Tadalis SX
General Information about Tadalis SX
Tadalis SX incorporates the active ingredient Tadalafil, which is also found in the brand-name medicine Cialis®. Tadalafil is a phosphodiesterase type 5 (PDE5) inhibitor that relaxes the blood vessels in the penis, allowing for elevated blood circulate throughout sexual stimulation. This ends in a firm and lasting erection, which is essential for a satisfying sexual experience.
Tadalis SX is a drugs used to treat sexual perform issues in males, specifically erectile dysfunction. It is manufactured by Ajanta Pharma, which is a reputable pharmaceutical company primarily based in India. Ajanta Pharma has a global presence and is understood for its high-quality generic drugs.
Tadalis SX works by growing the production of nitric oxide within the body, which is responsible for stress-free the sleek muscle tissue within the penis. This relaxation permits for elevated blood flow, which is crucial for achieving and maintaining an erection. It additionally works by blocking the action of PDE5, which is answerable for breaking down the erection-inducing chemical called cGMP. By inhibiting the motion of PDE5, Tadalis SX helps to maintain up high levels of cGMP, leading to improved blood move and a stronger erection.
Tadalis SX is suitable for males over the age of 18 who are experiencing erectile dysfunction. It is not really helpful for ladies or children, and people with underlying medical circumstances corresponding to heart illness, kidney or liver problems, or high or low blood pressure should seek the advice of their doctor before utilizing Tadalis SX. Additionally, it's essential to disclose another medications you are taking, as Tadalis SX might work together with sure drugs, together with nitrates, alpha-blockers, and some antibiotics and antifungal drugs.
Tadalis SX is an efficient treatment for erectile dysfunction, with a success fee of over 80%. It is well-tolerated, and the commonest unwanted facet effects reported by customers include complications, indigestion, again pain, and muscle aches. These side effects are normally gentle and resolve on their own. Tadalis SX can be more affordable than its brand-name counterpart Cialis®, making it an accessible choice for these on the lookout for an economical treatment for ED.
In conclusion, Tadalis SX is a safe and effective medication for the remedy of erectile dysfunction. It provides a viable solution for men who wish to enhance their sexual perform and improve their total high quality of life. However, it is important to seek the advice of a health care provider earlier than utilizing Tadalis SX to make sure it's suitable for you and to discuss any potential interactions or side effects. With Tadalis SX, men can regain their sexual confidence and enjoy a satisfying and satisfying sex life.
Tadalis SX: The Solution for Erectile Dysfunction
Erectile Dysfunction (ED), also referred to as impotence, is a standard condition in males that may have vital impacts on their emotional and psychological well-being. This situation is characterized by the lack to realize or maintain an erection adequate for sexual intercourse. While it could happen sporadically, persistent ED can have a detrimental effect on a man’s confidence, vanity, and relationships. Fortunately, with developments in medical science, there are efficient treatments out there to deal with this situation. One such treatment is Tadalis SX.
Tadalis SX is available in tablet kind with dosages of 10mg and 20mg. The ordinary beginning dose is 10mg, taken at least 30 minutes earlier than sexual exercise. However, relying in your response to the treatment, your doctor could regulate the dosage to 20mg or lower it to 5mg. Tadalis SX shouldn't be taken more than once a day and ought to be taken as prescribed by your physician. It could be taken with or with out meals however could take longer to work if taken with a high-fat meal.
