Tulasi
General Information about Tulasi
Tulasi has also been found to have anti-stress and anti-depressant properties. It is believed to have a chilled effect on the mind and might help to reduce stress and nervousness. This is supported by its capability to manage the degrees of cortisol, the stress hormone, within the physique. Additionally, Tulasi can also assist to enhance temper and cognitive perform, making it a priceless herb for overall well-being.
In addition to its respiratory benefits, Tulasi has also been used to help general immunity. It is known to boost the immune system, making it easier for the body to battle off infections and diseases. This makes it an excellent herb to take throughout chilly and flu season.
The Tulsi plant is native to India and has a long historical past of use in Indian traditional medicine. It is considered a holy plant and is often worshiped in Hindu households. The plant is also identified for its sturdy and nice aroma, which is believed to have a relaxing effect on the thoughts and physique.
One of the main compounds present in Tulasi is eugenol, which has been proven to have bronchodilatory effects. This signifies that it helps to relax the airway muscle tissue and enhance respiratory. Tulasi also incorporates different beneficial compounds similar to camphene and cineole, which have anti-congestive properties and assist to clear mucus from the respiratory tract.
Tulasi may be consumed in various types, including as a tea, complement, or in fresh or dry form. It is also commonly used as an ingredient in cooking in Indian households. However, for max medicinal benefit, it is strongly recommended to take it in its purest kind, either in the type of a tea or supplement.
Tulasi is rich in antioxidants, nutritional vitamins, and minerals, making it a potent herb with a extensive range of medicinal advantages. It is particularly recognized for its capability to help the respiratory system. Tulasi has been historically used to deal with colds, coughs, and respiratory infections. The herb is known to have anti-inflammatory and antimicrobial properties, which help to soothe respiratory irritation and battle towards infections.
Overall, Tulasi is a robust herbal treatment that has been used for tons of of years for its numerous well being benefits. Its capability to help the respiratory system, increase immunity, and promote overall well-being makes it a priceless addition to any natural drugs cupboard. However, as with any herbal remedy, it is essential to seek the guidance of with a healthcare professional earlier than using Tulasi, particularly if you're pregnant, breastfeeding, or have any pre-existing medical circumstances.
Tulasi, also identified as Holy Basil, is a popular herbal remedy that has been used for centuries in conventional Ayurvedic medication. It is derived from the leaves of the Tulsi plant, which is considered a sacred plant in India and is often referred to as the “Queen of Herbs”. Tulasi is understood for its quite a few well being benefits, notably its capability to assist the respiratory system.
It is made from the leaves of Tulsi plant, also called Holy Basil, which is held in excessive esteem for its medicinal properties in conventional Ayurvedic medication.
Other organoarsenicals treatment kennel cough buy tulasi with amex, most notably lewisite (dichloro[2-chlorovinyl]arsine), were developed in the early 20th century as chemical warfare agents. Arsenic trioxide was reintroduced into the United States Pharmacopeia in 2000 as an orphan drug for the treatment of relapsed acute promyelocytic leukemia and is finding expanded use in experimental cancer treatment protocols. Melarsoprol, another trivalent arsenical, is used in the treatment of advanced African trypanosomiasis (see Chapter 52). Pharmacokinetics Soluble arsenic compounds are well absorbed through the respiratory and gastrointestinal tracts (Table 571). Percutaneous absorption is limited but may be clinically significant after heavy exposure to concentrated arsenic reagents. Most of the absorbed inorganic arsenic undergoes methylation, mainly in the liver, to monomethylarsonic acid and dimethylarsinic acid, which are excreted, along with residual inorganic arsenic, in the urine. When chronic daily absorption is <1000 mcg of soluble inorganic arsenic, approximately two thirds of the absorbed dose is excreted in the urine within 23 days. Inhalation of arsenic compounds of low solubility may result in prolonged retention in the lung and may not be reflected by urinary arsenic excretion. Arsenic binds to sulfhydryl groups present in keratinized tissue, and following cessation of exposure, hair, nails, and skin may contain elevated levels after urine values have returned to normal. However, arsenic in hair and nails as a result of external deposition may be indistinguishable from that incorporated after internal absorption. The use of phenylarsenic compounds as feed additives for poultry and swine was terminated