Tizanidine
General Information about Tizanidine
While Zanaflex can provide reduction from spasticity and different circumstances, it could be very important use it with warning and underneath the steering of a healthcare skilled. It could cause drowsiness and dizziness, which can be probably harmful when participating in actions that require alertness, similar to driving. It can also interact with other medications, so it is essential to inform your physician about some other drugs you're taking before starting Zanaflex.
Tizanidine, generally known by its brand name Zanaflex, is a medicine used to treat spasticity in muscle tissue. Spasticity is a condition characterized by the tightness and stiffness of muscles, often brought on by neurological issues such as a quantity of sclerosis, spinal cord damage, or stroke.
Zanaflex belongs to a class of medication generally recognized as muscle relaxers, which work by quickly relaxing the muscle tone in tense and rigid muscle tissue. It is on the market as a tablet or a capsule, and is normally taken by mouth every 6 to 8 hours, with a maximum daily dose of 36 mg.
Zanaflex has been proven to be effective in managing spasticity and improving quality of life for these living with situations such as multiple sclerosis, spinal twine damage, and stroke. However, as with any medicine, you will need to use it as prescribed and comply with up with your physician frequently to ensure its effectiveness and safety.
In addition to its use in treating spasticity, Zanaflex has also been found to be effective in treating chronic tension headaches and migraine complications. By relaxing the tense muscular tissues in the head and neck, it might possibly help to alleviate the pain and discomfort associated with these kind of complications.
Zanaflex works by blocking nerve impulses, which prevents the muscle tissue from contracting and ends in relaxation. It additionally will increase the manufacturing of a chemical known as gamma-Aminobutyric acid (GABA) within the brain, which additional helps to cut back muscle exercise and stiffness. This twin mechanism of action makes Zanaflex an efficient treatment choice for spasticity.
Zanaflex may have unwanted effects corresponding to dry mouth, weakness, and fatigue. However, these side effects are normally mild and subside with continued use of the treatment. If you experience any extreme side effects, it is necessary to search medical consideration immediately.
One of the key benefits of Zanaflex is its capacity to focus on and relieve specific muscles affected by spasticity. Unlike other muscle relaxers that may cause widespread drowsiness and sedation, Zanaflex is more selective in its action, permitting people to hold up their every day activities with minimal disruption.
In conclusion, Tizanidine, or Zanaflex, is a useful treatment for the remedy of spasticity and different associated situations. By quickly stress-free muscle tone and targeting particular muscles, it might possibly present relief and improve mobility for people residing with these situations. With correct utilization and careful monitoring, Zanaflex might help individuals lead a extra snug and active life.
Appropriate laboratory diagnosis may include the use of direct microscopy and selective culture media to recover and identify the suspected causative agent spasms in colon cheap 2 mg tizanidine overnight delivery. What are the key elements to obtain in the history when interviewing a patient with diarrheal illness How is the workup of diarrhea in an immunocompromised patient different from that in a healthy host Which parasite may cause a bloody diarrhea and disseminated infection sometimes resulting in liver abscesses What are some life-threatening complications associated with bacterial diarrheal infections Clinical Infectious Diseases: an Official Publication of the Infectious Diseases Society of America,32,1706. Clinical Infectious Diseases: an Official Publication of the Infectious Diseases Society of America,32,1201. OutbreakofEscherichia coli O157-H7 infection associated with eating fresh cheese curds-Wisconsin,June1998. Clinical Infectious