Suhagra
General Information about Suhagra
Suhagra is a broadly used medicine for the treatment of erectile dysfunction (ED) in males and pulmonary arterial hypertension (PAH). It is a potent and effective drug that has helped numerous people improve their sexual health and general well-being.
It is essential to note that Suhagra just isn't a cure for ED or PAH. It is a therapy that helps improve the signs and allows for a more satisfying sexual expertise. It does not shield against sexually transmitted infections, and it should not be used by people who are not experiencing ED or PAH.
Suhagra, additionally identified by its generic name sildenafil citrate, belongs to a class of medication known as phosphodiesterase kind 5 (PDE5) inhibitors. It works by relaxing the muscle tissue and rising the blood flow to the penis, allowing for a stronger and longer-lasting erection. This medicine is commonly prescribed to men who've problem reaching or sustaining an erection because of bodily causes such as diabetes, high blood pressure, or nerve damage.
Like any treatment, Suhagra could cause side effects in some individuals. The most typical side effects reported embrace headache, facial flushing, upset abdomen, and dizziness. These unwanted side effects are mild and normally subside on their own. However, if they persist or turn out to be bothersome, it's essential to consult a healthcare supplier for correct guidance.
Erectile dysfunction is a typical condition that impacts males of all ages. It is the inability to realize or maintain an erection sufficient for sexual activity. This is normally a source of nice misery and can result in relationship issues, low shallowness, and even depression. ED could be brought on by varied elements similar to physical conditions, psychological points, or life-style decisions.
In conclusion, Suhagra is an efficient medicine for the remedy of erectile dysfunction and pulmonary arterial hypertension. It has helped many individuals reclaim their sexual well being and enhance their overall quality of life. If you might be experiencing symptoms of ED or PAH, consult your physician to see if Suhagra is right for you. Remember to all the time comply with your doctor's instructions and never take more than the prescribed dose. With the proper treatment and help, ED and PAH could be managed successfully, permitting for a satisfying and enjoyable life.
Aside from its use in treating ED, Suhagra can also be approved for the therapy of pulmonary arterial hypertension (PAH). PAH is a situation where the blood vessels in the lungs turn into slim and put stress on the center, making it difficult for the heart to pump blood to the lungs. This can result in shortness of breath, fatigue, and chest pain. Suhagra works by stress-free the blood vessels in the lungs, reducing the stress and enhancing blood circulate, finally easing the symptoms of PAH.
Suhagra is out there in numerous strengths, ranging from 25mg to 100mg, and is usually taken 30 minutes to 1 hour before sexual exercise. It may be taken with or with out meals, however it is suggested to avoid high-fat meals as they may delay the drug's effects. Its effectiveness can last up to 4 hours, offering ample time for spontaneous sexual activity.
Once warfarin is stopped erectile dysfunction icd 10 purchase suhagra visa, dual antiplatelet therapy with aspirin and clopidogrel are prescribed until completion of 6-month follow-up. If the leak remains greater than 5 mm, the implant is considered a failure and the patient needs to remain on oral anticoagulation. All-cause stroke rates were similar between groups, but the pathophysiology of stroke was significantly different; more warfarin patients experiencing hemorrhagic strokes and more Watchman patients experiencing ischemic strokes. In addition, all-cause bleeding was similar between groups; however, when periprocedural bleeding was excluded, bleeding rates were significantly lower in the Watchman group (likely related to withdrawal of chronic anticoagulation therapy in device patients). However, this reduction in hemorrhagic stroke was balanced by a relative increase in ischemic stroke. Of particular concern, these late ischemic strokes may be related to late thrombus formation on the Watchman device in the absence of anticoagulation. The risk is thought to be highest early after the implant, when endothelialization on the device is still incomplete. For this reason, the standard medical treatment after Watchman implantation, as studied in prospective trials, includes warfarin for 45 days. These modifications include a longer