Speman
General Information about Speman
Speman may be taken as a tablet, capsule, or syrup, relying on personal preference. The recommended dosage is one tablet or capsule twice every day, or as directed by a healthcare skilled. The syrup may be taken in a dose of 5ml twice daily.
Speman is an ayurvedic natural supplement that's primarily used to deal with male infertility. It incorporates a mixture of potent herbs and minerals that work collectively to enhance the standard and amount of sperm in men. The supplement is produced by the renowned Himalaya Drug Company, which is well known for its pure and protected merchandise.
Improves sperm depend and quality: The natural components in Speman have been known to boost sperm count, motility, and morphology. Studies have proven that men who took Speman for 6 months skilled a major improve in sperm rely and a greater high quality of sperm.
The herbal elements in Speman have aphrodisiac properties that help enhance libido, sexual health, and fertility. The complement also has anti-inflammatory and antioxidant properties, which can defend sperm from damage attributable to free radicals. It also nourishes the reproductive organs, making them more healthy and more environment friendly in producing and storing sperm.
Reduces irritation: The anti-inflammatory properties of Speman can help scale back inflammation in the reproductive organs, which may enhance the general well being of the male reproductive system.
It is crucial to seek the guidance of a well being care provider before taking Speman, particularly if you are on any treatment or have a pre-existing medical condition. The complement just isn't appropriate for pregnant or lactating ladies and ought to be averted by children.
Increases libido and sexual efficiency: Speman contains aphrodisiac properties that can enhance sexual desire and performance. It helps increase testosterone levels, which play an important role in male sexual health.
In conclusion, Speman is an all-natural natural complement with numerous benefits for male reproductive well being. It helps improve sperm count, motility, and high quality, and can also enhance libido and sexual efficiency. Additionally, it's protected and free of unwanted effects, making it a popular selection for males fighting fertility points. However, it is important to consult a healthcare professional before beginning any new supplement to ensure it is suitable for you.
Enhances antioxidant defense: Free radicals can harm sperm and have an result on their high quality and motility. The antioxidant properties of Speman can help protect sperm from oxidative stress, enhancing their possibilities of fertilization.
Speman is an herbal complement that has gained popularity for its potential to promote spermatogenesis – the process of sperm production. It is a novel blend of pure herbs and minerals that have been utilized in Ayurvedic drugs for hundreds of years to improve male reproductive health. This article will delve into the benefits of Speman and how it works to spice up sperm manufacturing.
Speman primarily works by stimulating the testes to produce wholesome and viable sperm. It additionally enhances the features of the seminal vesicles and epididymis, that are answerable for storing and transporting sperm.
Speman is formulated using 44 totally different pure components corresponding to Ashwagandha, Kokilaksha, Vanya Kahu, and Gokshura, amongst others. Each ingredient in Speman has its distinctive benefits and works synergistically to extend sperm manufacturing and motility.
Safe and pure: One of the significant advantages of Speman is that it is created from pure herbs and minerals, making it secure for consumption and free of unwanted side effects.
