotic portal vein thrombosis. Idiopathic noncirrhotic portal hypertension is common in India and has been attributed to chronic infections, exposure to medications or toxins, prothrombotic disorders, immunologic disorders, and genetic disorders that result in obliterative vascular lesions in the liver. It is rare in Western countries, where increased mortality is attributable to associated disorders and older age. Portal vein thrombosis may occur in 1025% of patients with cirrhosis, is associated with the severity of the liver disease, and may be associated with hepatocellular carcinoma but not with increased mortality. Other risk factors are oral contraceptive use, pregnancy, chronic inflammatory diseases (including pancreatitis), injury to the portal venous system (including surgery), other malignancies, and treatment of thrombocytopenia with eltrombopag. Portal vein thrombosis may be classified as type 1, involving the main portal vein; type 2, involving one (2a) or both (2b) branches of the portal vein; or type 3, involving the trunk and branches of the portal vein. Laboratory Findings Liver biochemical test levels are usually normal, but there may be findings of hypersplenism. It is possible, however, that in many cases evidence of hypercoagulability is a secondary phenomenon due to portosystemic shunting and reduced hepatic blood flow. The liver can be invaded by bacteria via (1) the bile duct (acute "suppurative" [formerly ascending] cholangitis); (2) the portal vein (pylephlebitis); (3) the hepatic artery, secondary to bacteremia; (4) direct extension from an infectious process; and (5) traumatic implantation of bacteria through the abdominal wall. Predisposing conditions and factors include presence of malignancy, diabetes mellitus, inflammatory bowel disease, and cirrhosis; necessity for liver transplantation; and use of proton pump inhibitors. Pyogenic liver abscess has been observed to be associated with a subsequent increased risk of gastrointestinal malignancy.
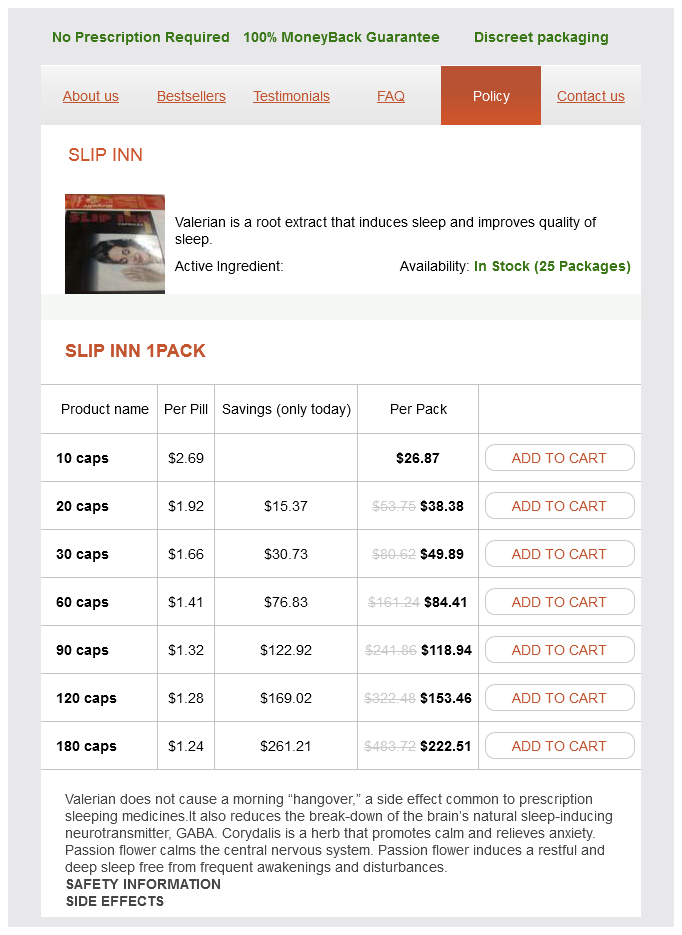
Slip Inn Dosage and Price
Slip Inn 1pack
- 10 caps - $26.87
- 20 caps - $38.38
- 30 caps - $49.89
- 60 caps - $84.41
- 90 caps - $118.94
- 120 caps - $153.46
- 180 caps - $222.51
Placement of an inferior vena cava filter is also recommended for recurrent thromboembolism despite adequate anticoagulation herbs list order genuine slip inn, for chronic recurrent embolism with a compromised pulmonary vascular bed (eg, in pulmonary hypertension), and with the concurrent performance of surgical pulmonary embolectomy or pulmonary thromboendarterectomy. Percutaneous transjugular placement of a mechanical filter is the preferred mode of inferior vena cava interruption. In rare critically ill patients for whom thrombolytic therapy is contraindicated or unsuccessful, mechanical or surgical extraction of thrombus may be indicated. Pulmonary embolectomy is an emergency procedure of last resort with a very high mortality rate. These statistics highlight the importance of preventive therapy in high-risk patients (Chapter 14). Death from recurrent thromboemboli is uncommon, occurring in less than 3% of cases. Chronic thromboembolic pulmonary hypertension develops in approximately 1% of patients. Predictive value of computed tomography in acute pulmonary embolism: systematic review and meta-analysis. Evaluation of patients with suspected acute pulmonary embolism: best practice advice from the Clinical Guidelines Committee of the American College of Physicians. Normal pulmonary artery systolic pressure at rest is 1530 mm Hg, with a mean pressure between 10 mm Hg and 18 mm Hg. The pulmonary circulation is a lowpressure, low-resistance system due to its large crosssectional area, and it can accommodate significant increase in blood flow during exercise. The primary pathologic mechanism in pulmonary hypertension is an increase in pulmonary vascular resistance that leads to an increase in the pulmonary systolic pressure greater than 30 mm Hg or the mean pressure greater than 20 mm Hg. The World Health Organization currently classifies pulmonary hypertension based on similarities in pathologic mechanisms and includes the following