Toradol
General Information about Toradol
Toradol, additionally known by its generic name ketorolac, is a nonsteroidal anti-inflammatory drug (NSAID) that's primarily used for the treatment of average to extreme ache. It is usually prescribed for the short-term reduction of ache following surgical procedure or from conditions similar to kidney stones, migraine complications, and osteoarthritis.
Another benefit of Toradol is its short-term use. It is often prescribed for not more than 5 days, reducing the danger of long-term unwanted aspect effects corresponding to gastrointestinal bleeding and kidney damage. This additionally helps to prevent sufferers from turning into dependent on the medication for pain administration.
One of the primary benefits of Toradol is its ability to supply strong pain reduction. It works by inhibiting the production of prostaglandins, that are chemicals that trigger inflammation and contribute to pain. This makes it a extremely efficient option for treating average to extreme pain that isn't responding to over-the-counter pain relievers.
It can be necessary to note that Toradol should not be utilized in sure situations, corresponding to by individuals with a history of allergic reactions to aspirin or different NSAIDs, these with a history of bleeding issues, and pregnant girls. It can also interact with different medications, so it is crucial for sufferers to disclose all medications they are taking to their healthcare supplier.
First approved by the United States Food and Drug Administration (FDA) in 1989, Toradol is on the market in both oral and injectable types. It is commonly seen as a preferable various to opioids due to its decrease potential for habit and abuse. However, it is necessary to note that like all medicines, Toradol does come with its own set of risks and side effects.
Despite its effectiveness, Toradol does come with potential unwanted aspect effects. These include nausea, vomiting, abdomen ache, dizziness, and drowsiness. In uncommon instances, it could also lead to more severe circumstances such as heart attack, stroke, or liver harm. For this purpose, it is important for patients to discuss their medical history and any other drugs they're taking with their doctor before starting Toradol.
Toradol is often used in hospital settings after surgical procedures or procedures, as it offers quick and efficient ache relief. In addition, it might be administered through an intramuscular or intravenous injection, making it a super option for sufferers who're unable to take treatment orally.
In conclusion, Toradol is a strong and efficient medicine for the short-term therapy of moderate to severe pain. Its use is proscribed to 5 days or less, reducing the danger of long-term unwanted facet effects. However, like all medicines, it is necessary for patients to tell their physician about any medical conditions or other medications they're taking to make sure safe and efficient use of Toradol.
If so pain treatment with antidepressants toradol 10 mg purchase without a prescription, the marked airway obstruction in the absence of a history of airway disease makes other causes unlikely. There are no investigations which are helpful in making the diagnosis, and the diagnosis is confirmed by the response to appropriate treatment with adrenaline and intravenous fluids. The treatment is the same, namely cardiorespiratory support until the effect wears off, so a lack of certainty in the final diagnosis is not critical. However, they are an allergic response to foreign biological material, and anaphylaxis can develop. Symptoms usually occur soon after the transfusion begins, and the cause is therefore obvious. The diagnosis of the underlying cause of the collapse may not be immediately obvious. As has been emphasised in this section, resuscitation must begin even if the diagnosis is unclear. The differential diagnosis is not extensive, but in this clinical situation rational thought often deserts us. Prompt introduction of appropriate resuscitation may make the difference between the woman living or dying and give the time necessary to make the correct diagnosis. Progressively the woman complains of feeling short of breath or finding it difficult to breathe and becomes more anxious and dyspnoeic before proceeding rapidly to respiratory arrest. The close correlation between the administration of local anaesthetic and the progressive respiratory distress in the absence of circulatory disturbance confirms the diagnosis. A more truly toxic effect occurs with intravascular injection of a local anaesthetic agent, again typically with the insertion or topping up of an epidural block. Pregnant women appear to be more susceptible because of increased vascularity in the vessels around the epidural space and the increased pressures in the subarachnoid and epidural spaces that occur with contractions. Signs and symptoms usually occur within minutes of the injection of local