Time course of neuromuscular effects and pharmacokinetics of rocuronium bromide (Org 9426) during isoflurane anaesthesia in patients with and without renal failure impotence lotion buy discount tadalis sx 20 mg on-line. End-stage renal failure reduces central clearance and prolongs the elimination of half-life of remifentanil. Pharmacokinetics and pharmacodynamics of atracurium during isoflurane anesthesia in normal and anephric patients. Diagnosis and management of coronary artery disease in patients with end-stage renal disease on hemodialysis. Pharmacokinetics of 1R-cis 1R-cis atracurium besylate (51 W89) and plasma laudanosine concentrations in health and chronic renal failure. Absence of biochemical evidence for renal and hepatic dysfunction after 8 hours of 1. Patient survival after kidney transplantation: relationship to pretransplant cardiac troponin T levels. Pharmacokinetics and pharmacodynamics of remifentanil in persons with renal failure compared with healthy volunteers. Peri-operative cardiac morbidity in kidney transplant recipients: incidence and risk factors. Propofol infusion for induction and maintenance of anaesthesia in patients with endstage renal disease. Pharmacokinetics of propofol and haemodynamic changes during induction of anaesthesia in uraemic patients. Comparison of propofol/ alfentanil anaesthesia with isoflurane/N2O/fentanyl anaesthesia for renal transplantation. Readmission to an intensive care unit following liver and kidney transplantation: a 50-month study. Risk factors for delayed graft function in cadaveric kidney transplantation: a prospective study of renal function and graft survival after preservation with University of Wisconsin solution in multi-organ donors. Cardiovascular risk factors of sirolimus compared with cyclosporine: early experience from two randomized trials in renal transplantation. Cardiovascular risk assessment among potential kidney transplant candidates: approaches and controversies. Exercise in hemodialysis patients after treatment with recombinant human erythropoietin. Pharmacokinetics of pancuronium in patients with normal and impaired renal function. Prognostic value of dipyridamole thallium-201 screening to minimize perioperative cardiac complications in diabetics undergoing kidney or kidneypancreas transplantation. Perioperative anticoagulation and antiplatelet therapy in renal transplant: is there an increase in bleeding complication? Treatment of the anemia of progressive renal failure with recombinant human erythropoietin. The pharmacokinetics and pharmacodynamics of atracurium in patients with and without renal failure. Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Renal concentrating function with prolonged sevoflurane or enflurane anesthesia in volunteers. Sevoflurane degradation product concentrations with soda lime during prolonged anesthesia. Death in the first year after kidney transplantation: implications for patients on the transplant waiting list. Evaluation of induction doses of propofol: comparison between endstage renal disease and normal renal function patients. Cardiac events in patients undergoing noncardiac surgery: shifting the paradigm from noninvasive risk stratification to therapy. Dopamine treatment of human cadaver kidney graft recipients: a prospectively randomized trial. The effect of different crystalloid solutions on acid΢ase balance and early kidney function after kidney transplantation. Pharmacokinetics and pharmacodynamics of the three isomers of mivacurium in health, in end-stage renal failure and in patients with impaired renal function. Laser Doppler blood flow measurement as a predictor of viability of renal allografts. Anaesthesiological complications in renal transplantation: a retrospective study of 500 transplantations. Comparison of a continuous glucose-insulin-potassium infusion versus intermittent bolus application of insulin on perioperative glucose control and hormone status in insulin-treated type 2 diabetics. Dobutamine stress echocardiography for the detection of significant coronary artery disease in renal transplant candidates. Changes in renal blood flow in response to sympathomimetics in the rat transplanted and denervated kidney. Improvement of left ventricular function and arterial blood pressure 1 year after simultaneous pancreas kidney transplantation. The impact of timing of maximal crystalloid hydration on early graft function during kidney transplantation. The effect of repeated doses of succinylcholine on serum potassium in patients with renal failure. Defective high-density lipoprotein composition in patients on chronic hemodialysis. Predictability of difficult laryngoscopy in patients with long-term diabetes mellitus. Increased volume of gastric contents in diabetic patients undergoing renal transplantation: lack of effect with cisapride.
