Vantin
General Information about Vantin
It's necessary to notice that Vantin just isn't efficient in opposition to all forms of bacteria. It specifically targets certain forms of micro organism, including Streptococci, Staphylococci, and a few strains of E. coli. Therefore, it is essential to only take Vantin for infections that are caused by these bacteria, as using it for different types of infections can contribute to the development of antibiotic resistance.
In conclusion, Vantin is a highly efficient and commonly prescribed antibiotic for the therapy of mild to reasonable bacterial infections. It is essential to observe the prescribed remedy plan and to take the complete course of medication in order to guarantee complete eradication of the an infection. If you experience any unwanted effects or have any concerns, it is essential to seek the assistance of your physician. With proper use, Vantin may help alleviate signs and aid in a swift recovery from bacterial infections.
Vantin is usually taken twice a day, with or without food. The dosage and length of therapy will range depending on the type and severity of the infection, in addition to a person's age and medical history. It's necessary to observe the prescribed therapy plan and complete the total course of antibiotics, even if signs enhance. Stopping medication too early can lead to the micro organism not being totally eradicated, leading to a recurrence of the an infection.
Vantin works by stopping the growth and copy of bacteria in the physique. It does this by interfering with the production of the bacterial cell wall, which is important for the bacteria’s survival. Without a cell wall, the bacteria are unable to maintain up their shape and ultimately die off. This helps to stop the unfold of infection and allows the physique's immune system to fight off the remaining bacteria.
It is necessary to tell your doctor of some other medicines you are taking, together with over-the-counter medicines and dietary supplements, as they could work together with Vantin. In explicit, it is important to keep away from taking Vantin with antacids or iron dietary supplements, as they can lower the effectiveness of the antibiotic.
Like any medication, Vantin may trigger unwanted facet effects in some people. Common side effects may include nausea, diarrhea, upset stomach, and headache. If these signs persist or turn into extreme, it may be very important contact a physician. Additionally, as with any antibiotic, there is a threat of creating an allergic response. Seek instant medical consideration if any signs of an allergic response occur, corresponding to rash, itching, swelling of the face or throat, or difficulty breathing.
Vantin, also known by its generic name cefpodoxime, is a commonly prescribed antibiotic used to treat a selection of bacterial infections. It belongs to the category of antibiotics known as cephalosporins, and is commonly prescribed for the remedy of delicate to moderate infections. Let's take a extra in-depth take a glance at what Vantin is, how it works, and what situations it may possibly effectively treat.
Vantin is an oral antibiotic, available in tablet type or as a suspension. It is often used to deal with infections of the respiratory tract, together with pneumonia, bronchitis, and sinusitis. It may additionally be used to treat skin and delicate tissue infections, as properly as sure forms of urinary tract infections. Vantin can also be effective in treating some sexually transmitted infections, corresponding to gonorrhea.
Incidence ranges from 5 to more than 20 cases per 1000 hospital admissions virus 86 order vantin 200 mg without a prescription,1 with the highest rates in immunocompromised, surgical, and elderly patients. Biofilm is composed of sessile bacteria embedded within a selfproduced exopolysaccharide matrix. Elderly patients,49-52 patients with disabilities,53 and patients tracheally intubated for extended periods are at increased risk for overgrowth of oropharyngeal pathogens, because of their inability to carry out effective oral care. Additionally, the extensive use of antibiotics in critical care settings promotes overgrowth of oropharyngeal pathogens. Interestingly, in a study by Heo,66 oral respiratory pathogens were often genetically identical to pathogens recovered from the lower airways, and rapid changes of bacterial species in both oral and pulmonary sites occurred. In the critically ill patient, the oral flora shifts early to a predominance of aerobic gram-negative pathogens,41 P. Pulmonary aspiration of oropharyngeal