It is during this period that the blood-air barrier is established and specialized cells of the respiratory epithelium appear prostate cancer quality of life order 60 pills speman with visa. During early fetal development the entire gut tube is suspended by the dorsal mesentery. The dorsal mesentery extends from the lower oesophagus to the cloaca but is lost over the duodenum, ascending colon, and descending colon, probably as a result of subsequent gut rotation. The liver develops within the ventral mesentery while the spleen arises from the dorsal mesogastrium. The pancreas develops from the endodermal lining of the duodenum starting as two pancreatic buds, the dorsal and ventral buds, which begin to arise from week 4 of intra-uterine life. The hepatic diverticulum arises above the pancreatic duct from the ventral wall of the duodenum. Prior to this the red blood cells contain a nucleus and are produced by the mesoblast. Through fetal development the midgut rapidly elongates and outgrows the small volume of the peritoneal cavity. The herniation is reduced at 10 weeks of intra-uterine life when the volume of the peritoneal cavity is bigger than the length of the midgut. Initially the hindgut opens into the primitive cloaca, the precursor to the bladder (urogenital sinus), and the rectum (hindgut). It is primarily involved in nutrition and excretion, collection of liquid waste from the embryo, and the exchange of gases in the embryos of birds, reptiles, and some mammals. In human embryos the allantois is comparatively small and involved with early blood formation and with the formation of the urinary bladder. The allantois is initially continuous with the bladder, but as the bladder enlarges with further development and division of the urogenital sinus and the hindgut by the urorectal septum, the allantois constricts and becomes a thick, fibrous cord called the urachus, represented in the adult as the median umbilical ligament. The anal canal is derived from two embryological tissues demarcated by the pectinate line. Thus, the upper two-thirds are lined with columnar epithelium and derive their blood supply from the superior rectal artery (which is a branch of the inferior mesenteric artery). The lower third, however, is lined with stratified squamous epithelium and derives its blood supply from the inferior rectal artery (which is a branch of the internal pudendal artery). The lumen of the anal canal is initially occluded at 7 weeks of intra-uterine life and recanalized at 9 weeks. Urinary system the initial structures that develop in the urogenital system have an excretory function. This figure was published in Gray, Anatomy of the Human Body, Twentieth edition, throughly revised and re-edited by Warren H. The ureteric bud is an outgrowth of the mesonephric duct and begins to develop from week 5 of intra-uterine life. Transverse sections showing successive stages in the development of a mesonephric tubule between the fifth and eleventh weeks. The vesicle soon becomes an S-shaped mesonephric tubule and extends laterally to join the pronephric duct, now renamed the mesonephric duct. The development of the female internal genitalia occurs in the absence of testosterone and anti-Mullerian hormone. The mesonephric duct is responsible for the formation of the: ductus deferens epididymis seminal vesicles the paramesonephric ducts are also known as the Mullerian ducts. Regression of these ducts is due to the secretion of anti-Mullerian hormone in the male fetus. The ducts lie lateral to the mesonephric ducts and form the: fallopian tubes broad ligament uterovaginal canal. The uterovaginal canal gives rise to the uterus, cervix, and upper half of the vagina. It eventually fuses with the sinovaginal bulb, which is the swelling on the urogenital sinus that forms the lower half of the vagina and the vaginal plate. The abdominal opening of intestine lower part, represented by a dotted line the left uterine tube descending to the prostatic utricle, ls. Epoophoron indicates the direction in which the testis which either the ovary or and epididymis descend from the abdomen sc. Scattered remains of constituting the organ of Giraldès, or the Wolffian tubes near it (paroöphoron paradidymis of Waldeyer of Waldeyer) the external genitalia are undifferentiated until 9 weeks of intra-uterine life. The genital tubercle elongates to form the clitoris in the female fetus and gives rise to the penis in the male fetus. Later in intrauterine life they differentiate into the male (testis) and female (ovary) sex organs. Trophoblastic differentiation gives rise to the cytotrophoblast and syntiotrophoblast. The chorionic villi increase the surface area available for gaseous and substrate exchange with the maternal blood. Fibrinoid deposition occurs in the placenta from as early as 4 months of gestation. Chapter 1 General Embryology the ovary is formed by the gonadal ridge and mesonephros. The first phase is an independent phase that occurs until the testes reach the deep inguinal ring at about 7 months of intrauterine life. The second phase is hormone dependent and occurs from 7 to 9 months of intra-uterine life. The muscles of the anterior abdominal wall have several functions: loosely attached by connective tissue. This enables local anaesthetic solution to pass freely up and down this space in an abdominal wall field block.
