Triamcinolone
General Information about Triamcinolone
One of the commonest uses of triamcinolone is within the remedy of skin conditions such as eczema, psoriasis, and dermatitis. These conditions are related to redness, swelling, and itching, which may be relieved by the anti-inflammatory properties of triamcinolone. The cream or ointment form of the treatment is often utilized topically to the affected space, providing focused reduction.
Triamcinolone shouldn't be used by individuals who've a identified allergic reaction to corticosteroids or any of the ingredients in the medicine. It can also be not really helpful for use in pregnant or breastfeeding girls except the potential benefits outweigh the risks. It is essential to tell a healthcare supplier of any other medicines you are taking to keep away from any potential drug interactions.
In conclusion, triamcinolone, marketed as Aristocort, is a robust corticosteroid medication that's used to treat a wide selection of inflammatory and immune-related circumstances. It offers aid from symptoms similar to swelling, redness, and itching and is out there in different varieties for various applications. While there are potential unwanted effects, triamcinolone is a trusted and efficient treatment prescribed by healthcare suppliers to alleviate discomfort and improve high quality of life.
Triamcinolone, more generally known by its model name Aristocort, is a synthetic glucocorticoid corticosteroid. It is used to treat a wide range of medical conditions characterised by irritation, extreme immune response, and swelling. Triamcinolone is a flexible medication that is available in varied forms, including creams, ointments, injections, and oral tablets.
The main mechanism of triamcinolone is to reduce inflammation by suppressing the physique's pure immune response. It works by binding to glucocorticoid receptors in the physique, thereby blocking the synthesis of inflammatory mediators. This ends in decreased irritation and pain within the affected space.
Triamcinolone can be used to treat allergies, significantly hay fever, which is caused by an overreaction of the immune system to allergens such as pollen and dust. The medicine could be prescribed to relieve the symptoms of allergy symptoms, such as sneezing, runny nostril, and itchy eyes.
As with any medicine, there could be potential side effects of using triamcinolone. The most typical side effects embrace skin irritation, burning or stinging sensation, dryness, and thinning of the pores and skin. Rarer side effects could embody headache, nausea, dizziness, and temper adjustments. It is essential to comply with the really helpful dosage and consult with a healthcare provider if any unwanted effects persist or worsen.
In addition to pores and skin situations and allergic reactions, triamcinolone can be prescribed for other situations, including asthma and rheumatoid arthritis. In these instances, the medicine is commonly given by way of injection to target specific areas of inflammation within the physique, such because the joints in rheumatoid arthritis or the airways in bronchial asthma.
The treatment of spondylotic cervical myelopathy by multiple subtotal vertebrectomy and fusion treatment shingles purchase 4 mg triamcinolone amex. An instrument to measure the health status in children with hydrocephalus: the Hydrocephalus Outcome Questionnaire. Craniosynostosis: an analysis of the timing, treatment, and complications in 164 consecutive patients. Quality of life in patients with glioblastoma multiforme participating in a randomized study of brachytherapy as a boost treatment. Normative sample of an instrument for tracking functional independence in children. The Sickness Impact Profile: development and final revision of a health status measure. The development of a patientcompleted index of distress from the Nottingham health profile: a new measure for use in cost-utility studies. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. Duplex venous scanning for the prospective surveillance of perioperative venous thrombosis. International Study of Unruptured Intracranial Aneurysms Investigators [see comments] [published erratum appears in N Engl J Med. Risk factors for death or stroke after carotid endarterectomy: observations from the Ontario Carotid Endarterectomy Registry. Centralized databases available for describing primary brain tumor incidence, survival, and treatment: Central Brain Tumor Registry of the United States; Surveillance, Epidemiology, and End Results; and National Cancer Data Base. Correlation of neurosurgical subspecialization with outcomes in children with malignant brain tumors. Discrepancies in diagnoses of neuroepithelial neoplasms: the San Francisco Bay Area Adult Glioma Study. Issues of diagnostic review in brain tumor studies: from the Brain Tumor Epidemiology Consortium. Identifying patient preoperative risk factors and postoperative adverse events