Sulfasalazine
General Information about Sulfasalazine
The energetic ingredient in Azulfidine is sulfasalazine, a sulfa drug that works by reducing inflammation in the colon. It is believed to inhibit the production of chemical compounds referred to as prostaglandins, which contribute to irritation within the physique. This medication is out there in both tablet and liquid kind, and is usually taken several times a day.
Azulfidine, also recognized by its generic name sulfasalazine, is a medicine primarily used for the remedy of ulcerative colitis. This chronic inflammatory disease affects the massive gut, inflicting painful and infrequently bloody bowel actions. Azulfidine can additionally be used to forestall the recurrence of flare-ups in sufferers who have already experienced ulcerative colitis.
In conclusion, Azulfidine is a commonly prescribed medicine for the remedy of ulcerative colitis. It works by decreasing irritation within the colon and might help to stop the recurrence of flare-ups. While it might cause some unwanted aspect effects, many patients have found relief from their signs with using Azulfidine. As with any medication, it could be very important comply with your physician's directions and report any regarding unwanted side effects. With correct management and therapy, patients with ulcerative colitis can lead a more healthy and extra comfortable life.
Ulcerative colitis is a situation that impacts tens of millions of people worldwide, and there could be currently no treatment. The symptoms of this disease can range from mild to severe, and will include stomach pain, diarrhea, rectal bleeding, and fatigue. These signs can significantly impression an individual's high quality of life and make it troublesome to carry out every day actions. Azulfidine helps to relieve these symptoms and improve the overall well-being of patients.
In addition to treating ulcerative colitis, Azulfidine has also been found to be effective in treating different inflammatory conditions such as rheumatoid arthritis and ankylosing spondylitis. It works by decreasing joint ache and stiffness, and likewise helps to prevent joint harm in these situations.
It is necessary to note that Azulfidine shouldn't be used in patients who are allergic to sulfa drugs, as it might possibly cause a extreme allergic reaction. It can also be not recommended for pregnant or breastfeeding women, as sulfasalazine can pass into breast milk and harm the infant. Patients with a historical past of liver or kidney disease should also use caution when taking this medication.
Like any medicine, Azulfidine could cause unwanted effects in some people. These can embrace nausea, vomiting, headache, and pores and skin rash. Some patients can also expertise a decrease in the variety of white blood cells, which might enhance the risk of infections. It is necessary to debate any potential side effects together with your doctor earlier than beginning Azulfidine.
At week 52 stomach pain treatment natural discount 500 mg sulfasalazine, all subjects were re-randomized to either placebo or lorcaserin for an additional year. Subjects who showed a weight loss of greater than 5% in the first year and were maintained on lorcaserin treatment in the second year were able to maintain their weight loss better than those who had been switched to placebo. Phentermine is an adrenergic agonist that promotes weight loss by activation of the sympathetic nervous system with a subsequent decrease in food intake and increased resting energy expenditure. Inhibiting reuptake of dopamine and/or norepinephrine modulates the "reward pathway" that various foods can stimulate. Naltrexone is a pure opioid antagonist that blocks an opioid pathway that may slow weight loss. Abrupt discontinuation of chronic use of alcohol, benzodiazepines, barbiturates, or antiepileptic drugs may further increase the risk for seizure. Bupropion/naltrexone should be avoided in patients with uncontrolled hypertension, history of seizures, or if there is a recent history of bulimia or anorexia nervosa. The primary endpoints were percent change from baseline body weight and the proportion of patients achieving at least a 5% reduction in body weight. Both 56-week, randomized, placebo-controlled, double-blind clinical trials illustrated significantly greater mean weight loss with liraglutide than with placebo (8% vs. By the end of the study, participants in the liraglutide group lost an additional 6. Although liraglutide is associated with improvements in blood pressure and lipids, it was found to increase heart rate by 2. Liraglutide carries a black box warning on the association with medullary thyroid cancer in rodents although the relevance to humans has not been determined. On average, 120 mg of orlistat taken 3 times per day will decrease fat absorption by 30%. In addition, a device under investigation is the Gelesis hydrogel capsule that expands in the stomach, increases satiety, and may improve glycemic control. In animal studies, peripheral administration of liraglutide results in uptake in specific brain regions regulating appetite including the hypothalamus. A study involving obese individuals without diabetes demonstrated that liraglutide 3. Causes can be attributed to a combination of genetic, epigenetic, and environmental and lifestyle phenomena. Current treatments range from dietary and behavioral interventions to pharmacologic and surgical therapies in more