Urispas
General Information about Urispas
Urispas is often taken orally, with or without meals, and the dosage is usually based mostly on the individual's age, medical situation, and response to therapy. It is important to follow the prescribed dosage and to proceed taking the medicine even if symptoms enhance, as stopping the medication abruptly may cause a return of symptoms.
As with any medicine, Urispas may cause unwanted aspect effects in some people. Common unwanted aspect effects embody dry mouth, nausea, constipation, and dizziness. If these side effects turn into extreme or persistent, it is very important consult with a healthcare supplier.
Urispas is mostly well-tolerated and can provide aid for individuals affected by urinary problems. However, it is not recommended to be used in individuals with sure medical circumstances, similar to glaucoma, an enlarged prostate, or an obstructive gastrointestinal disorder. It is essential to discuss your medical historical past with your healthcare provider before starting Urispas.
Urispas, additionally identified by its generic name flavoxate, is a drugs used to treat urinary issues in people with certain medical circumstances. It belongs to a class of medication called urinary antispasmodics and works by stress-free the muscle tissue in the bladder, thereby lowering ache, frequency, and urgency of urination.
In conclusion, Urispas is a medicine that can provide aid from the pain, frequency, and urgency of urination in people with certain medical conditions. It is essential to consult with a healthcare supplier before starting treatment and to observe the prescribed dosage to attain most advantages. With correct use, Urispas can considerably enhance the quality of life for these suffering from urinary problems.
It is also important to inform your healthcare provider of some other drugs you take, as Urispas can work together with certain medicine, corresponding to antihistamines and antidepressants. It is also not recommended to drink alcohol whereas taking Urispas.
One of the main makes use of of Urispas is for people who are suffering from urinary incontinence, which is the involuntary leakage of urine. This situation could be brought on by a big selection of factors, including bladder muscle spasms, overactive bladder, and nerve injury. Urispas might help management these symptoms and improve the individual's high quality of life.
Another widespread use of Urispas is for people with urinary tract infections (UTIs). UTIs are attributable to bacteria coming into the urinary tract and can cause painful urination, frequent urination, and a powerful urge to urinate. Urispas can help alleviate these signs and also help forestall recurrent UTIs.
In addition, Urispas can be used for people with bladder issues, corresponding to interstitial cystitis and bladder pain syndrome. These conditions are characterized by bladder pain and discomfort, and Urispas may help cut back these symptoms by stress-free the muscle tissue within the bladder.
In the kidney muscle relaxant vicodin 200 mg urispas buy, P pili may then take over as the primary mediator of bacterial attachment via their binding to the glycolipid receptors (Stapleton et al, 1995). Subsequently, Schaeffer and colleagues (1981) confirmed these vaginal differences in women, but in addition they observed that the increased bacterial adherence was also characteristic of buccal epithelial cells. In addition, there was a significant relationship between vaginal cell and buccal cell receptivity. A direct nonlinear relationship between buccal and vaginal adherence in controls and patients was confirmed for urinary, vaginal, and anal isolates. Thus high vaginal cell receptivity was associated with high buccal cell receptivity. The A3 antigen was identified in 12 (34%) of the patients, which is significantly higher than the 8% frequency observed in healthy controls. In vitro adherence of Escherichia coli to vaginal (A) and buccal (B) cells from healthy controls and patients with recurrent urinary tract infections. A small variation in both vaginal cell and buccal cell receptivity may be observed from day to day in healthy controls. Adherence ranges from 1 to 