distal lobe, larger diameter of the proximal disc, longer waist between the distal lobe and the proximal disc, recessed end-screw on the proximal disc, and more fixation barbs. With the new Amulet, a larger oversize is recommended: 3 to 5 mm for 16- to 22-mm devices and 3 to 6 mm for 25- to 34-mm devices. If the device release criteria are satisfactory, the device is released by counterclockwise rotation of the delivery cable. If one or more of those criteria appears suboptimal, the device can be retrieved and exchanged or repositioned. The lobe and disc are connected by a short flexible central waist, with two polyester patches sewn onto the two components. The flexible waist allows the disc to self-orient to the cardiac wall and facilitates conformation to variable appendage shapes. Unlike the Watchman device, the length of the Amplatzer Cardiac Plug is shorter than its diameter and, thus, it can be implanted in appendages that are shorter than wide. The diameter of the disc is 4 or 6 mm larger than the lobe for the 16 to 22 mm or 24 to 30 mm devices, respectively. The Amulet, a second-generation Amplatzer Cardiac Plug, has been designed with strategic modifications at improving device stability and Postoperative Management Currently, directions for use of the Amplatzer Cardiac Plug and the Amulet recommend dual antiplatelet therapy for 3 months followed by aspirin alone. In the absence of randomized trials and rigorous follow-up, the significance of device-related thrombosis is not entirely known, but this risk remains a concern. A short course of anticoagulation therapy (similar to that used following Watchman) can potentially reduce the risk of early thrombus formation, especially in patients with markers of increased risk of thrombus formation. Sequence of the Amulet implantation showing the initial position of the delivery cable (A), the inner 0. To date, the published reports of the Amplatzer Cardiac Plug and the Amulet are not as robust as those of the Watchman device. These devices are available outside of the United States, and they have been marketed for use with antiplatelet therapy only, albeit with little supportive evidence. The incidence of device-associated thrombosis has varied among different studies from 3% to 17%. Notably, thrombosis appeared to originate from the central end-screw of the device in a significant proportion of cases. Nonetheless, a recent report found a high incidence of devicerelated thrombosis (17%) despite continued antiplatelet therapy. A particular benefit of the Lariat device when compared with other endovascular devices, particularly the Watchman device, is that anticoagulation is not required preoperatively. Hence, the Lariat procedure can be performed in patients with contraindications to anticoagulation. The combined use of the anteroposterior and left-lateral fluoroscopic views is recommended to assure anterolateral pericardial access. In the anteroposterior fluoroscopic view, the needle is directed toward the left shoulder, just lateral to the pulmonary artery and the hilum of the pulmonary vasculature. There is a curve at the end of the epicardial sheath (marked by the black colored flat surface of the proximal end of the sheath) that should be directed away from the surface of the heart. The dilator and the sheath should never be advanced into the pericardial space without the guidewire. Similarly, the sheath should never be advanced without the dilator or the Lariat device. All the wires and sheaths are then retracted and a pericardial drain is placed and will be left in place. An angiogram (through the occlusion balloon catheter) is performed to confirm guidewire placement. Postoperative Management A pericardial drain is left in place for the next 24 to 48 hours to allow for prompt management of potential pericardial effusion. The drain may be removed once the absence of reaccumulating effusion is verified on echocardiographic examinations over a 24-hour period. Colchicine is frequently used to reduce pain associated with pericarditis and the prevention of Dressler syndrome. Colchicine is usually initiated on the day of the procedure and maintained for 3 to 4 weeks. Dual antiplatelet therapy (aspirin and clopidogrel) or aspirin alone can be considered in patients who cannot tolerate short-term oral anticoagulation. Snaring the Left Atrial Appendage the Lariat is back-loaded over the epicardial magnet-tipped guidewire and, with the snare closed, advanced over the guidewire into the pericardial sheath. Once past the pericardial sheath, the snare is opened fully in the pericardial space.