severe cases. There are several new medical therapies with separate mechanisms of action that are in clinical trials as well as new devices. Management of obesity is evolving and obesity is now viewed as a multi-factorial chronic disease that needs to involve a combination of medical therapies and, when appropriate, interventional procedures. Regular consumption from fast food establishments relative to other restaurants is differentially associated with metabolic outcomes in young adults. The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review. Glycemic index, glycemic load, and chronic disease risk-a meta-analysis of observational studies. Relation between changes in intakes of dietary fiber and grain products and changes in weight and development of obesity among middleaged women. Declining rates of physical activity in the United States: what are the contributors Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. Fetal programming of body composition, obesity, and metabolic function: the role of intrauterine stress and stress biology. Ten-year weight gain in smokers who quit, smokers who continued smoking and never 29. Is the gut microbiota a new factor contributing to obesity and its metabolic disorders Effects of Recombinant leptin therapy in a child with congenital leptin deficiency. The diagnosis and management of Lipodystrophy syndromes: a multi-society practice guideline. Reliability and practicality of measuring waist circumference to monitor cardiovascular risk among community mental health center patients. Long-term influences of bodyweight changes, independent of the attained weight, on risk of impaired glucose tolerance and type 2 diabetes. Restoring the salivary cortisol awakening response through nasal continuous positive airway pressure therapy in obstructive sleep apnea. Osteoarthritis, obesity and weight loss: evidence, hypotheses and horizons-a scoping review. Severe obesity and comorbid condition impact on the weight-related quality of life of the adolescent patient. Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: a meta-analysis of randomized controlled clinical trials. Evaluation of meal replacements and a home food environment intervention for long-term weight loss: a randomized controlled trial. Efficacy of a liquid lowenergy formula diet in achieving preoperative target weight loss before bariatric surgery. Metabolic adaptation following massive weight loss is related to the degree of energy imbalance and changes in circulating leptin.
Close attention should be paid to avoiding uterine perforation pain treatment in shingles sulfasalazine 500 mg low cost, which can happen at any time during the procedure from uterine sounding, cervical dilation, hysteroscope insertion, and/or during fibroid resection. Perforation occurring at the time of cervical dilation is most commonly due to cervical stenosis, a severely retro- or anteverted uterus, or in nulliparous/menopausal women. If uterine perforation is recognized, it is important to identify which steps of the hysteroscopy have been completed thus far; regardless, the procedure should be terminated. If only a mechanical perforation without suspicion of bowel damage, patients can be placed in extended observation for a few additional hours and discharged home. If perforation is secondary to an activated electrode or sharp instrument, one should assume the possibility of bowel injury, and diagnostic laparoscopy should be performed immediately. If perforation is noted, the perforation should be sutured in patients of reproductive age even if hemostatic due to the risk of uterine rupture during pregnancy [25]. Once all equipment has been set up and hysteroscopy can commence, a distending media is used (described in more detail later). The decision for fluid distention (both fluid type and distending pressure) should be based on the procedure planned, and it is critical to be familiar with possible complications and acceptable fluid deficits. Fluid deficit is the difference between the total amount of solution instilled into the uterus and the amount of fluid recovered from the hysteroscope outlet channel and the plastic draping pouch used to funnel escaping fluid through the cervix through a tube into a calibrated bottle. Many fluid management systems can measure both instilled and recovered fluid and give the fluid deficit on the machine control panel. The surgeon should continue to communicate with operating room staff regarding fluid deficit over time in order to plan the timing of the remainder of the surgery, and if all specimens can be removed safely in line with fluid deficit restrictions. Three types of distending media are available: carbon dioxide gas, hypotonic nonconductive fluid (glycine, sorbitol, mannitol), and isotonic conductive fluids (normal saline). Carbon dioxide is only available for diagnostic use and because it has a risk of gas embolization, it is not discussed further with regard to operative hysteroscopic surgery in this chapter. Hypotonic fluids like those described earlier are used with monopolar energy and can have significant complications, such as volume overload, water intoxication, pulmonary edema, severe hyponatremia, and cerebral edema. Isotonic fluids used with bipolar energy are generally better tolerated with the most common complication being fluid overload, generally easily treatable with diuretics. Regardless of the fluid medium, steps should be taken to