Graft loss was numerically higher in the groups receiving sirolimus but not significantly so (2-year graft survival 88 erectile dysfunction due to medication cheap tadalis sx 20 mg amex. Adverse events were the primary reason for patients not continuing in the study and this occurred in 34. The authors concluded that sirolimus-based regimens were not associated with improved outcomes after kidney transplantation. Acute rejection (biopsy-proven) in the first 6 months was three times higher in the low-dose sirolimus group (35. Allograft survival at 12 months (censored for death with a functioning transplant) was also significantly lower in the low-dose sirolimus and standard-dose cyclosporine groups (91. Withdrawal from the study, mainly because of treatment failure (use of additional immunosuppressive agents and discontinuation of study drug), was highest in recipients randomized to low-dose sirolimus (48. In this study, therefore, low-dose sirolimus resulted in higher rates of biopsy-proven rejection and no improvement in renal function compared to the cyclosporine-based regimens. However, the study was not powered to detect differences in the key end-points at 3 years. The number of patients in the low-dose sirolimus group who remained on sirolimus for the entire 3-year study period was low, although their average renal function at 3 years was numerically, but not significantly, slightly higher than that of patients remaining on the original agents in the other three groups. Small numbers of patients in the study and an unequal distribution of African Americans between the six study groups meant that the results were difficult to interpret. Nevertheless, the study showed that the combination of sirolimus and cyclosporine was more potent than cyclosporine alone in the prevention of acute rejection and that half-dose cyclosporine and sirolimus were as efficacious as full-dose cyclosporine and sirolimus. The higher incidence of acute rejection seen in African Americans in this study was also observed in subsequent studies. Note: Acute rejection incidence and creatinine clearance (Nankivell formula) are 6-month values; graft and patient survivals are 12-month values. Both studies showed a clear benefit in terms of reduction in the rate of acute rejection for patients receiving sirolimus, an effect that was more marked in patients receiving a higher dose of sirolimus. These two pivotal studies in the development of sirolimus reveal much about how best to use sirolimus and its drawbacks. Of particular importance was the observation that the renal function of patients on a combination of sirolimus and cyclosporine was worse than that of patients on cyclosporine alone, with a 12-month calculated creatinine clearance of 67. The immunosuppressive synergy between cyclosporine and sirolimus in these studies was analyzed by median effect analysis of the pooled data. Experimental data also suggest that synergism accounts for the increased nephrotoxicity. An early multicenter clinical trial conducted predominantly in Europe compared two fixed doses of everolimus (1. However, significantly worse renal function in both everolimus groups led to a protocol revision at 12 months with reduction in the target trough cyclosporine levels to 50ͷ5 ng/mL. A similar trial conducted predominantly in North America with the same composite endpoint at 36 months and the same protocol amendment showed that all three groups were similarly efficacious but creatinine clearance was lower at 12 and 36 months in the everolimus groups. Sirolimus has also been evaluated in combination with tacrolimus after an initial report suggesting that the theoretical misgivings about the combination are not seen in clinical practice. Both arms of the study received corticosteroids and sirolimus was dosed to achieve blood levels of 4ͱ2 ng/mL. At 1 year renal function was superior in the tacrolimus arm and patients receiving sirolimus had a higher incidence of study drug discontinuation (26. Sirolimus was given according to a fixed-dose regimen of 2 mg for 28 days and 1 mg thereafter. Both study groups received steroids initially but these were tapered and discontinued after day 90. Renal function at 6 months, the primary end-point, was similarly good in the two study groups. Acute rejection and graft survival were similar in both groups, but premature withdrawal due to adverse events was twice as high in the sirolimus/tacrolimus arm (15. Everolimus plus tacrolimus has also been evaluated for use as primary immunosuppression after renal transplantation. The first prospective study to evaluate this combination was a 6-month multicenter study performed in the United States. Ninety-two de novo renal transplant recipients were randomized to receive everolimus, steroids, and basiliximab together with either standard or low-exposure tacrolimus. The study failed to demonstrate any benefit in the tacrolimus minimization group, possibly due to overlapping of achieved tacrolimus exposure in the two groups, but suggested that everolimus in combination with early tacrolimus minimization was associated with a low rejection rate, good graft survival and renal function, and an acceptable safety profile. Sirolimus was shown to provide sufficient immunosuppression during the maintenance phase, with superior calculated creatinine clearance compared with patients remaining on sirolimus and cyclosporine. Although the acute rejection rate was slightly higher in the no-cyclosporine group, this did not translate into poorer renal function. Late conversion to sirolimus is associated with three dominant side effects that might limit its usefulness as a maintenance agent, in addition to the other side effects that are well recognized with sirolimus (see later). First, more than half of patients in some studies experience a rash, either an acneiform rash or a dermatitis-like rash affecting the hands and, in particular, the fingers. Second, the period of conversion to sirolimus is associated with the development of mouth ulcers that, in most patients, resolve within 4 weeks. Finally, patients with suboptimal renal function, particularly patients with proteinuria, are prone to develop marked proteinuria after conversion (see later).