If that timing cannot be achieved mens health quiz questions order speman paypal, it can be done at other times in the cycle as the patient is switching from another reliable method of contraception. The devices may also be inserted in breastfeeding women, who, in fact, demonstrate a lower incidence of postinsertional discomfort and bleeding. Insertion may be performed immediately postpartum (within 10 minutes of placental delivery) or intraoperatively during a cesarean before closure of the hysterotomy incision. Although the expulsion rate is higher, the success rate decreases the pregnancy rate from missed postpartum visits and lengthens the interval between pregnancies. Reconstructed coronal view of uterus with appropriately placed progesterone-containing intrauterine device in endometrial cavity. Reconstructed coronal view of uterus with appropriately placed copper-containing intrauterine device in endometrial cavity. It rarely works by inhibiting implantation and does not function as an abortifacient in normal use. The local progesterone effect is used to relieve pain related to endometriosis and adenomyosis as well as for endometrial protection for women taking hormone replacement therapy who cannot take oral progestins. There is, however, an approximate two- to four-fold increase in the incidence of preterm labor and delivery. If the string is not visible, rotating two cotton-tip applicators in the endocervical canal will often retrieve the strings. It can be given up to 15 weeks after the last injection without requiring additional contraceptive protection, providing a useful "safety margin. Food and Drug Administration has added a warning to this formulation that use beyond 2 years should be carefully considered and alternate contraceptive methods be evaluated. It may also improve management of pain associated with endometriosis, endometrial hyperplasia, and dysmenorrhea. However, hormones are also used in many other contraceptive methods, including injectable hormonal preparations, implantable hormonal rod, hormonecontaining intrauterine systems (as discussed earlier), and contraceptive patches and rings. Although hormonal contraceptive methods are associated with risks, the use of one of these agents is safer than pregnancy for most women. Method (perfect use) failure rates for oral, transdermal, and transvaginal contraceptives are in the range of 1%. Longer-acting hormonal methods (injections, implants, and intrauterine contraception) have effectiveness rates that equal or even surpass those of sterilization. Women who use these techniques should be counseled about high-risk behaviors, safe sexual behaviors, and the need to use condoms for additional protection. It also provides the added effects of thickening the cervical mucus, inhibiting sperm migration, and creating an unfavorable atrophic endometrium for implantation. The estrogen provides an additional modest contraceptive effect, thus increasing the efficacy of this method. Common progestin compounds used in hormonal contraceptives include, in descending order of biologic progestin activity, norgestrel, ethynodiol diacetate, norethindrone acetate, norethynodrel, and norethindrone. Knowing the difference may help in the selection of the most appropriate and acceptable formulation for a patient. The classic regimen for hormonal contraception has been 21 days of active hormone (pill, patch, and ring) and 7 days of placebo or no hormones. Continuous hormone regimens are also available that produce shorter or less frequent menstrual periods, either every 3 or even every 12 months. Some women may prefer this usage pattern, although they should be aware that there is a higher incidence of breakthrough bleeding in the first 12-week cycle, compared with the 4-week cycle preparations. New 576 preparations continue to be developed with the ultimate goal of maximizing the benefits and minimizing the side effects. Ovulation continues normally in about 40% of patients using the progestin-only formulation. In the former group, the progestin effect coincides with the prolactin-induced suppression of ovulation; in the latter group, the inherent reduced fecundity adds to the progestin effect. There is no effect on the quality or quantity of breast milk or any evidence of short- or long-term adverse effects on infants, and the progestin-only pill may be started immediately after delivery in the breastfeeding mother. The progestin-only pill is also an option for women in whom estrogen-containing formulations are contraindicated. Because of the low dosages of progestin, the minipill must be taken at approximately the same time each day, starting on the first day of menses. If a woman is more than 3 hours late in taking the minipill, a back-up contraceptive method should be used for 48 hours. Effects of Hormonal Contraceptives Hormonal contraception affects more than just the reproductive system. Progestins increase sebum, stimulate the growth of facial and body hair, induce smooth muscle relaxation, and increase the risk of cholestatic jaundice. The newer progestational agents-desogestrel, norgestimate, and drospirenone-have less metabolic impact. By decreasing conception, the risk of ectopic pregnancy is reduced, along with the complications of undesired intrauterine pregnancies. Although it is an especially worrisome symptom, it is not associated with decreased efficacy as long as the pill-taking regimen is maintained. The abnormal bleeding pattern is the most common reason for discontinuation of contraception, and women should be counseled to expect irregularities before hormones are initiated.