contents increases the risk for airway colonization and infection. The authors found that sinusitis increased the risk of nosocomial pneumonia by a factor of 3. Early studies have shown that in tracheally intubated patients, gastric pH higher than 4 was consistently associated with gastric colonization. Impairment of Respiratory Defense During Critical Illness and Tracheal Intubation In healthy subjects, the anatomic laryngeal barrier prevents aspiration of pathogen-laden oropharyngeal contents. A cough is one of the most efficient mechanisms to prevent further translocation of pathogens that may have gained access to airways. Hence, it hinders cough85; moreover, intubated patients are often sedated and unable to generate high expiratory flows. Mucociliary clearance is the primary innate airway defense mechanism to clear pathogens. In young, healthy nonsmokers, the mucociliary velocity ranges between 10 and 20 mm/min. Interestingly, the proportion of causative pathogens was similar between groups, except for a higher proportion of Streptococcus pneumoniae in patients not invasively ventilated. In most patients, two different bacterial species were isolated (34%); however, up to four different bacterial species coexisted in 7 patients (6%). Interestingly, no differences were detected in mortality rate at 30 days among patients with polymicrobial or monomicrobial infection. In the majority of the cases, resistance to third- and fourth-generation cephalosporins in carbapenem-susceptible strains of Escherichia coli and K. Legionella pneumophila as the cause of nosocomial pneumonia should be considered, particularly in immunocompromised patients. Candida promotes the development of pneumonia by creating biofilms that facilitate bacterial colonization. The World Health Organization has endorsed hand hygiene as the single most important element of strategies to prevent healthcare-associated infections. Also, ventilator circuits should be carefully manipulated to prevent the aspiration of colonized fluids from within the circuit. Therefore, preventive strategies should be implemented to reduce the overall incidence of the disease (Box 75-1). The Institute for Healthcare Improvement recommends that approaches with proven efficacy in infection control should be implemented together as a bundle because combined, they are expected to result in a better outcome than when implemented individually. Upon inflation, folds form along the cuff surface, and colonized oropharyngeal secretions may leak through these folds. Hence, upon inflation, smaller folds form with polyurethane cuffs, and aspiration of secretions above the cuff can be prevented or reduced. Some investigators have attempted to prevent aspiration by modifying the shape of the cuff. Continuous control of internal cuff pressure reduces risks of significant deflation and pulmonary aspiration. Interestingly, subglottic secretion drainage has been consistently associated with tracheal injury in clinical184 and laboratory studies. These factors are of paramount importance during the weaning period to shorten the duration of tracheal intubation. Therefore, circuits should not be changed unless the circuit is soiled or damaged. Importantly, inadvertent flushing of the contaminated condensate into the lower airways or nebulizers should always be avoided by careful emptying of ventilator circuits and water traps. To date, neither humidification strategy can be recommended as a pneumonia prevention tool. However, it is rational to deliver inspiratory gases at body temperature or slightly below and at the highest relative humidity to prevent loss of heat and moisture from the airways, change in rheologic properties of secretions, and impairment of mucociliary clearance. Body Position Early studies demonstrated that intubated patients are at higher risk for gastropulmonary aspiration when placed in the supine position (0 degrees) as compared with a semirecumbent position (45 degrees). Thus, as strongly suggested by the American1 and European guidelines,211 intubated patients should be preferentially kept in the semirecumbent position (30-45 degrees) rather than supine (0 degrees), especially when receiving enteral feeding. Laboratory reports212,213 have challenged the preventive benefits of the semirecumbent position. However, its alternative, parenteral nutrition, is associated with higher risks for catheter-related infections, complications of line insertions, higher costs, and loss of intestinal villous architecture, which may facilitate enteral microbial translocation.