Diseases: an Official Publication of the Infectious Diseases Society of America,32(3),331351. Clinical Infectious Diseases: an Official Publication of the Infectious Diseases Society of America,33,110. Clinical Infectious Diseases: an Official Publication of the Infectious Diseases Society of America,30(3),515. Guidelines for the control of shigellosis including epidemics due to Shigella dysenteriae type 1 (pp. Clinical Infectious Diseases: an Official Publication of the Infectious Diseases Society of America,45,302. For each pathogen associated with meningitis, correlate one host-related risk factor and one virulence-related factor. Identify the common bacterial, fungal, and parasitic pathogens associated with brain abscesses. List fungi that typically cause meningitis and compare the virulence and host factors of two fungi that typically cause intracerebral lesions. Case in Point A 3-year-old boy with a recent history of acute otitis media was brought to the emergency department; on examination, he was found to be febrile with a temperature of 103° F (39. Examination of a complete blood count showed leukocytosis with a total leukocyte count of 21,000/µL with a left shift. These infections may be caused by bacteria, viruses, fungi, spirochetes, or parasites. Since the introduction of vaccination against Haemophilus influenzae type b in the 1980s, there has been a dramatic reduction in the incidence of meningitis caused by this organism. In the United States, Streptococcus pneumoniae has become the leading cause of bacterial meningitis among children less than 5 years of age. Pneumococci cause over 50% of all cases of bacterial meningitis in the United States. Before routine use of the pneumococcal conjugate vaccine, children less than 1 year of age had the highest rates of pneumococcal meningitis, approximately 10 cases per 100,000 population. The incidence of meningococcal meningitis is higher in sub-Saharan Africa (the so-called meningitis belt), extending from Senegal in the west to Ethiopia in the east. The brain and spinal cord are protected by the skull and vertebral column respectively and three layers of meninges-the dura, arachnoid, and pia mater. The dura mater is a thick, fibrous, white membrane that is firmly adherent to the overlying skull. Bacteria Involving the Central Nervous System Bacterial Meningitis Related to Age Neonates (<1 month) Gram-negative bacilli (Escherichia coli, Klebsiella spp. Host risk factors that predispose to infection include extremes of age; nutritional and immunologic status; comorbidities, such as alcoholism, diabetes mellitus, malignancy, renal failure, and head trauma; and neurosurgical procedures. Structural components of the organism, such as capsule, pili, and fimbriae, which mediate adherence to respiratory tract epithelial cells, play an important role in meningeal infection. Additionally, the bacterial capsule can resist neutrophil phagocytosis and complement-mediated bactericidal activity, thus enhancing survival in the bloodstream. Host defenses include the presence of mucosal immunity mediated via immunoglobulin A (IgA) antibody, complement activation, and the presence of organism-specific antibodies. Central Nervous System Infections Meningitis Acute meningitis is commonly caused by bacteria. Patients with acute meningitis usually have fever, headache, vomiting, photophobia, and altered mental status. In infants and children, irritability, restlessness, and poor feeding may be the only signs of meningitis. Bacterial Meningitis the likely causative agents of bacterial meningitis depend on the age of the patient (Box 35. Bacterial infection of the leptomeningeal space can occur from a distant focus via the bloodstream or by direct invasion from a contiguous focus of infection. Most commonly, infection or colonization of the respiratory tract is followed by invasion of blood from a respiratory focus and seeding of the meninges. Patients with sickle cell anemia, those who have undergone splenectomy or have asplenia, and those with malignancy, malnutrition, and chronic renal or liver disease are more likely to develop serious pneumococcal disease.