anaesthetic. Respiratory paralysis follows, and cardiac arrest may occur as a result of anoxia and/or myocardial depression. However, collapse in the puerperium is more common, principally due to postpartum haemorrhage. The symptoms and signs of hypovolaemia (shock) may develop rapidly with progressive loss of consciousness as the blood pressure falls. It should be remembered that in severe haemorrhage there may be multiple factors contributing to the blood loss. For example, blood loss from perineal trauma may add to the bleeding from an atonic uterus, which can be aggravated by a developing coagulopathy due to consumption of clotting factors. Blood samples for full blood count, group and screen, coagulation screen, and renal and liver function tests should be taken right after inserting large bore cannulas. Once again it is important to emphasise that resuscitation must be proceeding hand in hand with diagnosis. The causes of collapse are listed in Box 1 and will be covered in this sequence in this chapter. If significant bleeding continues despite the application of pressure, the cervix must be examined for lacerations. In a collapsed woman this should be done under anaesthesia together with exploration of the uterine cavity. Uterine cause If vaginal and cervical traumas are excluded by examination, then either retained placenta or products of conception or a poorly retracted lower segment are the likely causes of the bleeding. Gentle exploration of the uterine cavity digitally or using a large, blunt curette will allow the removal of any remaining tissue. Great care must be taken in these circumstances because of the ease with which the uterus can be perforated. If no tissue is detected it is likely that the lower segment is not retracting, and this is usually seen when the placenta has been implanted in the lower segment. Delayed collapse (more than 24 h after delivery and less than 6 weeks postpartum) Haemorrhage Eclampsia Infection/sepsis Pulmonary embolus Myocardial infarction Coagulopathy In most cases of postpartum haemorrhage sufficient to cause maternal collapse, coagulopathy will contribute to the blood loss. This is most often a consumptive coagulopathy due to depletion of clotting factors with excessive blood loss. Alternatively, it may be associated with sepsis or one of the coagulopathic conditions peculiar to pregnancy (pre-eclampsia, abruption, amniotic fluid embolism, intrauterine fetal death). Repeated blood testing will be necessary to monitor blood and blood product replacement during resuscitation. Input from a haematologist is required to expedite the testing, interpreting the results, and procuring replacement factors. In general, coagulopathy due to consumption is more readily corrected (once bleeding is arrested) than that due to a coagulopathic condition of pregnancy. The causes of postpartum haemorrhage can be classified as the four Ts: Tone or lack of it (uterine atony) Trauma (vaginal, cervical, uterine) Tissue (retained products of conception or blood clot) Thrombin or lack of it (coagulopathy) Blood loss Atonic uterus Uterine atony is more likely and should be anticipated if the labour has been prolonged, augmented, or the delivery assisted by forceps or vacuum. Bleeding will continue while the uterus remains atonic, and this must be corrected with oxytocics and abdominal or bimanual massage of the uterus. The contraction of the uterus must be palpated frequently to assess the effects of the measures taken. If the uterus fails to respond, rupture of the uterus, although rare, should be considered.
The distal part of the stomach is made up of the body and the pyloric antrum pain treatment for arthritis in dogs 10 mg toradol purchase fast delivery, which are defined on the anterior aspect by the left hepatic lobe. The muscular opening into the duodenum is the pyloric orifice, which is in direct contact with the head of the pancreas. The small intestine is subdivided into the duodenum, which is about 30 cm long, and the jejunum plus ileum, which altogether measure approximately 1. The duodenum is a C-shaped arc (slightly more than a semicircle) that encloses the head of the pancreas, only partially covered by peritoneum. The inferior duodenal segment, situated about two fingerbreadths inferior to the mesenteric root and caudad of the pancreas, crosses anterior to the vena cava and the aorta. Cross-sectional views of the superior mesenteric artery and vein can be demonstrated anterior to the intestine. The retroperitoneal duodenum continues as an intraperitoneal organ at the level of the mesenteric root slightly left of the aorta. The jejunum and ileum are attached to the posterior abdominal wall by the fan-shaped folds of the peritoneum known as the mesentery proper; most of the coils of the small intestine are found in the left upper (jejunum) and lower (ileum) quadrant. The colon is about 120 cm long and runs along the margins of the intraperitoneal