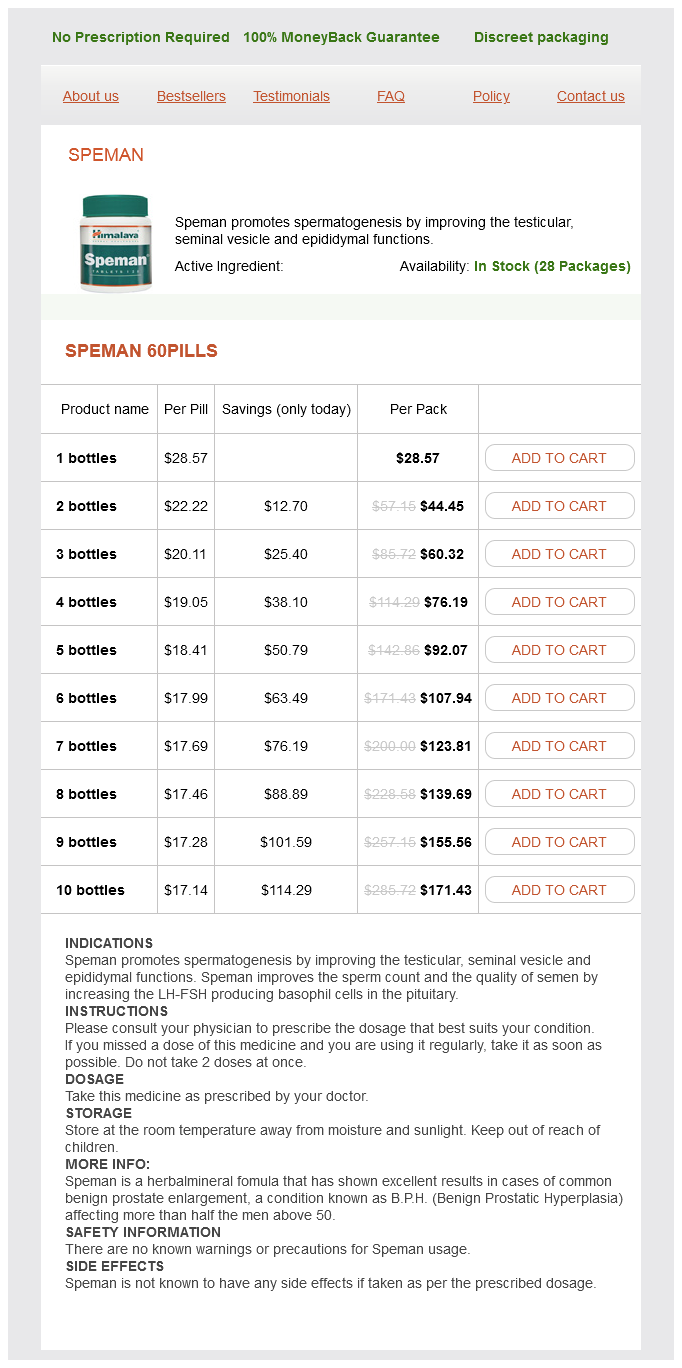
Speman Dosage and Price
Speman 60pills
- 1 bottles - $28.57
- 2 bottles - $44.45
- 3 bottles - $60.32
- 4 bottles - $76.19
- 5 bottles - $92.07
- 6 bottles - $107.94
- 7 bottles - $123.81
- 8 bottles - $139.69
- 9 bottles - $155.56
- 10 bottles - $171.43
I-Intoxication is not likely to cause hemiplegia man health cure cure erectile dysfunction buy speman 60 pills on-line, but ischemia would suggest the transient ischemia of carotid stenosis and migraine. N-Neoplasms of brain (causing hemiplegia) include meningiomas, gliomas, and metastatic carcinoma. An early meningioma of the high cervical cord may rarely be associated with hemiplegia. Approach to the Diagnosis the history is very important in determining the diagnosis of hemiplegia. An acute onset without a history of trauma would suggest a cerebral embolism, hemorrhage, or thrombosis, whereas a gradual onset would indicate a possible neoplasm or other space-occupying lesion. Intermittent occurrence of hemiplegia might suggest migraine, multiple sclerosis, or carotid artery insufficiency. A history of fever may indicate a cerebral abscess or subacute bacterial endocarditis. A central facial palsy or other cranial nerve signs indicate a brain or brain stem lesion as opposed to a cervical cord insult. Spinal fluid analysis should be done if multiple sclerosis or neurosyphilis is suspected. If the blood is bright red and alkaline (use Nitrazine paper to test) and the nasal passages and posterior pharynx are clear, then it is probably hemoptysis. Anatomy is the basic science to apply to develop a differential diagnosis of hemoptysis. Beginning at the larynx and working down the trachea, bronchi, and alveoli, one can quickly recall the major causes of hemoptysis using the cross-index of the various etiologies as in Table 36. Laryngitis is an infrequent cause of hemoptysis, but laryngeal carcinoma may cause it. A foreign body such as a chicken bone lodged in the larynx or trachea should always be considered, especially in children. Additional etiologies of hemoptysis that one might encounter in the trachea are ulceration and rupture of an aortic aneurysm or a carcinoma of the esophagus with a tracheoesophageal fistula. Hereditary telangiectasia may lead to hemoptysis anywhere along the tracheobronchial tree. In the alveoli the acute causes of hemoptysis-pneumonia (pneumococcal and Friedlander, especially), and pulmonary embolism or infarctions-are encountered. Collagen diseases, Goodpasture syndrome, and primary hemosiderosis should be looked for in the elusive cases. Approach to the