With the emergence of biofilm-associated diseases muscle relaxant in india tizanidine 2 mg order otc, considerable diagnostic problems exist for the clinical laboratory. In general, these problems can be classified into five categories: (1) false-negative cultures, (2) viable but nonculturable organisms, (3) underestimated or low colony count, (4) inappropriate specimen, and (5) loss of or decreased antimicrobial susceptibility. Studies have shown that cultures detect less than 10% of molecularly detectable methicillin-resistant staphylococci from vaginal specimens of biofilm communities. Some persister cells found in biofilms are viable but nonculturable bacteria, for reasons not fully understood. Organisms upregulated to the biofilm phenotype may have significantly altered biochemical profiles. When bacteria are recovered from a biofilm, often aggregates representing 105 cells/mL or more can be recognized as a single colony on a bacteriologic plate. Ignoring the presence of a biofilm can result in the collection of inappropriate specimens. Until the true nature of biofilms was understood and the importance of stress realized, most organisms could be considered attached (as in arterial line sepsis) on the outside of the inserted line. It is now apparent that bacteria preferentially select a luminal environment, often devoid of immunologic components. The only technique that has been associated with the recovery of organisms from extraluminal sources is the rolling (Maki) technique. This is a semiquantitative culture technique in which a 4-cm length of the catheter is rolled over the surface of an agar plate. Recovery of more than 15 colonies along with the same organism isolated from peripheral blood, with clinical signs and symptoms with no other recognized source of the organism, is suggestive of a catheter-related bloodstream infection. Currently, it is recognized that line sepsis is often intraluminal and that procedures need to be developed to recover luminal organisms attached as biofilms. Microbiology laboratories historically have performed antimicrobial susceptibility testing on organisms in the plank-tonic phenotype state in pure culture. This is associated with expressed gene markers and detection of drug resistance of an organism. In contrast, a community of cells loses its susceptibility as a phenotypic expression of that community. It is now well accepted that the minimum inhibitory concentration against a free-floating planktonic isolate will increase by 10- to 1000-fold when measured in the biofilm community. Drug resistance is amplified even more when multiple species are present, particularly with the accommodation of prokaryotic and eukaryotic cells. Consequently, bacterial isolates that appear sensitive in vitro will not respond to therapy or may relapse several months later because of the existence of biofilms in vivo. Detection of Biofilms the direct detection of biofilms on biopsied tissue such as the middle ear mucosa in people with chronic otitis media and on tissue or implants removed from diseased areas of the body is now possible. Although not performed routinely in clinical microbiology laboratories, these techniques provide valuable information about the role of biofilms in the disease process and what interventions may be possible to eliminate or prevent biofilms. Techniques for the evaluation of biofilm formation potential by bacteria have become more available in the last decade. These techniques add to our knowledge about the organisms that form biofilms and allow us to study how to eliminate them or prevent them from initiating biofilm formation. These methods provide detailed information, but they are laborious and time-consuming and thus do not lend themselves to large-scale screening assays. Therefore more rapid and less laborious methods have been devised to evaluate the potential for bacteria to form biofilms in tubes or microtiter wells. One such rapid method is a colorimetric assay in which a suspension of bacteria is prepared in a culture medium that is then placed in the wells of a microtiter plate or tubes. After incubation for 24 to 48 hours, the medium is removed from the wells and each well is rinsed several times to remove any bacteria not adhering to the sides. After a specified time, the wells are rinsed several times, and then the wells are evaluated with a spectrophotometer for the presence of stain. The ability of the bacteria to form biofilms is determined by the degree of stain adhering to the bacteria in the wells or tubes after rinsing. Techniques such as this allow study of the effects an antimicrobial agent might have on the formation or inhibition of the growth of a biofilm. In a similar method, bacteria are incubated in the presence of silicone disks, and the ability of the bacteria to adhere to the disks is determined by a colorimetric method. Enhancement of this technique by the use of preferential stains allows the determination of live and dead bacteria within the biofilm. The main problem with assays for the detection of biofilms or the potential of bacteria to form biofilms is the lack of standardization; therefore analysis of data from these studies needs to include a critical assessment of the methods used. Potential Interventions Because of the physical and chemical properties of biofilms, traditional antimicrobial therapy based on planktonic susceptibility profiles will have a limited effect on resilient multispecies biofilms. Therapeutic modalities are focusing on multiple interventions, recognizing that the properties of biofilms are similar to those of organic polymers, not planktonic microbes. In theory, disk diffusion antimicrobial testing should be related to antimicrobial resistance testing, and biofilm testing or colonization resistance can be associated with antimicrobial susceptibility testing. Disruption of the biofilm and its aggregates could have clinical consequences detrimental to the patient. Therefore the focus on reducing the bioburden and preventing attachment in the first place should continue. In addressing biofilm eradication, combinations of strategies have been used: (1) mechanical disruption or removal (sonication), (2) immune modulation, and (3) antimicrobial agents (silver and tobramycin). The effects of various antimicrobials on the elimination or reduction in the number of organisms in a biofilm or the prevention of biofilms have been studied.