in the United States in 2015. In some regions of the Pharmacodynamics Arsenic compounds are thought to exert their toxic effects by several modes of action. Inorganic arsenic or its metabolites may induce oxidative stress, alter gene expression, and interfere with cell signal transduction. Although on a molar basis, inorganic trivalent arsenic (As3+, arsenite) is generally two to ten times more acutely toxic than inorganic pentavalent arsenic (As5+, arsenate), in vivo interconversion is known to occur, and the full spectrum of arsenic toxicity has occurred after sufficient exposure to either form. Arsenic methylation requires S-adenosylmethionine, a universal methyl donor in the body, and arsenic-associated perturbations in one-carbon metabolism may underlie some arsenic-induced epigenetic effects such as altered gene expression. Arsine gas is oxidized in vivo and exerts a potent hemolytic effect associated with alteration of ion flux across the erythrocyte membrane; it also disrupts cellular respiration in other tissues. Arsenic is a recognized human carcinogen and has been associated with cancer of the lung, skin, and bladder. Marine organisms may contain large amounts of a well-absorbed trimethylated organoarsenic, arsenobetaine, as well as a variety of arsenosugars and arsenolipids. Arsenobetaine exerts no known toxic effects when ingested by mammals and is excreted in the urine unchanged; arsenosugars are partially metabolized to dimethylarsinic acid. Thioarsenite compounds that occur as minor metabolites of inorganic arsenic and methylated arsenic compounds in vivo may contribute to toxicity. The diagnosis may be confirmed by demonstration of elevated amounts of inorganic arsenic and its metabolites in the urine (typically in the range of several thousand micrograms in the first 23 days after acute symptomatic poisoning). Arsenic disappears rapidly from the blood, and except in anuric patients, blood arsenic levels should not be used for diagnostic purposes. Treatment is based on appropriate gut decontamination, intensive supportive care, and prompt chelation with unithiol, 35 mg/kg intravenously every 46 hours, or dimercaprol, 35 mg/kg intramuscularly every 46 hours. In animal studies, the efficacy of chelation has been highest when it is administered within minutes to hours after arsenic exposure; therefore, if diagnostic suspicion is high, treatment should not be withheld for the several days to weeks often required to obtain laboratory confirmation. Succimer has also been effective in animal models and has a higher therapeutic index than dimercaprol. However, because it is available in the United States only for oral administration, its use may not be advisable in the initial treatment of acute arsenic poisoning, when severe gastroenteritis and splanchnic edema may limit absorption by this route. Chronic Inorganic Arsenic Poisoning Chronic inorganic arsenic poisoning also results in multisystemic signs and symptoms. Overt noncarcinogenic effects may be evident after chronic absorption of more than 0. The time to appearance of symptoms varies with dose and interindividual tolerance. Constitutional symptoms of fatigue, weight loss, and weakness may be present, along with anemia, nonspecific gastrointestinal complaints, and a sensorimotor peripheral neuropathy, particularly featuring a stocking glove pattern of dysesthesia. Epidemiologic studies suggest a possible link to hypertension, cardiovascular disease mortality, diabetes, chronic nonmalignant respiratory disease, and adverse reproductive outcomes. Cancer of the lung, skin, bladder, and possibly other sites, including the kidney and liver, may appear years after exposure to doses of arsenic that are not high enough to elicit other acute or chronic effects. Some studies suggest that tobacco smoking may interact synergistically with arsenic in increasing the risk of certain adverse health outcomes. The diagnosis of chronic arsenic poisoning involves integration of the clinical findings with confirmation of exposure. High urine levels associated with overt adverse effects may return to normal within days to weeks after exposure ceases. Because it may contain large amounts of nontoxic organoarsenic Major Forms of Arsenic Intoxication A. Acute Inorganic Arsenic Poisoning Within minutes to hours after exposure to high doses (tens to hundreds of milligrams) of soluble inorganic arsenic compounds, many systems are affected. Initial gastrointestinal signs and symptoms include nausea, vomiting, diarrhea, and abdominal pain. Diffuse capillary leak, combined with gastrointestinal fluid loss, may result in hypotension, shock, and death. Pancytopenia usually develops within 1 week, and basophilic stippling of erythrocytes may be present soon after. Central nervous system effects, including delirium, encephalopathy, and coma, may occur within the first few days of intoxication. An ascending sensorimotor peripheral neuropathy may begin to develop after a delay of 26 weeks.