five groups. Group 1 (pulmonary arterial hypertension secondary to various disorders): this group gathers diseases that localize directly to the pulmonary arteries leading to structural changes, smooth muscle hypertrophy, and endothelial dysfunction. Group 2 (pulmonary venous hypertension secondary to left heart disease): Often referred to as pulmonary venous hypertension or "post-capillary" pulmonary hypertension, this group includes left ventricular systolic or diastolic dysfunction and valvular heart disease. Group 4 (pulmonary hypertension secondary to chronic thromboembolism): this group consists of patients with pulmonary hypertension due to thromboembolic occlusion of the proximal and distal pulmonary arteries. Narrow splitting of second heart sound with loud pulmonary component; findings of right ventricular hypertrophy and heart failure in advanced disease. Electrocardiographic evidence of right ventricular strain or hypertrophy and right atrial enlargement. Elevated right ventricular systolic pressure on two-dimensional echocardiography with Doppler flow studies. Patients in whom pulmonary hypertension is suspected should undergo echocardiography with Doppler flow. The echocardiogram is useful in the assessment of underlying cardiac disease while Doppler flow can estimate the right ventricular systolic pressure. Right ventricular systolic pressure can be estimated based on tricuspid jet velocity and right atrial pressure. The severity of pulmonary hypertension can also be assessed based on the right ventricular size and function. Right-sided cardiac catheterization remains the gold standard for the diagnosis and quantification of pulmonary hypertension and should be performed prior to initiation of advanced therapies. Estimated pressures on echocardiogram correlate with right heart catheterization measurement but can vary by at least 10 mm Hg in more than 50% of cases so should not be used to direct therapy. Cardiac catheterization is particularly helpful in differentiating pulmonary arterial hypertension from pulmonary venous hypertension by assessment of the drop in pressure across the pulmonary circulation, also known as the transpulmonary gradient. Vasodilator challenge is often performed during right heart catheterization and for a significant acute vasodilator response consists of a drop in mean pulmonary pressure of greater than 10 mm Hg (or 20%) to less than 40 mm Hg. V /Q lung scanning is a very sensitive test that can differentiate chronic thromboembolic pulmonary hypertension from idiopathic pulmonary arterial hypertension. Currently, pulmonary angiography is considered the most definitive diagnostic procedure for defining the distribution and extent of disease in chronic thromboembolic pulmonary hypertension. No symptoms at rest but ordinary physical activity causes dyspnea, fatigue, chest pain, or near syncope. No symptoms at rest but less than ordinary activity causes dyspnea, fatigue, chest pain, or near syncope. Syncope occurs with exertion when there is insufficient cardiac output or if there is an arrhythmia. Hemoptysis is a rare but life-threatening event in pulmonary hypertension usually caused by the rupture of a pulmonary artery. Findings on physical examination can include jugular venous distention, accentuated pulmonary valve component of the second heart sound, right-sided third heart sound, tricuspid regurgitation murmur, hepatomegaly, and lower extremity edema. Cyanosis can occur in patients with an open patent foramen ovale and right-to-left shunt due to increased right atrial pressure. Laboratory Findings errs es ook b ook b Routine blood work is often normal; any abnormalities noted are usually related to the underlying disease in secondary pulmonary hypertension. On arterial blood gas analysis, patients with idiopathic pulmonary arterial hypertension often have normal Pao2 at rest but show evidence of hyperventilation with a decrease in Paco2. Currently, there are no primary therapies available targeting the underlying lesion for patients in Group 1 (pulmonary arterial hypertension) but advanced therapies are available directly targeting the pulmonary hypertension itself.