Stent complications include restenosis due to intimal hyperplasia erectile dysfunction cause of divorce suhagra 100 mg line, acute/subacute thrombus formation, distal stent migration, restenosis of the parent artery, or further injury to the vessel. While the published rates of complications in stent placement vary upon uses in the acute and chronic phase as well as the location of the artery and initial neurological presentation of the patient, the use of stents to treat traumatic vascular pathology remains in high favor. These techniques provide for a faster, safer, and more efficient method of visualizing and treating traumatic arterial injuries following cervical trauma. Cervical root compression by a traumatic pseudoaneurysm of the vertebral artery: case report. Liberalized screening for blunt carotid and vertebral artery injuries is justified. Timing and mechanism of ischemic stroke due to extracranial blunt traumatic cerebrovascular injury. Incidence and trends in the diagnosis of traumatic extracranial cerebrovascular injury in the nationwide inpatient sample database, 20032010. Does improved detection of blunt vertebral artery injuries lead to improved outcomes The high morbidity of blunt cerebrovascular injury in an unscreened population: more evidence of the need for mandatory screening protocols. Helical computed tomographic angiography: an excellent screening test for blunt cerebrovascular injury. Blunt cerebrovascular injuries: redefining screening criteria in the era of noninvasive diagnosis. Western Trauma Association critical decisions in trauma: screening for and treatment of blunt cerebrovascular injuries. Delayed presentation of carotid intimal tear following blunt craniocervical trauma. Stroke prevention by endovascular treatment of carotid and vertebral artery dissections. Treatment-related outcomes from blunt cerebrovascular injuries: importance of routine follow-up arteriography. The unrecognized epidemic of blunt carotid arterial injuries: early diagnosis improves neurologic outcome. Extracranial internal carotid artery dissections: noniatrogenic traumatic lesions. Blunt vertebral artery injuries in the era of computed tomographic angiographic screening: incidence and outcomes from 8,292 patients. Dissecting aneurysm of the vertebral artery and cervical manipulation: a case report with autopsy. Vertebrovertebral arteriovenous fistula diagnosis and treatment: report of 8 cases and review of the literature. Nonsurgical treatment of unruptured intracranial vertebral artery dissection with serial follow-up angiography. Computed tomographic angiography for the diagnosis of blunt carotid/vertebral artery injury: a note of caution. Blunt vascular neck injuries: diagnosis and outcomes of extracranial vessel injury. Antithrombotic therapy and endovascular stents are effective treatment for blunt carotid injuries: results from long term follow up. Endovascular treatment of intracranial arteriovenous malformations with onyx: technical aspects. Angioplasty and stenting of symptomatic and asymptomatic vertebral artery stenosis: to treat or not to treat. Endovascular treatment of distal cervical and intracranial dissections with the neuroform stent. Emergent self-expanding stent placement for acute intracranial or extracranial internal carotid artery dissection with significant hemodynamic insufficiency. Pipeline embolization device as primary treatment for cervical internal carotid artery pseudoaneurysms. Endovascular treatment of carotid and vertebral pseudoaneurysms with covered stents. Vertebral artery pseudoaneurysms secondary to blunt trauma: endovascular management by means of neurostents and flow diverters. Pipeline Embolization Device as primary treatment for blister aneurysms and iatrogenic pseudoaneurysms of the internal carotid artery. Successful treatment of a traumatic carotid pseudoaneurysm with the Pipeline stent: case report and review of the literature. Treatment of a giant vertebral artery pseudoaneurysm secondary to gunshot wound to the neck using pipeline embolization device. Application of Pipeline Embolization Device for iatrogenic pseudoaneurysms of the extracranial vertebral artery: a case report and systematic review of the literature. Successful treatment of iatrogenic vertebral pseudoaneurysm using pipeline embolization device. Pipeline embolization device and subsequent vessel sacrifice for treatment of a bleeding carotid pseudoaneurysm at the skull base: a case report. Yom, and Kern Singh Abstract After trauma to the cervical spine, the first decision in the treatment algorithm is between surgical and conservative management. When surgical therapy is required, cervical fusion procedures are frequently utilized. Consequently, decisions regarding bone grafting options are of significant concern. During graft selection, considerations must be made regarding many factors, such as osteogenic potential, biocompatibility, cost, structural support, site of implantation, immunogenetics, and preservation techniques. While autologous bone graft remains the gold standard in cervical spine fusion procedures, obtaining such grafts is not without disadvantages.