17 bacteria per cell and appears to be both cyclic and repetitive. The number of bacteria per epithelial cell often correlated with the value obtained on the same day of the menstrual cycle 1 or 2 months previously. Premenopausal women are particularly susceptible to attachment of uropathogenic E. Reid and Sobel (1987) found that uropathogens attached in larger numbers to uroepithelial cells from women older than 65 years of age than to cells from premenopausal women 18 to 40 years of age. Blood group antigens and carbohydrate structures bound to membrane lipids or proteins also constitute an important part of the uroepithelial cell membrane. The protective effect in women with the secretor Le(a-b+) phenotype may be due to fucosylated structures at the vaginal cell surface or in the overlying mucus, which decreases availability of putative receptors for E. The nonsecretor status has also been associated with female acute uncomplicated pyelonephritis, especially in premenopausal women (Ishitoya et al, 2002). These studies individually and collectively support the concept that there is an increased epithelial receptivity for E. The possibility that vaginal mucus might influence bacterial receptivity was investigated by Schaeffer and colleagues (1994). The importance of vaginal fluid in bacteria/epithelial cell interactions was investigated in an in vitro model that measured the effect of vaginal fluid on the binding of bacteria to an epithelial cell line (Gaffney et al, 1995). Vaginal fluid from colonized women enhanced binding of bacteria to epithelial cells. Thus the vaginal fluid appears to influence adherence to cells and, presumably, vaginal mucosal colonization. Subsequent studies demonstrated that secretory IgA is the primary glycoprotein responsible for vaginal fluid receptivity (Rajan et al, 1999). As they grow, the bacteria maintain their typical rod shape of approximately 3 µm and form a loosely organized cluster, with microorganisms randomly oriented in the cell cytoplasm. Similar bacteria-engorged urothelial cells have been identified in 22% of Bladder Cells FimH binds mannosylated residues on the uroplakin molecules covering bladder superficial epithelial cells. The apical surfaces of umbrella cells appear as a quasi-crystalline array of hexagonal complexes composed of four integral membrane proteins known as uroplakins (Sun, 1996). High-resolution freeze-fracture electron microscopy has shown that the tips of these pili, including the adhesins, are buried in the central cavity of the uroplakin hexameric rings (Mulvey et al, 2000). In addition, polystyrene latex beads coated with FimH are quickly internalized in a process identical to bacteria expressing type 1 pili. Biofilms shield bacteria from environmental challenges such as antimicrobial agents and the host immune response (Donlan and Costerton, 2002). Characteristics of the biofilm that increase protection include the slower growth rate of the bacteria with associated physiologic changes, expression of factors that inhibit antimicrobial activity, and the inability of the antimicrobial agent to penetrate the biofilm matrix (Anderson et al, 2004b). These bacteria may become highly filamentous, reaching up to 70 µm or greater in length. This process occurs by approximately 24 hours after inoculation (Justice et al, 2004). It is possible that the filaments may help the bacteria evade the immunologic response. Exfoliation of superficial urothelial cells (see later) exposes underlying transitional cells. In contrast, urine will usually support the growth of nonfastidious bacteria (Asscher et al, 1968). Urine from normal individuals may be inhibitory, especially when the inoculum is small (Kaye, 1968). The most inhibitory factors are the osmolality, urea concentration, organic acid concentration, and pH. Bacterial growth is inhibited by either very dilute urine or a high osmolality when associated with a low pH. Much of the antimicrobial activity of urine is related to a high urea and organic acid content (Solomon et al, 1983). From a clinical perspective, however, these conditions do not appear to significantly distinguish between patients who are susceptible or resistant to infection.