minimize fluid intravasation, especially in cases with increased risk with larger intracavitary component. The American Association of Gynecologic Laparoscopists recommends a maximum fluid deficit of 750 mL for elderly patients or those with cardiac comorbidities and 1000 and 2500 mL for younger, healthy patients with hypotonic and isotonic solutions, respectively [27]. Diagnostic hysteroscopy, most commonly with a rigid 5 mm hysteroscope, is recommended prior to initiation of operative hysteroscopy to confirm imaging findings and to determine the surgical plan. An outer sheath is generally necessary to allow for inflow and outflow channels for fluid distention and generation of a lavage system for the uterine cavity for improved visualization. Cervical dilation is generally not necessary in most patients prior to diagnostic hysteroscopy, although special consideration for nulliparous or menopause women should be made which may require dilation. Bipolar instruments, in which both electrodes are introduced into the thermal loop, are generally safer as current only passes through the tissue with which the loop comes into contact, minimizing the danger derived from random passage from the corporeal structures. While other methods exist, such as vaporization with laser therapy, electrosurgical loop resection is the most commonly performed. When dealing with small submucosal fibroids, particularly in patients with infertility, it might be ideal to avoid electrosurgery in order to decrease adhesion rate. This removes the time-consuming nature of repeat manual extraction of shaved fragments for improved visualization. Benefits of these devices include improved complete resection, low complication Hysteroscopic Myomectomy 109 rates (less than 1%), faster removal, and reduced mean operating time. One must take caution with fibroids greater than 4 cm, as often there is a lower complete resection rate with morcellation devices and more need for conversion to electrosurgical technique, especially with a significant intramural component [28,29]. If pedunculated submucosal fibroids are noted (type 0), the base of the pedicle can generally be transected easily with the electrosurgical loop and is generally performed using a slicing technique of the cutting loop until normal myometrial fibers can be noted (more vascular and pink-appearing layer of tissue). The fibroid can then be extracted either with the loop or sometimes blindly with a curette or grasper. With type 1 or 2 fibroids, the procedure can become somewhat more complex, which may require multiple rounds of resection of the fibroid from the intracavitary layer up toward the myometrium. The Mazzon technique, with a described up to 88% success rate in one-step surgical removal of type 1 and 2 fibroids, uses cold loop to minimize both thermal damage to healthy myometrium as well as decrease synechiae formation. Mechanical enucleation of intramural components over slicing not only respects the anatomy and integrity of the myometrium but also avoids significant risks such as thermal perforation [30]. This involves using a U-shaped cutting loop to slice down to the level of the endometrial surface, then inserting the resectoscope loop into the cleavage plane between the myoma and myometrium to bring the intramural component into the uterine cavity. Saline infusion would then be discontinued and restarted multiple times to induce rapid intrauterine pressure changes and stimulate contractions as well as act as a component of bimanual massage. Office Myomectomy Office hysteroscopy is generally feasible and safe for both diagnosis and occasionally treatment of small intrauterine pathologies, which is often referred to as the "see and treat" approach. Office hysteroscopy can be considered with less than 5 mm hysteroscopes to minimize the risk of cervical dilation, need for anesthesia, and costs. The other benefits include immediate resumption of normal activities postprocedure, when nonsteroidal anti-inflammatory drugs alone are used, and although pain is the primary reason for aborting in-office procedures, the use of opioid medications or anxiolytics has not shown any added benefit. The most common complications from in-office hysteroscopy include vasovagal reaction, local anesthesia toxicity, uterine perforation, uterine hemorrhage, and false passages. It is recommended that both office and clinical staff undertake a safety self-assessment and practice simulated patient scenarios at regular intervals to be prepared for situations with procedural complications. Postoperative Care Postoperative care is generally straightforward, and patients should be discharged home the same day unless any of the complications mentioned earlier were to occur requiring extended observation or management (perforation, excessive fluid intravasation). There are no restrictions on return to normal activity following hysteroscopic myomectomy, and patients should be able to shower when they return home after surgery. Patients should be counseled that vaginal spotting can occur for up to 4 weeks after surgery, although strict precautions for heavy bleeding (changing two pads per hour for over 2 hours), fevers, foul-smelling discharge, or severe abdominal pain should prompt reevaluation prior to the postoperative visit. Data have shown that there is an approximate 30% 3-year cumulative recurrence rate with reoperation rates of approximately 5%20% at 34 years [26,33].