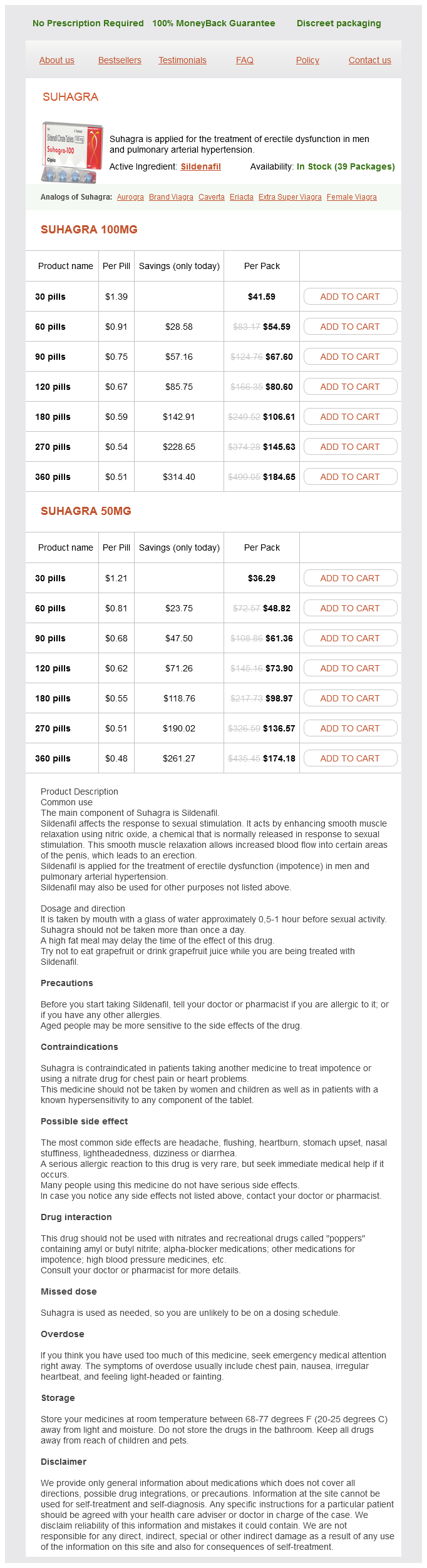
Suhagra Dosage and Price
Suhagra 100mg
- 30 pills - $41.59
- 60 pills - $54.59
- 90 pills - $67.60
- 120 pills - $80.60
- 180 pills - $106.61
- 270 pills - $145.63
- 360 pills - $184.65
Suhagra 50mg
- 30 pills - $36.29
- 60 pills - $48.82
- 90 pills - $61.36
- 120 pills - $73.90
- 180 pills - $98.97
- 270 pills - $136.57
- 360 pills - $174.18
Furthermore encore erectile dysfunction pump suhagra 100 mg buy, they found cervical spinal stenosis only in players whose stingers were caused by the extension-compression mechanism described above, supporting their claim that a normal Torg ratio may protect 124 Cervical Spine Trauma in Patients with Congenital Spinal Stenosis 17. Patients with central cord syndrome should be immobilized with a hard collar to prevent further injury, and medical management should entail placement in intensive care, respiratory protection, and maintenance of mean arterial blood pressure at 85 to 90 mm Hg to improve spinal cord perfusion. In certain subsets of patients, central cord syndrome can be managed surgically with anterior cervical decompression and fusion, posterior cervical decompression and fusion, or posterior cervical decompression alone. When a stinger is suspected, initial evaluation should include localization of symptoms (unilateral vs. Imaging studies of athletes can be conducted to identify underlying pathological conditions and to inform decisions regarding return to play. The following conditions were considered relative contraindications: (1) Torg ratio < 0. Prophylactic Decompression Prophylactic decompression has been performed on patients with congenital cervical spinal stenosis to prevent neurological injury from minor degenerative lesions that would be insignificant in a nonstenotic canal. The value of prophylactic decompression for the prevention of neurological injury resulting from trauma in patients with congenital stenosis has been questioned. In their study of the prevalence of cervical spinal stenosis in skeletal specimens, Lee et al5 noted that although an estimated 4. The authors, therefore, recommend that prophylactic decompression should not be performed solely on the basis of radiographic evidence of cervical stenosis. Decisions regarding prophylactic decompression should not rely solely on identification of congenital stenosis using the Torg ratio because doing so will fail to identify canal narrowing around the disc caused by spondylosis or soft-tissue protrusion. In patients with cervical spine trauma, practitioners should include consideration of congenital stenosis in their decisionmaking before recommending a return to contact activities. Establishment of parameters for congenital stenosis of the cervical spine: an anatomic descriptive analysis of 1,066 cadaveric specimens. Incidence of cervical spinal stenosis in professional and rookie football players. The prevalence of congenital cervical spinal stenosis in 262 college and high school football players. Cervical spinal stenosis and sports-related cervical cord neurapraxia in children. Normal cervical spine morphometry and cervical spinal stenosis in asymptomatic professional