Nasal insufflation of desmopressin may be less effective when nasal congestion is present symptoms 20 weeks pregnant purchase tulasi line. Pharmacodynamics Vasopressin activates two subtypes of G proteincoupled receptors (see Chapter 17). V1 receptors are found on vascular smooth muscle cells and mediate vasoconstriction via the coupling protein Gq and phospholipase C. V2 receptors are found on renal tubule cells and reduce diuresis through increased water permeability and water resorption in the collecting tubules via Gs and adenylyl cyclase. In several clinical trials, both agents promoted the excretion of free water, relieved symptoms, and reduced objective signs of hyponatremia and heart failure. Tolvaptan treatment duration is limited to 30 days due to risk of hepatotoxicity, including life-threatening liver failure. Several other nonselective nonpeptide vasopressin receptor antagonists are being investigated for these conditions (see Chapter 15). Clinical Pharmacology Vasopressin and desmopressin are treatments of choice for pituitary diabetes insipidus. Bedtime desmopressin therapy, by intranasal or oral administration, ameliorates nocturnal enuresis by decreasing nocturnal urine production. Katznelson L et al: American Association of Clinical Endocrinologists medical guidelines for clinical practice for the diagnosis and treatment of acromegaly-2011 update. Penson D et al: Effectiveness of hormonal and surgical therapies for cryptorchidism: A systematic review. Webster J et al: A comparison of cabergoline and bromocriptine in the treatment of hyperprolactinemic amenorrhea. The findings of small testes and a microphallus in this patient suggest a diagnosis of hypogonadism, likely as a consequence of gonadotropin deficiency. He should also be evaluated for the presence of central diabetes insipidus and, if present, treated with desmopressin, a V2 vasopressin receptorselective analog. These complaints are new since she used to always feel "hot," noted difficulty sleeping, and could eat anything that she wanted without gaining weight. Other medications include calcium carbonate three times daily to "protect her bones" and omeprazole for "heartburn. Evaluate the management of her past history of hyperthyroidism and assess her current thyroid status. Identify your treatment recommendations to maximize control of her current thyroid status. These hormones contain 59% and 65% (respectively) of iodine as an essential part of the molecule. Calcitonin, the second type of thyroid hormone, is important in the regulation of calcium metabolism and is discussed in Chapter 42. Iodide, ingested from food, water, or medication, is rapidly absorbed and enters an extracellular fluid pool. The thyroid gland removes about 75 mcg a day from this pool for hormone synthesis, and the balance is excreted in the urine. If iodide intake is increased, the fractional iodine uptake by the thyroid is diminished. At - the apical cell membrane a second I transport enzyme called pendrin controls the flow of iodide across the membrane. At the apical 687 Iodide Metabolism the recommended daily adult iodide (I-) intake is 150 mcg (200 mcg during pregnancy and lactation and up to 250 mcg for children). The sites of action of various drugs that interfere with thyroid hormone biosynthesis are shown. Thyroidal peroxidase is transiently blocked by high levels of intrathyroidal iodide and blocked more persistently by thioamide drugs. In addition to thyroglobulin, other proteins within the gland may be iodinated, but these iodoproteins do not have hormonal activity. This process of proteolysis is also blocked by high levels of intrathyroidal iodide. The ratio of T4 to T3 within thyroglobulin is approximately 5:1, so that most of the hormone released is thyroxine. Many physiologic and pathologic states and drugs affect T4, T3, and thyroid transport. However, the actual levels of free hormone generally remain normal, reflecting feedback control. Peripheral Metabolism of Thyroid Hormones the primary pathway for the peripheral metabolism of thyroxine is deiodination by three 5deiodinase enzymes (D1, D2, D3). Deiodination of T4 may occur by monodeiodination of the outer ring, producing 3,5,3-triiodothyronine (T3), which is three to four times more potent than T4. The D1 enzyme is responsible for about 24% of the circulating T3 while 64% of peripheral T3 is generated by D2, which also regulates T3 levels in the brain and pituitary. The low serum levels of T3 and rT3 in normal individuals are due to the high metabolic clearances of these two compounds. Drugs such as amiodarone, iodinated contrast media, blockers, and corticosteroids, as well as severe illness or starvation, inhibit the 5-deiodinase necessary for the conversion of T4 to T3, resulting in low T3 and high rT3 levels in the serum. A polymorphism in the D2 gene can reduce T3 activation and impair thyroid hormone response. Evaluation of Thyroid Function the tests used to evaluate thyroid function are listed in Table 382.