cavity. The cecum is situated anterior to the psoas major muscle in the right lower quadrant. The ascending colon parallels the right lateral abdominal wall and its superior segment is 261 Gastrointestinal Tract 7 Gastrointestinal Tract 7 Gastrointestinal Tract anterior to the inferolateral part of the right kidney. The hepatic flexure comprises the terminal part of the ascending colon and the commencement of the transverse colon; usually, the convex part of this flexure hugs the gallbladder and the lower right margin of the liver, but as a variant it may dome up far superior and may even be situated between the lower right thoracic wall and the right hepatic lobe (so-called Chilaiditi syndrome). The transverse colon touches the anterior abdominal wall and traverses the upper abdomen from right to left; elongated variants may have a drooping center section reaching all the way into the pelvis. The splenic flexure connects the transverse and descending colon, its convex aspect being inferior to the spleen. The proximal part of the descending colon is anterior and lateral to the left kidney. The S-shaped sigmoid colon forms a loop that, depending on its length, frames the roof of the urinary bladder more or less markedly. The rectum descends into the pelvis posterior to the bladder and terminates at the anus. The proximal part of the cervical esophagus posterior to the left lobe of the thyroid lends itself to sonographic study (7. The esophagocardial junction can be better evaluated by transabdominal ultrasound. With appropriate techniques all of the stomach and duodenum are accessible to sonographic study. Later, the postprandial ileum loops in the lower abdomen will also be fluid-filled and display vivid peristalsis. Sometimes an elongated sigmoid colon or drooping transverse colon may interfere and be the reason for misidentification. Almost always the colon will appear as a tube filled with a varying amount of feces and lacking peristalsis. Assessment of the intestinal wall and differentiation of its characteristic layered structure becomes possible only with high-frequency probes (5, 7, or 7. Gut Signature the normal "gut signature" is known as the "cockade," a term whose origins date back to Old French and refer to a rosette-shaped badge. In ultrasonography, the gut signature and its pathological variant the "target sign" have come to denote the round crosssectional view of the intestinal wall with its different layers. Thus, in the cross-sectional view the gut signature/target sign refers to the annular image of the layered intestinal wall and its center, while in the longitudinal view it refers to the parallel arrangement of adjacent intestinal segments with the lumen in between. A so-called physiological gut signature refers to a lumen that is normal for this segment, a wall structure with characteristic layering, welldefined wall thickness, and normal peristalsis. A so-called pathological gut signature is characterized by changes in the normal appearance of lumen, wall thickness, and/or peristalsis/pliability Table 7. Pathological wall changes may be circular or eccentric and focal, or they may be continuous or discontinuous along the longitudinal axis. Intussusception will be seen on ultrasound as the "target/doughnut sign" (cross-sectional view) or "pseudokidney sign" (longitudinal view). Detection of a gut signature calls for analysis of its ultrasound morphology, lumen, and peristalsis as well as of the surroundings and the intestinal segments upstream and downstream. Only all of these criteria together will permit typing and assessment with a clear-cut diagnosis in many cases. Specifying the position of a gut signature offers the first chance of defining the anatomical relations. It is important to recognize whether the pathology exhibits a fixed location or is mobile. Basically, the echogenicity of the gut signature may be normal, hypoechoic, or hyperechoic; since one is dealing with a layered anatomical structure, this criterion has to be applied to the predominant elements of the wall or should reflect the possible loss of layering. Measurement of the wall thickness has to account for the degree of filling and the functional state (contraction/dilatation) of the intestines, and also has to specify whether the wall is thickened or thinned out or whether its outline is interrupted or ill defined. The wall may display a normal layered structure or may be markedly layered, may demonstrate thickening of just one particular layer, may present with layer defects, or may have lost its layered structure altogether. In terms of length, short focal or extended lesions have to be differentiated from the diffuse changes in the intestinal wall. Assessment of the luminal surface of the bowel wall will be able to differentiate between normal as well as pathological circular folds and haustra (preserved or lost) and also focal polypoid/tumorous changes, ulcers, and other surface irregularities.