In one of the largest and most comprehensive clinical series spasms jerking limbs 200 mg urispas otc, Weidner and associates (1991b) found significant bacteriuria (with uropathogenic organisms) in 4. Alexander and Trissel (1996) surveyed a cohort of 163 prostatitis patients on the Internet. These symptoms were best defined in the development of prostatitis symptom scores by Neal and Moon (1994), Krieger and colleagues (1996a), Nickel and Sorensen (1996), and Brahler and coworkers (1997). The predominant symptom in all these studies was pain, which was most commonly localized to the perineum, suprapubic area, and penis but can also occur in the testes, groin, or low back. Pain during or after ejaculation is one of the most prominent, important, and bothersome features in many patients (Shoskes et al, 2004). Storage and voiding urinary symptoms including urgency, frequency, hesitancy, and poor interrupted flow are associated with this syndrome in many patients. Over half of the men had pain or discomfort during or after sexual climax (ejaculatory pain may be the most discriminatory symptom). This assessment confirmed that perineal pain or discomfort was the most prevalent pain symptom (63%), followed by testicular pain (58%), pain in the pubic area (42%), and pain in the penis (32%); reports of pain during ejaculation and voiding were 45% and 43%, respectively. Further study of this cohort showed that pain has more impact on quality of life than urinary symptoms; pain severity and frequency are more important than pain localization or type. The symptoms tend to wax and wane over time; approximately one third of patients improve over 1 year (usually patients with a shorter duration of illness and fewer symptoms) (Nickel et al, 2002; Turner et al, 2004b; Propert et al, 2006b). Wenninger and associates (1996), employing a generic health status measure, the Sickness Impact Profile, showed that the mean scores were within the range of scores reported in the literature for patients with a history of myocardial infarction, angina, or Crohn disease. These investigators noted that the mental health component was affected more than the physical component of the quality-of-life assessment. Scientifically validated symptom indices not only improve the care of patients but also optimize clinical decision making in terms of comparing clinical trial outcomes. The quality of life or impact was captured in three additional questions that asked about the effect of symptoms on daily activities. The symptom index has also proved its usefulness in the evaluation and follow-up of patients in general clinical urologic practice (Nickel, 1999d; Nickel et al, 2001c). It assists in ruling out other perineal, anal, neurologic, pelvic, or prostate abnormalities and is an integral part of the lower urinary tract evaluation by providing prostate-specific specimens (Nickel, 2002a). In category I, acute bacterial prostatitis, the patient may be systemically toxic-that is, flushed, febrile, tachycardic, tachypneic, and even hypotensive. The patient usually has suprapubic discomfort and perhaps has clinically detectable acute urinary retention. Perineal pain and anal sphincter spasm may complicate the digital rectal examination. The expression of prostatic fluid is believed to be totally unnecessary and perhaps even harmful. Careful examination and palpation of external genitalia, groin, perineum, coccyx, external anal sphincter (tone), and internal pelvic floor and side walls may pinpoint prominent areas of pain or discomfort (Shoskes et al, 2008; Anderson et al, 2009b). The findings of pelvic floor dysfunction and spastic pain, myofascial pain, or painful trigger points has significant implications for developing treatment plans. The digital rectal examination should be performed after the patient has produced preprostatic massage urine specimens (see later) and after the perineal and pelvic examination. The prostate may be normal in size and consistency, and it has also been described as enlarged and boggy (loosely defined by me as softer than normal). The degree of elicited pain during prostatic palpation is variable and is unhelpful in differentiating a prostatitis syndrome. In patients with category I, acute bacterial prostatitis, a urine culture is the only laboratory evaluation of the lower urinary tract required. A midstream urine specimen will show significant leukocytosis and bacteriuria microscopically, and culturing usually discloses typical uropathogens. All four specimens are to be sent to the clinical microbiology laboratory for quantitative culture. Aliquots of the three urine specimens are centrifuged for 5 minutes and the sediment examined under high power for leukocytes (including aggregates of leukocytes), macrophages, oval fat bodies, erythrocytes, bacteria, and fungal hyphae. In a patient who has acute cystitis this localization is impossible, and in this case the patient can be treated with a short course (1 to 3 days) of therapy with an antibiotic such as nitrofurantoin, which penetrates the prostate poorly but eradicates the bladder bacteriuria. The patient provides a midstream pre-massage urine specimen and a urine specimen (initial 10 mL) after prostatic massage. In a retrospective personal series and a review of series in the literature, Nickel (1997a) noted that this test had 91% sensitivity and specificity compared with the gold standard Meares-Stamey test. Therefore the urethral specimens rarely resulted in detection of significant urethral inflammation, and in this series rarely did cultured organisms change the direction of clinical therapy in patients with prostatitis (without clinical urethritis). However, as discussed earlier in the section on etiology, other gram-positive organisms that typically colonize the urethra (Staphylococcus epidermidis, S. In patients with acute prostatitis, a blood culture should be considered, particularly if the patient has signs and symptoms of systemic infection (Etienne et al, 2010). A disadvantage of looking at a drop of prostatic fluid or urine sediment is that the cells may clump or aggregate, which renders quantifying them virtually impossible. The clinical relevance of adding cytologic examination of semen specimens (which is difficult without special staining techniques) is unknown. In fact, my colleagues and I have not been able to confirm the association between histologically proven prostate inflammation and prostatitis symptoms (Nickel et al, 2007), further confusing the issue of whether it is necessary to determine prostate-specific specimen inflammation, which is really just a surrogate for prostate inflammation. However, some investigators (Nickel, 2002b) have recommended that a separate aliquot of urine be examined cytologically for malignant cells, particularly examination detected 82% of the patients who had inflammation on one or both tests. This test, however, is only a screening test, and in patients in whom it is important to localize bacteria to the prostate versus the urethra.