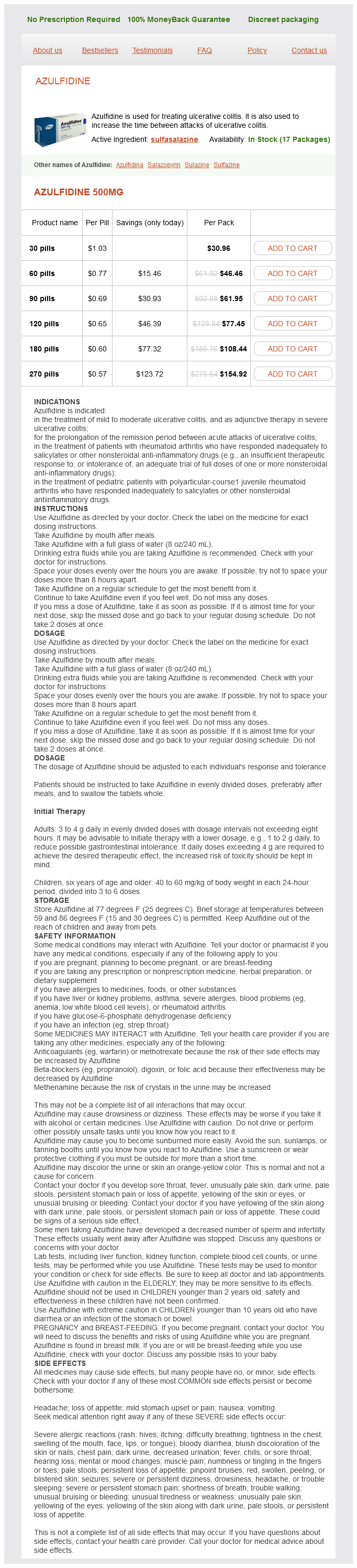
Sulfasalazine Dosage and Price
Azulfidine 500mg
- 30 pills - $30.96
- 60 pills - $46.46
- 90 pills - $61.95
- 120 pills - $77.45
- 180 pills - $108.44
- 270 pills - $154.92
Implantation of autologous muscle-derived stem cells in treatment of fecal incontinence: results of an experimental pilot study neck pain treatment exercise buy discount sulfasalazine 500 mg. A new method for treating fecal incontinence by implanting stem cells derived from human adipose tissue: preliminary findings of a randomized doubleblind clinical trial. Bowel dysfunction following spinal cord injury: a description of bowel function in a spinal cord-injured population and comparison with age and gender matched controls. Antegrade continence enema for the treatment of neurogenic constipation and fecal incontinence after spinal cord injury. Diagnosis and treatment efficacy of functional non-retentive fecal soiling in childhood. Bowel training in spina bifida: importance of education, patient compliance, age, and anal reflexes. Social and emotional impact of faecal incontinence after surgery for anorectal abnormalities. Biofeedback training in treatment of childhood constipation: a randomized controlled study. A controlled trial of an intervention to improve urinary and fecal incontinence and constipation. Does treatment of constipation improve faecal incontinence in institutionalized elderly patients Chronic constipation is diagnosed when a person describes symptoms of constipation for at least 3 consecutive months. Chronic constipation is usually due to a disorder of colonic propulsion and/or rectal evacuation1 and can be divided into 3 categories: slow-transit constipation, normal-transit constipation, and rectal evacuation disorder. Chronic constipation affects a substantial portion of the Western population and is particularly prevalent in women, children, and older adults. The most common terms used by young healthy adults to define constipation are straining (52%), hard stools (44%), and inability to have a bowel movement (34%). The Rome criteria include symptoms suggestive of pelvic floor dyssynergia or outlet obstruction Sensation of anorectal obstruction/blockage during more than 25% of defecations As shown in a National Canadian Survey, only 34% of people who reported constipation had seen a physician for their symptoms. In general, the prevalence is highest when constipation is self-reported16 and lowest when the Rome criteria for constipation are applied. The frequency of is higher among women, older adults, and those with a lower socioeconomic status. Diet and lifestyle may also play a role in the development of constipation (Box 19. Incidence Talley and colleagues surveyed 690 nonelderly residents of Olmsted County, Minnesota, at baseline and after 12 to 20 months. The rate of new constipation in this study was 50/1000 person-years, whereas the disappearance rate was 31/1000 person-years. In a similar study, residents were surveyed Gender the prevalence of self-reported constipation is 2 to 3 times higher in women,18,26,30,44 particularly women of reproductive age, than men, and infrequent bowel movements The frequency of constipation was significantly