In case of severe shock bacteria doubles every 20 minutes order on line vantin, where the patient is unresponsive to initial therapy, advanced hemodynamic monitoring is useful in identifying the key factors leading to hemodynamic abnormalities. Continuous or semi continuous measurements of cardiac output and/or Svo2 (or Scvo2) as well as P(cva)co2 are particularly useful to guide therapy and can also be nurse driven if strict medical protocols have been implemented. It is still possible to detect abnormalities in tissue perfusion through bedside microcirculatory exploration or by using the central venous toarterial carbon dioxide difference P(cva)co2. Continuous cardiac output measurement is provided by a combination of transpulmonary thermodilution and pulse contour analysis. Some devices are able to provide continuous cardiac output by pulse contour analysis without calibration. Bioreactance is a noninvasive technique to assess cardiac output but is not reliable in critically ill patients. Iterative blood gas analysis (another approach justifying insertion of an arterial line), metabolic acidosis and lactate concentration evalu ation, are other ways to assess global tissue oxygenation and to comple ment Scvo2 or Svo2 measurements. It is necessary to give supplemental O2 and ventilatory support in response to acute respira tory failure either through a face mask or by endotracheal intubation. Acute circulatory failure is treated by initial fluid loading in the absence of left ventricular failure (see later). In case of anaphylactic shock, emergency treatment includes intravenous epinephrine to treat allergyinduced vasodilation. Fluid loading is the first step in the treatment, and its first goal is to optimize left ventricular preload to improve Do2 by increasing cardiac output. Unless the patient has an acute lung injury, fluid loading aims at maximizing cardiac output33 according to the FrankStarling relationship, decreased lung gas exchange being detected by a decrease in Sao2 (or by a decrease in its surrogate, pulse oximetry). When applicable, dynamic preload dependency indices (arterial pulse pressure variations) should be preferred to static indices to guide fluid loading. Fluid administration should be titrated cautiously (except in severe hemor rhage) as fluid challenge. Of course, if cardiac output is monitored, stroke volume variations during fluid challenge must also be consid ered when applicable. Normalization of hemoglobin concentration (Hb), by red blood cell transfusion is not required. In all cases, targeting an Scvo2 larger than 70% may be a helpful guide for transfusion. All catecholamines are inotropes; they can be divided into (1) inodilators when they combine inotropic and vasodilatory properties (lowdose dopamine, any dose of dobutamine or dopexamine) or (2) inoconstrictors when they combine inotropic and vasoconstricting properties (highdose dopa mine, any dose of epinephrine or norepinephrine). Because of variable individual sensitivity to catecholamines, dose titration is necessary. In a large multicenter, randomized, doubleblind trial, vasopressin showed no benefit as a firstline vasopressor compared to norepineph rine in septic shock. Because increasing blood pressure through vasoconstriction may be associated with a decrease in flow, a tradeoff may exist between raising blood pressure and decreasing cardiac index that will vary depending on the specific vasopressor or combined inotrope/vasopressor. Applying such principles for symptomatic treatment in septic shock patients has resulted in improving mortality. The longer a site was involved in a Surviving Sepsis Campaign program, the greater was the benefit. Indeed, clinical studies, including one randomized, prospective trial, failed to show any hemodynamic benefit from bicarbonate therapy either to increase cardiac output or to decrease vasopressor requirements, regardless of the degree of aci demia. Cardiac function does not appear to be significantly decreased when the arterial pH remains higher than 7. Bicarbonate infusion, apart from renal or digestive losses, is therefore not recommended, unless the patient has hyperkalemia. Beyond 72 hours, absence of any hemodynamic improvement suggests that the hydrocortisone treat ment is futile. Although not oriented toward better circulatory efficacy, a number of treatments are essential in septic shock. Empiric or probabilistic antibiotics must be directed against gramnegative microorganisms and potentially resistant patho gens. It theo retically offers the following advantages: widening the spectrum of activity, antibacterial synergy, increased bactericidal speed, and decreased risk for emergent resistant germs. Treatmentaimsat(1)reducingpreloaddependency,(2)restoring cardiac contractility, (3) improving perfusion pressure, (4) reachingoxygensupply-to-oxygenneedsindependency,and(5) eliminatingdiseasesources. In cases of septic shock, control of the infectious source and the appropriate antibiotic therapy are essential prognostic factors. Surviving Sepsis Campaign: international guidelines for manage ment of severe sepsis and septic shock: 2008. The objective of the Surviving Sepsis Campaign, an international effort to increase awareness and improve outcome in patients with severe sepsis, was to develop management guidelines for severe sepsis and septic shock that would be of practical use for the bedside clinician. The process included a modified Delphi method, a consensus conference, several subsequent smaller meetings of subgroups and key individuals, teleconferences, and electronic-based discussion among subgroups and among the entire committee. Evidence-based recommendations, with their renewal in 2008, were made in 2004 regarding many aspects of the acute management of sepsis and septic shock that will hopefully translate into improved outcomes for the critically ill patient. The impact of these guidelines was formally tested and published in 2010 (see below). The Surviving Sepsis Campaign: results of an international guidelinebased performance improvement program targeting severe sepsis.