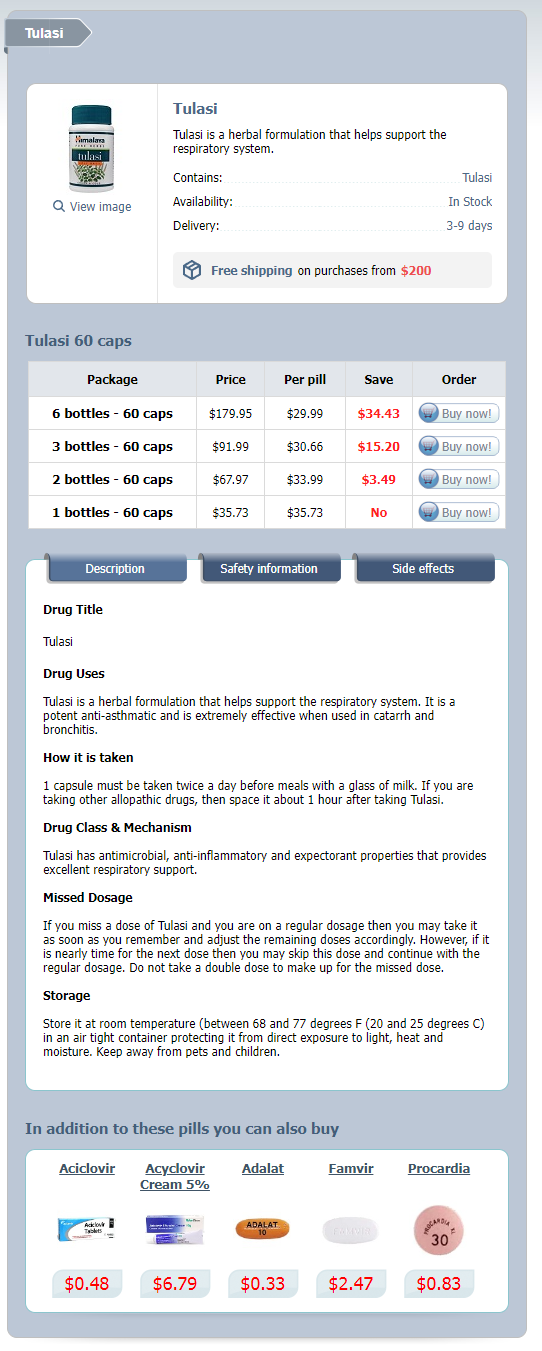
Tulasi Dosage and Price
Tulasi 60 caps
- 6 bottles - $179.95
- 3 bottles - $91.99
- 2 bottles - $67.97
- 1 bottles - $35.73
Both natural and synthetic corticosteroids are used for the diagnosis and treatment of disorders of adrenal function 9 medications that cause fatigue cheap 60caps tulasi amex. They are also used-more often and in much larger doses-for treatment of a variety of inflammatory and immunologic disorders. Secretion of the salt-retaining hormone aldosterone is primarily under the influence of circulating angiotensin and potassium. Corticotropin has some actions that do not depend on its effect on adrenocortical secretion. However, its pharmacologic value as an anti-inflammatory agent and its use in testing adrenal function depend on its secretory action. Inhibitors of the synthesis or antagonists of the action of the adrenocortical steroids are important in the treatment of several conditions. Some have minimal biologic activity and function primarily as precursors, and there are some for which no function has been established. The hormonal steroids may be classified as those having important effects on intermediary metabolism and immune function (glucocorticoids), those having principally salt-retaining activity (mineralocorticoids), and those having androgenic or estrogenic activity (see Chapter 40). In humans, the major glucocorticoid is cortisol and the most important mineralocorticoid is aldosterone. Adrenal androgens constitute the major endogenous precursors of estrogen in women after menopause and in younger patients in whom ovarian function is deficient or absent. Pregnenolone is the major precursor of corticosterone and aldosterone, and 17-hydroxypregnenolone is the major precursor of cortisol. The enzymes and cofactors for the reactions progressing down each column are shown on the left and across columns at the top of the figure. When a particular enzyme is deficient, hormone production is blocked at the points indicated by the shaded bars. Its synthesis and secretion are tightly regulated by the central nervous system, which is very sensitive to negative feedback by the circulating cortisol and exogenous (synthetic) glucocorticoids. The sensitivity of tissues to glucocorticoids is also circadian but inverse to that of cortisol, with low sensitivity in the late morning and high sensitivity in the evening and early night (lower panel). It is decreased by hypothyroidism, genetic defects in synthesis, and protein deficiency states. Albumin has a large capacity but low affinity for cortisol, and for practical purposes albumin-bound cortisol should be considered free. The half-life of cortisol in the circulation is normally about 6090 minutes; it may be increased when hydrocortisone (the pharmaceutical preparation of cortisol) is administered in large amounts or when stress, hypothyroidism, or liver disease is present. Only 1% of cortisol is excreted unchanged in the urine as free cortisol; about 20% of cortisol is converted to cortisone by 11-hydroxysteroid dehydrogenase in the kidney and other tissues with