Diagnosis the differential diagnosis of hemoptysis can be narrowed considerably by the clinical picture. Hemoptysis with chills and 439 fever suggests pneumonia, but one should always keep pulmonary embolism in mind. Hemoptysis with purpura or bleeding from other sites should suggest a systemic disease or coagulation disorder. If routine studies and the clinical picture suggest pneumonia, nothing more may need to be done other than a careful follow-up. If a bronchogenic neoplasm or bronchiectasis is suspected, a pulmonary consult and bronchoscopy would be ordered. She is a 20-year smoker and has had a chronic cough which has become more and more productive in the past 2 years. Physical examination reveals a few sibilant and sonorous rales over both lungs but is otherwise unremarkable. Thus, there are parenchymal cells that can be involved by toxic or inflammatory hepatitis. Infectious hepatitis is most commonly caused by a virus (type A or B; which is usually transfusiontransmitted but may be transmitted by fecaloral route) or by infectious mononucleosis. When considering the supporting tissue, do not forget lupoid hepatitis, periarteritis nodosa, sarcoidosis, and cirrhosis. In addition, because the liver contains von Kupffer cells, any disease causing proliferation of the reticuloendothelial system may produce hepatomegaly. The hepatic veins may be involved with a thrombosis and lead to hepatomegaly (BuddChiari syndrome). The portal veins may be obstructed by thrombophlebitis (pylephlebitis), usually secondary to infection elsewhere in the gut. From the bile canaliculi down to the hepatic and common bile ducts, obstruction may occur from stones, neoplasms (pancreatic or ampullary), infection (cholangitis), or parasites. Chlorpromazine and related drugs cause obstruction of the small canaliculi and present an obstructive picture. Pancreatitis may cause the pancreas to swell and produce bile duct 441 obstruction and hepatomegaly. Extrinsic conditions causing apparent hepatomegaly, but which is really only displacement of the liver, are diaphragmatic abscess and pulmonary emphysema. In hemolytic anemias, the liver may be enlarged because of the increased load on the reticuloendothelial tissue (both in liver and spleen) to dispose of the damaged red cells. Approach to the Diagnosis the clinical picture will help to distinguish many causes of hepatomegaly. Chronic cough, wheezing, jugular vein distention, hepatomegaly, and pitting edema suggest pulmonary emphysema and cor pulmonale. Hepatomegaly and ascites with a history of heavy alcohol intake suggest alcoholic cirrhosis.