in administrative databases: results from the Department of Veterans Affairs National Surgical Quality Improvement Program. Surgery for primary supratentorial brain tumors in the United States, 1988 to 2000: the effect of provider caseload and centralization of care. Association of surgical specialty and processes of care with patient outcomes for carotid endarterectomy. Comparison of effect estimates from a meta-analysis of summary data from published studies and from a meta-analysis using individual patient data for ovarian cancer studies. Individual patient-versus group-level data meta-regressions for the investigation of treatment effect modifiers: ecological bias rears its ugly head. Issues in the selection of a summary statistic for metaanalysis of clinical trials with binary outcomes. Statistical methods for examining heterogeneity and combining results from several studies in metaanalysis. Do authors of review articles use systematic methods to identify, assess and synthesize information Comment on A comparison of methods to detect publication bias in meta-analysis by P. A systematic literature review to identify the best method for a single level anterior cervical interbody fusion. Preparing, maintaining, and disseminating systematic reviews of the effects of health care. EvidenceBased Medicine Working Group and the Cochrane Applicability Methods Working Group. How to use an article evaluating the clinical impact of a computer-based clinical decision support system. How to use an article measuring the effect of an intervention on surrogate end points. Rules of evidence and clinical recommendations on the use of antithrombotic agents. Spencer, and Nitin Tandon this introductory chapter has two components: an initial overview of the contents of the epilepsy section and a discussion of various controversial topics related to epilepsy that neurosurgeons, irrespective of their experience, face when caring for patients with epilepsy. The addition of new topics has also increased the comprehensive nature of the epilepsy section. Since publication of the previous edition, a number of techniques have begun to change epilepsy surgery, with more minimally invasive monitoring approaches and treatment options. These techniques are highlighted in this "Epilepsy" section, and their pros and cons are pointed out in the "Controversies in Epilepsy" section of this introductory chapter. Subsequently, chapters deal with radiosurgical treatment for epilepsy (Chapter 78) and electrical stimulation for epilepsy (Chapter 79). Part 1, "Basic Science of Epilepsy," focuses on electrophysiologic properties of the central nervous system (Chapter 58), animal models responsible for scientific advances (Chapter 59), and malformations of cortical development frequently observed in patients with epilepsy (Chapter 60). These basic sciences are directly relevant to epilepsy and for the practicing neurosurgeon. Part 2, "Approach to the Patient," deals with the clinical evaluation and monitoring.
Other features include disturbed body image medicine 9312 purchase 10 mg triamcinolone free shipping, heightened desire to lose more weight, and pervasive fear of fatness. Two months after the second surgery, the patient experienced significant weight gain and increased appetite. The dorsolateral prefrontal cortex may become excessively involved in inhibitory processes to dampen information processing through reward pathways. Serotonin might play a role in altered satiety, impulse control, and mood, whereas dopamine is implicated in motivation, executive functions, and the aberrant reward effects of food. Such disturbances in the modulation of reward and emotion may increase vulnerability to dysregulated appetitive behaviors. In addition, inhibitory projections from the medial prefrontal cortex/orbitofrontal cortex to the amygdala are indispensable for this extinction. In this regard, individuals suffering from eating disorders exhibit faster fear learning and heightened resistance to the extinction of conditioned responses. It remains unknown whether disturbances in neural circuits occur before or as a result of malnutrition. It has been proposed that structural and functional alterations in the insula and frontal cortex, including areas that contribute to reward and anxiety processing, such as orbitofrontal and cingulate regions, could predispose individuals to developing eating disorders and that the adaptive changes in these circuits may occur in response to malnutrition. Furthermore, most side effects are reversible and can be managed by adjustment of stimulation parameters. Two months after treatment, anorexic patients had gained between 17 and 44 pounds, and eight experienced significant improvements in obsessive-compulsive behaviors and symptoms of anxiety. Anterior capsulotomy is a stereotactic ablative procedure that involves ablation of the anterior limb of the internal capsule to disconnect the