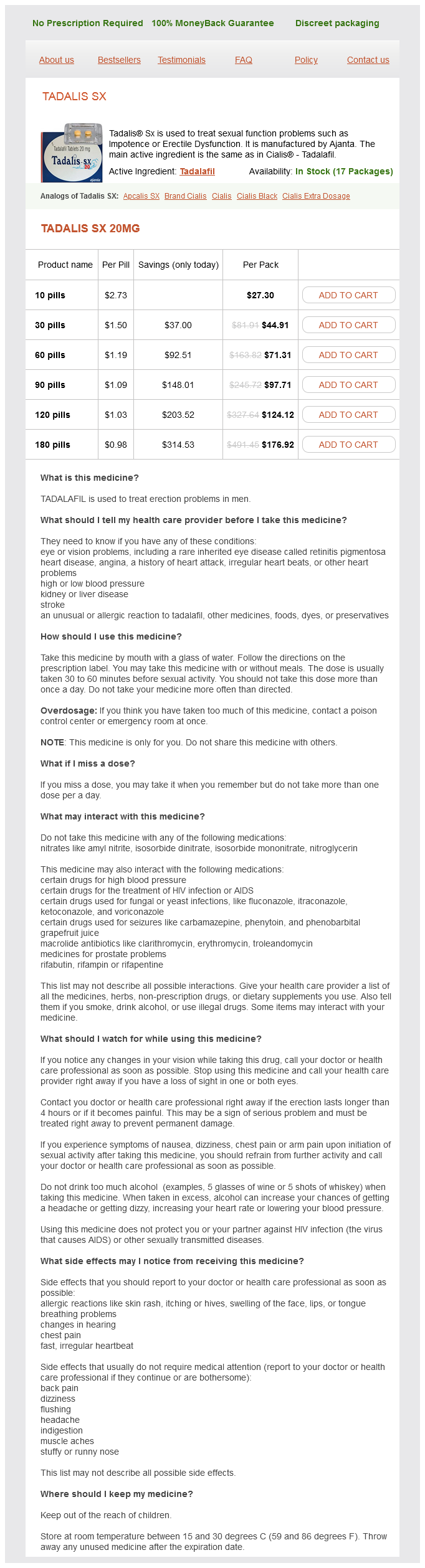
Tadalis SX Dosage and Price
Tadalis SX 20mg
- 10 pills - $27.30
- 30 pills - $44.91
- 60 pills - $71.31
- 90 pills - $97.71
- 120 pills - $124.12
- 180 pills - $176.92
In epidemics and localized outbreaks impotence over the counter buy tadalis sx pills in toronto, residual insecticide spraying of houses and the immediate area around the house is the most effective immediate control measure. Eliminating or treating the reservoir host Most success has been achieved where the domestic dog is the main reservoir, efforts being directed 76 Visceral leishmaniasis children. In areas where resistance is a problem, amphotericin B and miltefosine can be useful. Phlebotomous argentipes is the only known vector and is restricted to areas in and around the home. The elimination initiative has adopted five main strategies: × Early diagnosis and complete treatment of cases; × Integrated vector management; × Effective disease surveillance through passive and active case detection; × Social mobilization and partnership building at all levels; × Clinical and operational research as it is needed. The organisms in the host tissues are mainly found in reticuloendothelial cells in the skin, where, as amastigotes, they multiply by simple fission. Usually a papule develops at the site of infection, becomes a nodule and subsequently forms an ulcer with a central depression and raised indurated border. This may enlarge to a diameter of several centimetres and persist for months or years before eventually healing, leaving an atrophic scar. It is common to attach the terms Old World or New World depending on the region in which the infection is acquired. A single lesion gives rise to multiple diffuse soft fleshy nodules or plaques containing enormous numbers of amastigotes. There may be extensive depigmentation in the areas of affected skin, increasing the resemblance to leprosy. In endemic areas, the risk of mucosal disease following a primary cutaneous lesion is around 1ͱ0% within 1͵ years, although there are reports of incidence rates of up to 25%. The combination of scarring and signs of active inflammation is characteristic of the condition. The onset is usually a few years after resolution of the original cutaneous lesion, but may occur while the primary lesion is still present or decades later. Haematogenous and lymphatic dispersal results in spread of amastigotes from the skin to the naso-oropharyngeal mucosa. Granulomatous destructive lesions with chronic ulceration follow and secondary bacterial infection. Response to treatment may be problematic, with delayed healing and increased likelihood of recurrences. Cutaneous leishmaniasis 79 Investigations Cutaneous and diffuse cutaneous leishmaniasis Parasitological diagnosis is usually