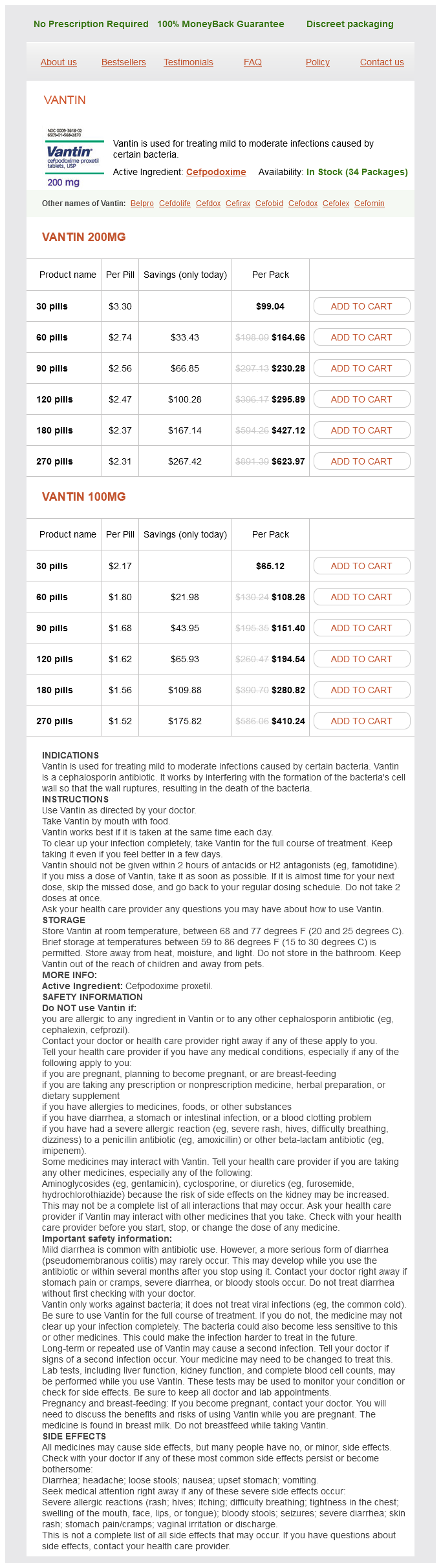
Vantin Dosage and Price
Vantin 200mg
- 30 pills - $99.04
- 60 pills - $164.66
- 90 pills - $230.28
- 120 pills - $295.89
- 180 pills - $427.12
- 270 pills - $623.97
Vantin 100mg
- 30 pills - $65.12
- 60 pills - $108.26
- 90 pills - $151.40
- 120 pills - $194.54
- 180 pills - $280.82
- 270 pills - $410.24
Ultrasonography can be performed at the bedside and provides excellent visualization of the biliary tree antimicrobial hypothesis purchase discount vantin on line. Ultrasonography can also detect abscesses, particularly in the pelvis when transvaginal or transrectal probes are used and can be used to guide percutaneous drainage procedures. Visualization is limited in the presence of bowel gas, and dressings, stomas, and drains can impede the positioning of the probe. Peritoneal Toilet Once source control has been achieved, additional intraoperative measures, including irrigation with fluid or antibiotic solutions and débridement of peritoneal surfaces, are ineffective and may be deleterious. It has been shown that irrigation with antibiotic solutions confers no benefit if parenteral antibiotics are administered9; however, a meta-analysis has also shown that pooled mortality is three-fold higher when saline solution is used rather than antibiotic solution for peritoneal lavage. The Open Abdomen Open abdomen management techniques are employed in select patients with diffuse peritonitis, inadequate primary source control, intestinal ischemia and discontinuity, abdominal compartment syndrome, or necrotizing infections of the anterior abdominal wall. In cases of peritonitis, goals of damage control include the assessment and reassessment of intestinal viability, decompression of the abdomen, and access for peritoneal toilet. The disadvantages of open abdomen management include fluid and protein loss, ileus, fistula formation, and ventral herniation. Neither planned re-laparotomy nor open abdomen management offer survival benefits as compared with repeat laparotomy on demand. Nasogastric and urinary catheter decompression are maintained, and early enteral nutrition has been shown to provide a benefit to recovery. After achieving resuscitation and adequate source control, aggressive diuresis should be initiated to reverse edema and facilitate closure of the abdomen. In these cases, healing by secondary intention is allowed to occur, and ventral hernias are repaired electively with absorbable mesh, biologic grafts, and skin grafts as necessary, but no earlier than 3 to 6 months after the acute episode, when all acute problems have resolved. Theabscess cavity demonstrates classic rim enhancement of the abscess wall (arrow). Consensus guidelines aim to implement source control interventions within the first 6 hours of management. Failure to obtain adequate source control reportedly occurs in 10% to 25% of cases of intraabdominal infection, depending on the severity and complexity of the infection. Studies Antibiotic Therapy Optimal antibiotic therapy for intraabdominal infection requires an agent or combination of agents active against gut-derived facultative enteric gram-negative bacilli and obligate anaerobes. A 2005 Cochrane review of 40 studies with 5094 patients comparing 16 different antibiotic regimens for empiric first-line therapy demonstrated equivalent efficacy and made no specific recommendations based on class I evidence. In hospital-acquired peritonitis, local antimicrobial resistance