prefrontal cortex and subcortical nuclei (including the dorsomedial thalamus); it is a widely used psychosurgical procedure. Most affected patients exhibit relief of certain symptoms and improved cognitive function, without experiencing alterations in personality. Radiofrequency electrodes are used to create two ablative lesions by thermocoagulation at 80°C for 60 seconds. In our center, of the 150 patients who underwent capsulotomy during October 2005 to December 2013, 85% experienced an improvement in symptoms, and menstruation resumed in all affected women. A few patients (<5%) experience long-term side effects, including memory loss, fatigue, excessive weight gain, and personality changes. Axial view (A) and coronal view (B) of the nucleus accumbens after the implantation of deep brain stimulation electrodes (arrows). Cingulotomy is a relatively safe procedure, and the incidence of adverse events is lower than that with anterior capsulotomy. Immediate transient symptoms include headache, confusion, and urinary incontinence. These parallel symptoms indicate that there is a considerable overlap in reward system neurocircuitry between these psychiatric disorders and eating disorders. At our institution, 12 patients in whom bilateral anterior capsulotomy failed underwent additional anterior cingulotomy; this procedure resulted in further improvements in about half of these patients. Finally, patients or their representatives must be willing to give informed consent for treatment and any subsequent follow-up study. Patients younger than 14 years and those who refuse to sign the patient information and consent form should also be excluded. Therefore, more detailed preoperative screening examinations such as electrocardiography and appropriate blood tests. According to our experience, hypokalemia and hypoalbuminemia are the most common electrolyte disorders, which should be restored to normal conditions before surgery. Careful perioperative management is essential to avoid anesthetic complications as well. In our center, the rate of wound infections is about 2%, which is similar to that in other medical centers. Neuropsychological Complications Neuropsychological complications can be divided into shortterm and long-term complications. Short-term side effects include incontinence, disorientation, sleep disorders, and headache. A number of patients (8%) experience long-term side effects, including memory loss, fatigue, excessive weight gain, and personality changes. Bhatia and colleagues72 reviewed data from 191 patients who received a total of 330 electrode implants and found that the overall incidence of hardware-related problems was 4. Intraoperative Management Local anesthesia is recommended during the ablative procedure to avoid hypervolemia and excessive dilution of electrolytes. In view of the potential anesthetic complications, a thorough preoperative anesthetic assessment and evaluation is required. In addition, doses of most anesthetic drugs should be adjusted for weight, and during the operation, electrocardiographic changes and potassium levels should be monitored carefully to minimize the risk of arrhythmias. To avoid cerebrospinal fluid overflow during the operation, fibrin glue should be applied immediately after the dura is opened. Furthermore, a warm air blower is necessary during the operation to maintain normal body temperature. The operation should be completed in a timely manner, and appropriate soft mats should be applied to prevent bedsores. Functional neuroimaging studies are particularly useful for finding the mechanisms of disease development and possible target areas for further neurosurgical interventions.
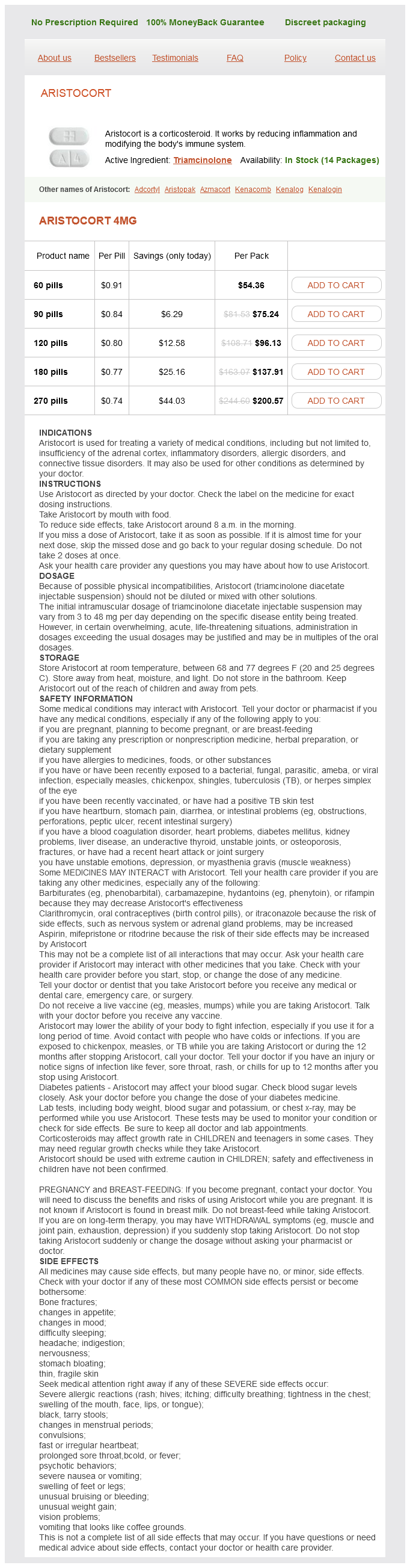
Triamcinolone Dosage and Price
Aristocort 4mg
- 60 pills - $54.36
- 90 pills - $75.24
- 120 pills - $96.13
- 180 pills - $137.91
- 270 pills - $200.57
Grids are flexible and may be shaped so that the edges of a grid conform to the cortical surface symptoms 6 weeks buy triamcinolone 4 mg on line. For instance, an interhemispheric grid may be curved to follow the convexity; furthermore, such grids may be designed to have electrode contacts on both faces, enabling monitoring of both hemispheres using the same single grid applied adjacent to the falx-one subdural and one epidural in location. Strip and grid placement not guided by a hypothesis is more likely to result in removal of hardware without resection. However, inadequate sampling due to insufficient electrode coverage may preclude accurate detection of the epileptogenic zone. Additional smaller grids or strips may be slid over the brain under the margins of the craniotomy without direct visualization, especially at orbitofrontal, inferior-temporal, and interhemispheric locations. When planning bur hole location, the surgeon must consider future skin incisions for craniotomy for grid placement or resections. A standard craniotomy is performed for grid placement