football players. Plain film radiography, multiplanar computed tomography, and magnetic resonance imaging. Cervical spinal cord contusion in professional athletes: a case series with implications for return to play. Sagittal measurements of the cervical spine in subaxial fractures and dislocations. An analysis of two hundred and eighty-eight patients with and without neurological deficits. Clinical relationship between cervical spinal canal stenosis and traumatic cervical spinal cord injury without major fracture or dislocation. Prognostic factors in distractive extension injuries of the subaxial cervical spine. Cervical cord neurapraxia: classification, pathomechanics, morbidity, and management guidelines. The relationship of developmental narrowing of the cervical spinal canal to reversible and irreversible injury of the cervical spinal cord in football players. Permanent partial cervical spinal cord injury in a professional football player who had only congenital stenosis. A histopathological analysis of the human cervical spinal cord in patients with acute traumatic central cord syndrome. Central cord syndrome resulting from congenital narrowness of the cervical spinal canal. Central cord syndrome in a football player with congenital spinal stenosis: a case report. National trends in the management of central cord syndrome: an analysis of 16,134 patients. Suggested management guidelines for participation in collision activities with congenital, developmental, or postinjury lesions involving the cervical spine. Functional cervical spinal stenosis: a contraindication to participation in contact sports. Clinical influence of cervical spinal canal stenosis on neurological outcome after traumatic cervical spinal cord injury without major fracture or dislocation. With careful consideration of the patient and these principles, successful management of traumatic injuries in the cervical spine can be effectively accomplished. Keywords: cervical spine, trauma, rheumatoid arthritis, nonoperative management, operative management, spinal instrumentation, case examples and acute traumatic lesions. It is, therefore, incumbent upon evaluating health care providers to obtain an appropriate patient history including past medical history and medication history, in addition to the standard trauma history that accompanies a recent history of injury. Patients with new or increased neck pain should always be carefully screened both clinically and radiographically as part of a complete spine workup. Outside of imaging assessments, repeat clinical and neurological assessments have a potential to play a key role in patients 18. Distracting injuries should be successfully treated and appropriately managed prior to full clearance of the cervical spine in this unique patient population. In addition, if rheumatoid pathology is discovered in the cervical spine, this may play a role in anesthesia care and careful intubation, even if no traumatic injury is ultimately identified in the cervical spine. Moving beyond single plane wiring techniques, multipoint posterior screw/rod fixation systems using the novel screw placement is now the standard of care.