made by biopsy of the edge of the ulcer or other lesion. Other techniques that are sometimes used include needle aspirates and dermal scrapings. A new microcapillary culture technique using a monophasic medium is also used in some centres. With advances in other techniques for diagnosis, the leishmanin test is seldom used in clinical practice today. Management Before commencing treatment, the following issues should be considered: × the number, size, evolution and persistence of lesions; × the location of lesion(s). Treatment of cutaneous leishmaniasis Cosmetically unimportant lesions caused by nondestructive and non-metastasizing species usually heal spontaneously and therefore may not require active treatment. Local, topical and physical treatments Various local, physical and topical therapies are sometimes used, including: × × × × heat treatment or cryotherapy; topical amphotericin B (L. Leishmanin test (Montenegro test) this is a skin test using a killed promastigote suspension as antigen (area and species specific), injected intradermally and read at 48 h, like the tuberculin test. In endemic areas a high proportion of the population will be leishmanin test-positive and may also have healed scars. A strongly positive test may be Treatment with paromomycin may result initially in increased ulceration, so it is best avoided for ulcers on the face. Oral treatment the following oral agents can be used for treating relatively benign cosmetically unimportant lesions. Adequate systemic treatment of cutaneous lesions is assumed (but not proven) to decrease the risk of mucosal disease. Treatment with 5 mg/ kg/day achieved a cure rate of 75% with a mean time to healing of 7. Several trials show that miltefosine cure rate is low for certain Leishmania species and inferior to SbV. However, two recent trials showed higher miltefosine cure rates compared with SbV for L. Short-course pentamidine has been shown to be effective in Colombia where disease is predominantly caused by the Viannia subgenus. In the Middle East it is customary for mothers to expose cosmetically unimportant areas of their infants to sandfly bites or to deliberately inoculate them with infected material to render the child immune to that species. There has also been some interesting work recently on the development of vaccines against sandfly saliva. Since then, advances in human understanding of the disease have been major catalysts in the development of modern medicine. As we approach the third decade of the 21st century, knowledge of the full genome of M. Growth is slow, the generation time being 15Ͳ0 h, as compared to well under 1 h for most common bacterial pathogens. Visible growth of yellow colonies in culture, on egg-based solid Lò·¥®steinΊensen medium, takes between 4 and 12 weeks.