mineralocorticoid receptors (see below) before reaching the liver. Many cortisol metabolites are conjugated with glucuronic acid or sulfate at the C3 and C21 hydroxyls, respectively, in the liver; they are then excreted in the urine. Mechanism of Action Most of the known effects of the glucocorticoids are mediated by widely distributed intracellular glucocorticoid receptors. These proteins are members of the superfamily of nuclear receptors, which includes steroid, sterol (vitamin D), thyroid, retinoic acid, and many other receptors with unknown or nonexistent ligands (orphan receptors). In the absence of the hormonal ligand, glucocorticoid receptors are primarily cytoplasmic, in oligomeric complexes with chaperone heat-shock proteins (hsp). Free hormone from the plasma and interstitial fluid enters the cell and binds to the receptor, inducing conformational changes that allow it to dissociate from the heat shock proteins and dimerize. These transcription factors have broad actions on the regulation of growth factors, proinflammatory cytokines, etc, and to a great extent mediate the anti-growth, anti-inflammatory, and immunosuppressive effects of glucocorticoids. The acetonide-substituted derivatives (eg, triamcinolone acetonide) have increased surface activity and are useful in dermatology. Dexamethasone is identical to betamethasone except for the configuration of the methyl group at C16: in betamethasone it is beta (projecting up from the plane of the rings); in dexamethasone it is alpha. The glucocorticoid-binding domain is located at the carboxyl terminal of the molecule. This region folds into a "two-finger" structure stabilized by zinc ions connected to cysteines to form two tetrahedrons. The amino-terminal domain is involved in the transactivation activity of the receptor and increases its specificity. The coregulators do this by serving as bridges between the receptors and other nuclear proteins and by expressing enzymatic activities such as histone acetylase or deacetylase, which alter the conformation of nucleosomes and the transcribability of genes. Between 10% and 20% of expressed genes in a cell are regulated by glucocorticoids. Some of the effects of glucocorticoids can be attributed to their binding to mineralocorticoid receptors. A mineralocorticoid effect of the higher levels of cortisol is avoided in some tissues (eg, kidney, colon, salivary glands) by expression of 11-hydroxysteroid dehydrogenase type 2, the enzyme responsible for biotransformation to its 11-keto derivative (cortisone), which has minimal action on aldosterone receptors. When the complex binds a molecule of cortisol, an unstable complex is created and the hsp90 and associated molecules are released. A variety of regulatory factors (not shown) may participate in facilitating (coactivators) or inhibiting (corepressors) the steroid response. Among the proposed mechanisms are direct effects on cell membrane receptors for the hormone or nongenomic effects of the classic hormone-bound glucocorticoid receptor. The putative membrane receptors might be entirely different from the known intracellular receptors.