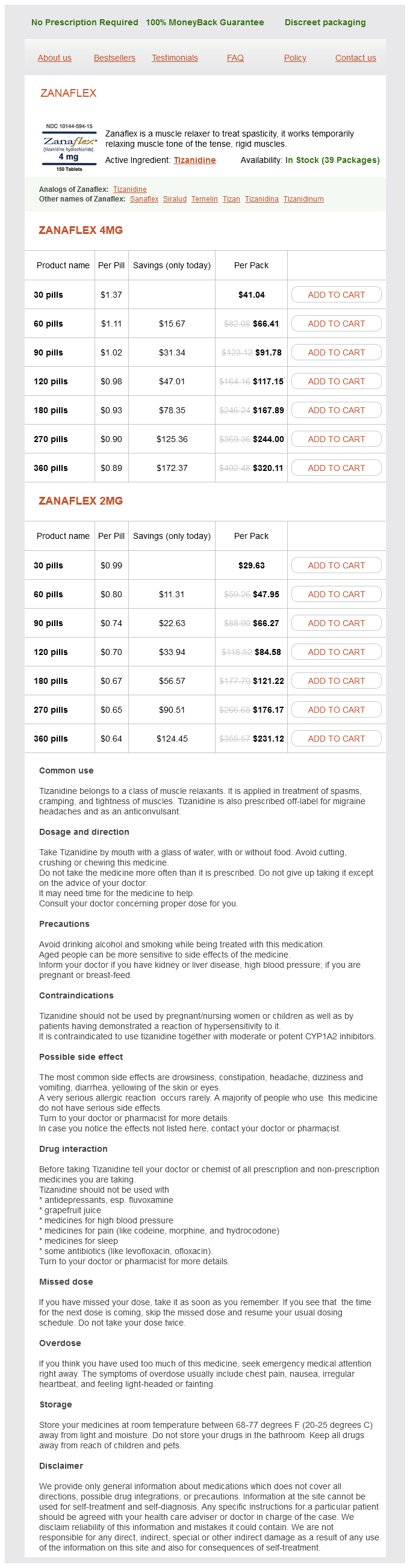
Tizanidine Dosage and Price
Zanaflex 4mg
- 30 pills - $41.04
- 60 pills - $66.41
- 90 pills - $91.78
- 120 pills - $117.15
- 180 pills - $167.89
- 270 pills - $244.00
- 360 pills - $320.11
Zanaflex 2mg
- 30 pills - $29.63
- 60 pills - $47.95
- 90 pills - $66.27
- 120 pills - $84.58
- 180 pills - $121.22
- 270 pills - $176.17
- 360 pills - $231.12
In between is a situation where many genes act in combination with one another spasms parvon plus 4 mg tizanidine order otc, and with the environment, to cause the illness. Our genes, and traits driven by those genes, are passed on according to biological laws. These laws have a mathematical description that predicts the pattern of illness in families. It is, therefore, possible to use family, twin, and adoption studies to test whether one, several, or very many genes are the cause of schizophrenia. Sadly, attempts to fit mathematical genetic models to schizophrenia family data have not given clear results. Some studies support the idea of a single responsible gene in some families, but most others find that many genes would be needed to explain the pattern of transmission seen in most families with schizophrenia. We call these simple or Mendelian disorders, so-named because they are inherited in the same predictable way as the traits of the pea plants studied by Gregor Mendel in the 1800s. The pattern of family transmission of these and many other disorders closely follows the laws of single-gene inheritance. In contrast, the exact mode of inheritance of schizophrenia is unknown and does not conform to the laws of inheritance for single-gene disorders. There are a number of ways in which genes can cause or influence traits and diseases. The confluence of enough risk genes plus environmental factors in any given individual can be random, and lead to an unpredictable pattern of disease in the family. A family with many affected ancestors will have a higher probability than other families of having affected descendants, but even in heavily affected families, many individuals will be unaffected, or just partly affected. Similarly, the disease can emerge in descendants of other families even where there is not a strong family history of the disease. Most families affected by schizophrenia do not show a pattern of inheritance consistent with either a dominant or recessive gene, but rather a multifactorial polygenic pattern. Note: squares represent males, circles represent females; black shading indicates presence of a disease, white shading indicates absence of a disease, and partial shading indicates a partial form of the disorder, such as a spectrum disorder; older generations are at the top of each pedigree. This type of study is usually done by comparing a large group of biologically unrelated people with schizophrenia against a separate group of people without schizophrenia, but who are similar in all other regards to those with schizophrenia. A simple statistical test determines if any genetic variant is reliably more common in individuals with schizophrenia. If we find such a difference, we refer to the variant that is more common among the affected individuals as a risk variant. In the context of the family, association studies look for a higher rate of individuals with schizophrenia receiving the risk variant of the gene from his or her parent, even when both the risk and normal variants of the gene were present in the parents and had an equal chance of being inherited. After decades of hard work, it is rewarding to have finally found a large number (~250) of places in the genome where individual differences are tied to risk for the disorder. So if the overall population