on the basis of the desired cortical location for intracranial monitoring (Video 71-1). Gentle irrigation is injected under the subdural strip as it passes over the brain surface. Depth electrodes may be considered an alternative to subdural electrodes if severe adhesions between the dura and the brain are encountered. Care is taken to avoid injury or sacrifice of large draining cortical veins, and grid arrays may be cut or trimmed as needed. Slits should be made in the Silastic material of the grids to allow the hardware to conform better to the shape of the brain. Sutures are placed along the edges of the grid to secure it to the dura and avoid future displacement. Impedance may be measured to determine whether electrodes are making adequate contact with the cortex, and intraoperative recordings may be obtained from the electrodes before closure. Cables arising from the electrodes on grids and strips are carefully tagged in order to ensure correct identification of the source data. They are bundled together and tunneled subcutaneously to exit at a site several centimeters from the initial skin incision. Additional sutures are placed to securely anchor the cables to the skin and to incorporate a strain-relief connector. Following subdural grid placement, some groups reapproximate the dura with or without a pericranial autograft, especially when the number of electrodes placed is high,15,18 whereas others leave the dura open because of concerns about delayed cerebral edema and increased intracranial pressure. Similarly, the bone flap may be left off, left tethered with craniotomy plates without screws in the bone flap itself,20 or replaced in the standard fashion with plates and screws. Violence of seizure, age, and expectation for intracranial hypertension should be considered in the determination whether to replace the bone flap at the time of grid implantation. The risk of bone flap infection appears to be higher in cases in which the flap is left off than in those in which it is replaced, and this finding should be factored into the decision making. Color photographs and sketches may be made of the cortical surface before and after subdural strip and grid implantation to record the spatial relationship between the hardware and the cortical surface. Another approach is to take a high-resolution digital photograph of the exposed cortex before and after grid placement. Photographs capture individual details about local anatomy and gyral patterns that may be lost on more advanced imaging. The location of each electrode on the postimplantation photograph is plotted manually on the preimplantation photograph. Intraoperative photograph showing placement of subdural grid overlying the cortical surface. Coregistration of digital photography of the human cortex and cranial magnetic resonance imaging for visualization of subdural electrodes in epilepsy surgery. Intraoperative digital photograph is superimposed on a three-dimensional reconstructed magnetic resonance imaging brain surface model with the use of rendering software. Thus, at the time of surgical resection, the coregistered image provides the position of the electrode in exact relation to the epileptogenic focus and the cortical surface. For mapping the function of cortex just below the implanted grid, a stimulus is applied to one grid electrode while a distant grid electrode acts as the reference point. Stimulus intensity and other parameters may be altered with the goal of bringing about a functional change, such as speech arrest. Brain mapping using subdural grids is especially useful in pediatric patients, in whom certain functions, such as language, can be tested only in the awake state. Two-stage monitoring approaches are most common and consist of an initial subdural electrode implantation stage, a period of invasive monitoring, and then an electrode removal and resection stage. Subdural strips may be removed at the bedside with gentle traction and without reopening the incision. A three-stage approach that includes a middle stage for resection and reimplantation may be used in select pediatric patients with extratemporal or nonlesional epilepsy, previous surgical failure, suspected overlap of eloquent cortex and the epileptogenic zone, or areas of multiple seizure onset. Doses of antiepileptic drugs are gradually reduced in order to increase the likelihood of seizure occurrence. The duration of monitoring depends on the number of, localization of, and consistency between seizure semiology and the electrographic pattern. Not all hematomas are symptomatic, and collections of blood around or under subdural grids are commonly encountered at the time of grid removal in asymptomatic patients. Among 2356 patients undergoing strip and grid placement, intracranial hemorrhage occurred in 3. Earlier studies of grid placement reported higher rates of symptomatic subdural hematomas, with subdural hematomas occurring in up to 5.