higher in children with a family history of constipation (49% vs. In populationbased surveys, people with a lower-income status have higher rates of constipation than those who have a higher income status. Constipation in older adults is most commonly characterized by excessive straining and hard stools53 rather than a decrease in stool frequency. In a community sample of 209 people aged 65 to 93 years, the main symptom used to describe constipation was the need to strain at defecation; only 3% of men and 2% of women reported that their average bowel frequencies were less than 3 per week. A study of patients on a geriatrics ward in the United Kingdom showed that up to 42% had a fecal impaction while hospitalized. Fecal retention with fecal soiling is a common cause of impaired quality of life and the need for medical attention in childhood. Diet and Physical Activity Cross-sectional studies have not linked a low intake of fiber with constipation. In one trial, symptoms of constipation did not improve after a 4-week exercise program. Some, but not all, observational studies have found an association between slow colonic transit and dehydration. Medication Use In a review of 7251 patients with chronic constipation (and nonconstipated controls) from a general practice database, medications that were significantly associated with constipation were opioids, diuretics, antidepressants, antihistamines, antispasmodics, anticonvulsants, and aluminum antacids (Box 19. Ingestion of coarse bran (10 g twice daily) was shown to reduce colonic transit by about one third, whereas ingestion of the same quantity of fine bran led to no significant decrease. The colon extracts most of the 1000 to 1500 mL of fluid that crosses the ileocecal valve and leaves only 100 to 200 mL of fecal water daily. Sodium-chloride exchange and short-chain fatty acid transport are the principal mechanisms for stimulating water absorption in the colon. The absorption of water in the colon also depends on an intact epithelial barrier function to prevent the back diffusion of electrolytes and other solutes once they have been absorbed across the epithelium. Although only a small fraction of patients with constipation have megacolon or megarectum, most patients with dilatation of the colon or rectum report constipation. Muscle activity is affected by sleep and wakefulness, eating, emotion, colon contents, and drugs. Neural control is partly intrinsic and partly extrinsic by the sympathetic nerves and the parasympathetic sacral outflow. The mean colonic transit in healthy volunteers is 34 to 35 hours, with an upper limit of normal of 72 hours. Once initiated, peristalsis can be propagated for long distances, thereby moving material through the gut. Unabsorbed carbohydrates, such as starches and non-starch polysaccharides, that enter the cecum serve as substrate for bacterial proliferation and fermentation, yielding short-chain fatty acids and gas (see Chapter 17). In one study that included 14 patients with slow-transit constipation, during a 24-hour period, 4 patients had no peristaltic movement, whereas in the remaining 10 patients peristaltic movements were fewer in number and shorter in duration compared with healthy controls.