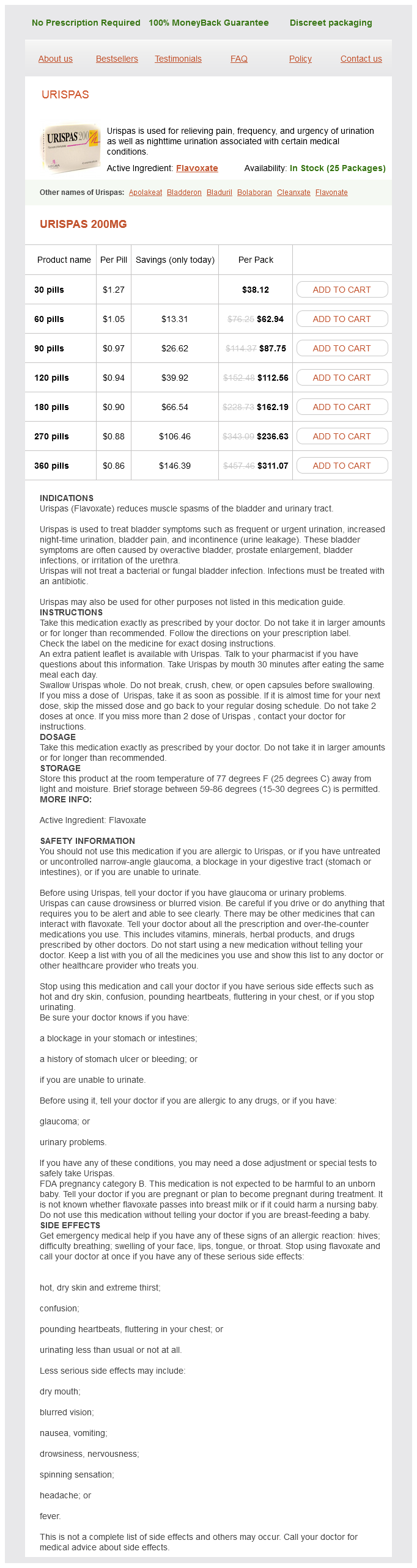
Urispas Dosage and Price
Urispas 200mg
- 30 pills - $38.12
- 60 pills - $62.94
- 90 pills - $87.75
- 120 pills - $112.56
- 180 pills - $162.19
- 270 pills - $236.63
- 360 pills - $311.07
Catastrophizing and pain-contingent rest predict patient adjustment in men with chronic prostatitis/chronic pelvic pain syndrome muscle relaxant succinylcholine buy urispas 200 mg with amex. Prostate histopathology in chronic prostatitis/chronic pelvic pain syndrome, a prospective biopsy study. Coccidioidomycosis of the prostate gland: two cases and a review of the literature. Validity and responsiveness of the National Institutes of Health Chronic Prostatitis Symptom Index. Men with pelvic pain: perceived helpfulness of medical and self-management strategies. Primary care and urology patients with the male pelvic pain syndrome: symptoms and quality of life. Incidence and significance of prostatic stones in men with chronic prostatitis/chronic pelvic pain syndrome. Clinical phenotyping of chronic prostatitis/chronic pelvic pain patients and correlation with symptom severity. Clinical phenotyping in chronic prostatitis/chronic pelvic pain syndrome and interstitial cystitis: a management strategy for urologic chronic pelvic pain syndromes. Greater endothelial dysfunction and arterial stiffness in men with chronic prostatitis/chronic pelvic pain syndrome-a possible link to cardiovascular disease. Anti-nanobacterial therapy for men with chronic prostatitis/chronic pelvic pain syndrome and prostatic stones: preliminary experience. Use of prostatic massage in combination with antibiotics in the treatment of chronic prostatitis. Immunohistochemical demonstration of chlamydial antigens in association with prostatitis. Comparative randomized pilot study of azithromycin and doxycycline efficacy in the treatment of prostate infection caused by Chlamydia trachomatis. Comparative randomized pilot study of azithromycin and doxycycline efficacy and tolerability in the treatment of prostate infection caused by Ureaplasma urealyticum. Comparative analysis of azithromycin and clarithromycin efficacy and tolerability in the treatment of chronic prostatitis caused by Chlamydia trachomatis. Comparative analysis of azithromycin and ciprofloxacin in the treatment of chronic prostatitis caused by Chlamydia trachomatis. Predictors of sexual and relationship functioning in couples with chronic prostatitis/chronic pelvic pain syndrome. Biofilm formation in uropathogenic Escherichia coli strains: relationship with prostatitis, urovirulence factors and anti-microbial resistance. Treatment of chronic bacterial