patterns should be considered. Newer agents, including tigecycline, ceftolozane-tazobactam, and moxifloxacin, are also equivalent in their ability to treat complicated intraabdominal infections and provide additional options in dealing with evolving bacterial resistance patterns. Antifungal treatment in an otherwise immunocompetent patient has not been found to improve survival. This treatment strategy limits intraabdominal infections caused by multidrug-resistant pathogens. Persistent sepsis should raise the possibility of inadequate source control, other nosocomial infections, or tertiary peritonitis. Broadening the antibiotic coverage or extending the duration of therapy are inappropriate strategies. Rather, sources of ongoing infection should be identified by a complete diagnostic reevaluation with physical examination, cultures, and imaging. The concept of deescalation, where targeted narrower spectrum agents replace empiric broad-spectrum antibiotics once susceptibilities are obtained, is safe and should help to reduce the risk of the emergence of antibiotic-resistant isolates. Whereas evidence-based recommendations are unequivocal, compliance with deescalation is poor. There is little proven benefit to empiric antibiotics, and most bacterial isolates tend to be resistant to standard regimens. Such coverage is recommended for complicated nosocomial infections in immunosuppressed patients, critically ill patients, and patients with valvular heart disease or implanted prosthetic materials. A fistula can contain an abscess cavity along its tract or exist internally as a connection between two intraabdominal structures. Therapy is directed at appropriate antibiotic therapy if signs of secondary infection are present, along with bowel rest, skin care, and parenteral nutritional support. Administration of octreotide may reduce fistula output, minimize fluid, electrolyte, and protein losses, and facilitate closure. Early recognition of organ dysfunction as a sign of persistent intraabdominal infection offers an opportunity to intervene while the process is still reversible. Administration of glucocorticoids in patients with septic shock does not improve survival or prevent sepsis and increases the risk of superinfection. Recent studies of medical patients indicate that this practice increases the rates of complications and mortality and should be avoided; however, there is evidence of benefit for critically ill surgical patients. Although an abscess, anastomotic dehiscence, and fistula formation are attributed most commonly to the failure of source control procedures, persistent peritonitis and sepsis often are attributed to the failure of host defenses. Enterocutaneous Fistula Enterocutaneous fistula formation is a dreaded complication of peritoneal inflammation and bowel injury. More than 80% of fistulas occur postoperatively, whereas fistulas that arise primarily from infection or irradiated bowel are rare. Critically ill patients with intraabdominal infection are at high risk of treatment failure. Adequate and timely resuscitation ensure tissue perfusion and oxygenation and can prevent the life-threatening complications associated with splanchnic hypoperfusion. Source control must also be adequate and timely and should include débridement of devitalized tissue, closure of perforations, drainage of infected collections, reduction of bacterial and toxin burden, and the use of appropriate broad-spectrum antimicrobial therapy.