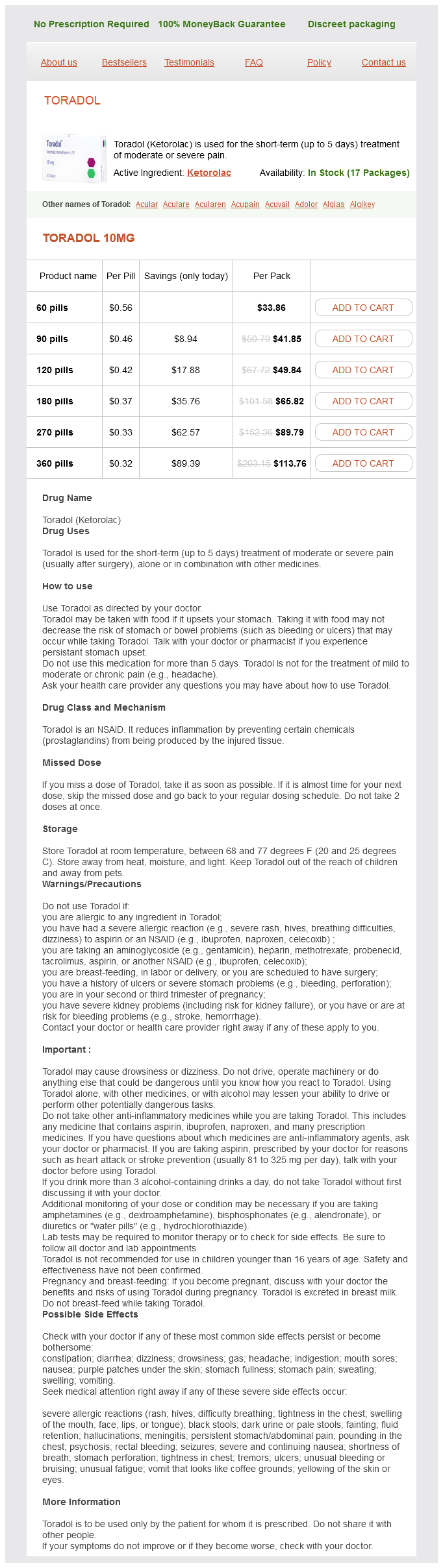
Toradol Dosage and Price
Toradol 10mg
- 60 pills - $33.86
- 90 pills - $41.85
- 120 pills - $49.84
- 180 pills - $65.82
- 270 pills - $89.79
- 360 pills - $113.76
However breakthrough pain treatment guidelines buy toradol amex, intracranial hemorrhage, cerebrovascular accidents, central venous thrombosis, and infarction have also been reported in the postpartum period and treatment for these conditions should be instituted in a timely manner to prevent permanent injury. Of concern in regard to late postpartum hypertension is a review that notes that many of these women were not given adequate discharge information, ignored premonitory signs, and/or presented to a primary care setting or an emergency room, often, after convulsing, where the treating physician was unfamiliar with the entity of postpartum preeclampsia. Efforts should also be directed at educating emergency physicians, primary care providers, and obstetricians to facilitate early recognition and treatment. Again, although under-studied in pregnant women, the routine use of nonsteroidal antiinflammatory agents for peripartum analgesia contributes, in our opinion, to some cases of significant hypertension in the postpartum period. These drugs are well known to elevate blood pressure in subgroups of nonpregnant patients at risk of hypertension. In some cases the blood pressure had normalized during gestation as a response to the physiologic vasodilatation that accompanies pregnancy. In most instances, the underlying disorder is essential hypertension; however, secondary causes should be considered when there are unusual features such as severe hypertension, hypokalemia, or symptoms suggestive of pheochromocytoma (see above). Primary aldosteronism in particular may first become apparent in the postpartum period, since antepartum blood pressure is often ameliorated by the antimineralocorticoid effects of progesterone during pregnancy. This is in contrast to the treatment philosophy for nonpregnant subjects where the primary concern is prevention of long-term cardiovascular morbidity and mortality. In the latter population blood pressure control is essential, the report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure4 recommending levels be maintained at 120 to 135 mm Hg systolic and 75 to 85 mm Hg diastolic, respectively. Management also includes aggressive attention to modifying other cardiovascular risk factors such as blood lipid and glucose levels, body weight, and smoking. For example, the level of blood pressure control tolerated during pregnancy may be higher, because the risk of exposure of the fetus to additional antihypertensive agents may outweigh the small benefits to the mother of tight control of her blood pressure during a 9-month period. Weight loss is not recommended during pregnancy, nor is vigorous cardiovascular exercise, which may reduce uteroplacental perfusion. Preconception Counseling Management ideally begins prior to conception, and includes ruling out and treating, if detected, secondary causes of hypertension. Women in whom hypertension is known to have been present for 5 years or more require careful evaluation for evidence of target organ damage, i. Pregnant women 35 years of age or older, particularly those with chronic illnesses, should be screened for occult coronary disease, and this is particularly important in women with type 1 diabetes with evidence of vascular complications. Risks posed by pregnancy are best discussed, and less emotionally evaluated, prior to conception. For example, women with stage 1 hypertension should be informed of the high likelihood of a favorable outcome, but should still be apprised of the risks of superimposed preeclampsia and the fetal complications associated with this disorder. This is also the best time to emphasize the importance of compliance and