prostatitis with ciprofloxacin: results of a one-year follow-up study. The diagnostic value of the immunologic response in bacterial and nonbacterial prostatitis. Chronic bacterial prostatitis treated with intraprostatic injection of antibiotics. Pain sensitization in male chronic pelvic pain syndrome: why are symptoms so difficult to treat The effect of alpha-adrenergic antagonists in chronic prostatitis/chronic pelvic pain syndrome: a meta-analysis of randomized controlled trials. Immunomodulatory action of levofloxacin on cytokine production by human peripheral blood mononuclear cells. Comparison of the efficacy of antibiotic monotherapy and antibiotic plus alpha-blocker combination therapy for patients with inflammatory chronic prostatitis/chronic pelvic pain syndrome. Zinc concentration in human prostatic fluid: normal, chronic prostatitis, adenoma and cancer. Inflammatory infiltrate (prostatitis) in whole mounted radical prostatectomy specimens from black and white patients is not etiology for racial differences in prostate specific antigen. Safety and efficacy of levofloxacin versus ciprofloxacin for the treatment of chronic bacterial prostatitis in Chinese patients. Stress is associated with subsequent pain and disability among men with non-bacterial prostatitis/pelvic pain. Efficacy of extracorporeal shock wave therapy for the treatment of chronic pelvic pain syndrome: a randomized, controlled trial. Physical therapist management of chronic prostatitis/chronic pelvic pain syndrome. Three-dimensional ultrasound guidance for percutaneous drainage of prostatitic abscesses. Laboratory findings in chronic prostatitis-with special reference to immunological and microbiological aspects. A pollen extract (Cernilton) in patients with inflammatory chronic prostatitischronic pelvic pain syndrome: a multicentre, randomised, prospective, double-blind, placebocontrolled phase 3 study. Impact of chronic prostatitis-like symptoms on the quality of life in a large group of men. The association between metabolic syndrome and the National Institutes of Health Chronic Prostatitis Symptom Index: results from 1673 men in China. Nerve growth factor level in the prostatic fluid of patients with chronic prostatitis/chronic pelvic pain syndrome is correlated with symptom severity and response to treatment. Effects of sodium pentosanpolysulphate on symptoms related to chronic non-bacterial prostatitis: a double-blind randomized study. Prostatitis-diagnostic criteria, classification of patients and recommendations for therapeutic trials. Quantitative culture of Ureaplasma urealyticum in patients with chronic prostatitis or prostatosis.