risk for schizophrenia is approximately 1%, having any given riskgene variant may bump that risk only to 1. On its own, no single riskgene variant is enough to cause schizophrenia, and in fact, each of us is carrying many risk variants for the disorder. It is only in combination with many other risk variants, and environmental risk factors that these genes bring about the disorder. Scientists are still working hard to figure out why there is such a large gap between the 6085% of schizophrenia risk that is heritable and the 20% of risk that has been found for the top genes. Also, the exact regions of the genome that are inserted or deleted in schizophrenia differ widely among affected individuals, suggesting that there are, again, variable paths from 44 Chapter 6 · Is schizophrenia inherited Apart from being quite rare, these large insertions and deletions do not, on their own, account for a large amount of risk in the population. However, for individuals who have, for example, a deletion of a large part of their 22nd chromosome or duplication of a large part of their 16th chromosome, their risk is dramatically increased (anywhere from two to ten times higher than the risk to the general population). It has been surprising that the strongest biological system associated with genetic risk for schizophrenia is the immune system, and this is changing our understanding of what immune system genes do. Aside from coordinating immune system responses, for example, C4A has recently been found to play a role in the way brain cells, or neurons, develop in early life, and how they mature. Apart from the immune system and neuron development, risk genes for schizophrenia also impact the biology of dopamine neurons, which is important because all medications that help with the positive symptoms of schizophrenia also interact with dopamine neurons. In addition, schizophrenia-risk genes impact a process called cell adhesion, which governs how cells make connections with other cells. Furthermore, schizophrenia-risk genes often are involved in calcium transport, a process by which this vital element is moved in and out of cells to regulate their electrical energy. So although the genes for schizophrenia are distributed widely across the genome, they have common threads at the level of biology. In fact, recent research shows that virtually every large duplication or deletion that increases the risk for an autism spectrum disorder or intellectual disability also increases the risk for schizophrenia, and vice versa. Genetic heterogeneity the wide variety of genetic results for schizophrenia that have emerged in the past 15 years sometimes gives scientists pause, as it abolishes all hope that there will be a single, simple explanation for the disorder. Instead, the data show that many cases of schizophrenia are due to individual or combinations of rare variants that are exclusive to a small number of families or individuals. In the best-case scenario (which we have already ruled out), schizophrenia would be caused by one factor, either genetic or environmental. This would simplify diagnosis and dictate a straightforward intervention to offset that genetic (or environmental) effect. In the worst case scenario (the Anna Karenina scenario), each affected individual has his or her own constellation of risk factors, which makes diagnosis, treatment, and even research much more difficult. Yet, as described above, these studies have limitations that may prevent us from detecting all of the associated genes or identifying the truly responsible variation at each site in the genome. New technologies will need to be brought to bear on schizophrenia to hasten the rate of risk-gene discovery.