that frequent visits increase the likelihood of detecting preeclampsia and other complications well before they become life-threatening to mother or fetus. Women with small children, and those in the workforce, should be informed of the possibility that lifestyle adjustments will be necessary especially if complications develop. This will allow them to plan ahead for increased support both at home and at work. Finally, early planning, including the assembling of a multidisciplinary team consisting of obstetrician, maternal-fetal medicine specialists, and internists, optimizes the chances of a successful outcome in hypertensive women with other medical complications. A large World Health Organization sponsored multicenter trial conducted in the developing world suggested improved pregnancy outcomes associated with calcium supplementation only in women with low dietary calcium. Pharmacologic Management (see Chapter 19) Guidelines for antihypertensive therapy during gestation are less clear than those for nonpregnant hypertensives. For the latter, there are compelling data from large population studies to document the benefits of lowering blood pressure with medication, even in women with only mild hypertension. During pregnancy, however, though maternal safety remains the primary concern, there is also a desire to minimize exposure of the fetus to drugs, given their unknown long-term effects on growth and development. Therefore, permissible maternal blood pressure levels are analyzed in terms of preventing complications during the relatively short duration of the pregnancy, rather than the long-term cardiovascular risk. Another debatable issue is whether lowering blood pressure will prevent superimposed preeclampsia, but at present there is little or no convincing evidence to support this contention. In this respect, many caregivers will not treat with antihypertensive medications unless blood pressure exceeds these levels. This approach, however, has not been rigorously evaluated with randomized controlled trials. There is even less evidence when considering the subgroup of women with chronic hypertension. There are exceptions, however, including parenchymal renal disease, and evidence of target organ damage. Whether or not antihypertensive treatment of mild to moderate hypertension during pregnancy results in better fetal outcomes is not clear. There is some evidence that exercise is associated with a reduced risk of developing preeclampsia in previously normotensive women. Excessive weight gain, of course, is not advisable, but again, in contradistinction to therapy in nonpregnant populations, obese women should not be advised to lose weight during pregnancy. Dietary adjustments in pregnant women with chronic hypertension have not been extensively investigated. Salt restriction, an important component of management in nonpregnant populations, is less so in gestation, where extremely low sodium intakes (2 g NaCl) may even jeopardize the physiologic plasma volume expansion which normally occurs. In summary, the unknown but potential hazards of antihypertensive treatment during pregnancy are sufficient reasons for withholding drug treatment when mild hypertension is present, particularly during the initial trimester. As noted, many of these patients experience a physiologic decrease in blood pressure which on occasion reaches normotensive levels. Patients whose levels are equal to or greater than 160/100Â105 mm Hg, however, should be treated, while evidence of renal disease or end-organ damage requires initiation of treatment at lower levels (90 mm Hg). Specific Antihypertensives the pharmacology, safety, and efficacy of antihypertensive drugs in pregnancy are addressed in detail in Chapter 19. For most agents the evaluations are sporadic, and there are almost no follow-up data regarding the children exposed to the drug in utero.