Viagra with Dapoxetine
General Information about Viagra with Dapoxetine
The action of Sildenafil in Viagra with Dapoxetine is based on its ability to increase blood flow to the penis. This helps to loosen up the muscular tissues in the blood vessels, permitting for more blood to flow into the penis when sexually stimulated. This ends in a firmer and longer-lasting erection, making it simpler for men to attain and maintain an erection during sexual activity.
Not only does Viagra with Dapoxetine improve bodily efficiency, however it also has a optimistic impression on the psychological aspect of sexual exercise. By growing confidence and lowering anxiety, this medicine allows men to fully enjoy their sexual expertise without worrying about efficiency issues.
But the mix of these two medicine has proven to be much more effective in treating both points simultaneously. Viagra with Dapoxetine 100mg accommodates 100mg of Sildenafil (the active ingredient in Viagra) and 60mg of Dapoxetine. This unique mixture allows for a dual action that not only helps with reaching and maintaining an erection but in addition prolongs the time it takes to succeed in orgasm.
It's essential to notice that Viagra with Dapoxetine isn't a treatment for erectile dysfunction or untimely ejaculation. It is a temporary solution that must be taken solely when wanted, about one hour earlier than partaking in sexual exercise. It can be beneficial to speak with a doctor earlier than taking this treatment, as it may interact with other drugs or have contraindications for sure well being circumstances.
On the opposite hand, Dapoxetine works by blocking the reuptake of serotonin, a neurotransmitter that performs a role in controlling ejaculation. By doing so, Dapoxetine helps to extend the time interval from the start of sexual exercise until orgasm, permitting men to have better management over their ejaculation. This signifies that sex after taking Viagra with Dapoxetine will final much longer than usual, giving both partners more time to enjoy one another's firm.
In conclusion, Viagra with Dapoxetine is a game-changer for males who struggle with both erectile dysfunction and untimely ejaculation. It provides a powerful combination of two well-known medications that work collectively to enhance sexual performance and satisfaction. With Viagra with Dapoxetine, men can get pleasure from a brilliant and long-lasting sexual experience that shall be remembered by their companions eternally.
Studies have proven that Viagra with Dapoxetine can enhance the time to ejaculation fourfold, that means that a man who often ejaculates inside a minute may now find a way to last as long as four minutes. This is a big enchancment for men who battle with premature ejaculation and might lead to a more satisfying sexual expertise for each partners.
Both Viagra and Dapoxetine have been used separately for his or her respective benefits in treating male sexual disorders. Viagra, also called the 'little blue tablet', is a well-known medication for treating erectile dysfunction. It works by rising blood circulate to the penis, permitting for a firmer and longer-lasting erection. Dapoxetine, on the other hand, is primarily used to deal with premature ejaculation, helping males to have control over their orgasm and last longer in bed.
Viagra and Dapoxetine, two highly effective medications that are helping males around the world enhance their sexual efficiency and satisfaction. But what occurs when these two medicine are combined into one? The result's Viagra with Dapoxetine, a revolutionary treatment for males who wrestle with both erectile dysfunction and premature ejaculation.
Venous thrombosis can occur as a result of damage to the endothelium, turbulence created by the tip at venous branching points, or insufficient dilution of infusate that causes thrombophlebitis erectile dysfunction jacksonville fl viagra with dapoxetine 100/60mg purchase mastercard. Catheter erosion through the vessel or cardiac wall can produce extravasation, fistula formation, and pericardial tamponade. Catheters inserted into the left internal jugular or subclavian veins have also eroded into the bronchi; the ensuing venobronchial fistulas were associated with cough, pneumonia, and respiratory failure. Repositioning the catheter can usually be accomplished by interventional radiologists without catheter removal. The catheters can usually be repositioned by trained nurses using simple bedside techniques. Migration of the apheresis catheter in the subcutaneous space also manifests as access failure, because the catheter tip is pulled back to the wall of the inferior vena cava or out of the intravascular space. Furthermore, neither age nor the presence of inhibitors significantly altered the thrombotic incidence. However, because thrombotic complications have been documented less extensively for hemophiliac patients (especially compared with infectious complications), the true extent of subclinical and clinical complications is unknown. For sickle cell patients, although the condition itself is considered hypercoagulable, it remains unclear how this, coupled with the presence of indwelling access devices, affects the incidence of clinically significant and symptomatic thrombosis. Patients with multiple myeloma are likely at increased risk for venous thrombosis in the setting of hyperviscosity and treatment with thalidomide or lenalidomide-containing regimens; placing central venous access devices likely increases the risk. Still, the presence of overlying bones may make the visualization and direct assessment via compression techniques difficult. Although venography is the gold standard, it is limited by its invasiveness and cost. If venous obstruction is demonstrated, intraluminal versus extraluminal obstruction may be further defined by venography if clinically warranted. In patients with prior central venous catheterization associated with deep venous thrombosis, preprocedural duplex ultrasound may be useful to predict the success of repeat catheter placement. Additional risk factors include greater than one attempt at insertion, a previous catheter (with vessel wall trauma and endothelial damage), ovarian cancer, and left-sided insertion site. A threefold increased rate of catheter failure from thrombosis was noted for triple-lumen compared with double-lumen Hickman catheters. They may develop septic thrombophlebitis, superior vena cava syndrome, major Chapter 89 Indwelling Access Devices 1401 long-term upper extremity disability, venous gangrene, and pulmonary emboli. Suggested duration of therapy includes all time with the catheter in place or for 3 months, whichever period is longer. If anticoagulation is contraindicated, the catheter should be removed, the patient followed for any changes in relative contraindications, and anticoagulation initiated if otherwise permissible. Currently there is no sound evidence to guide duration of anticoagulant therapy in these patients. The recommended practice is to continue treatment while there is evidence of active cancer and while the patient is receiving antineoplastics. Vesicant Drug Extravasation It is very unusual for a spontaneous leak to form in a large-bore catheter, but an attempt to irrigate an occluded catheter with a small syringe can cause a rupture through which the drug can extravasate. Occlusion of the catheter tip by a fibrin sheath may force drugs back up the sheath and through the exit site of the catheter. This so-called backtracking appears to be more common with percutaneously placed access devices. Leaks may develop if the catheter is disconnected from the reservoir or if the catheter is punctured by mistake by the Huber needle. Outpatients using a port for continuous infusion of chemotherapy can experience drug extravasation if the Huber needle is dislodged from the septum. Even usually nonvesicant drugs can produce skin necrosis severe enough to warrant removal of the port. Use of the Port-A-Cath port, which has a thicker septum than the Mediport and Infus-A-Port devices, has been associated with only a 3% to 4% incidence of extravasation. The thickness of the septum has been postulated to be responsible for the low incidence of needle displacement noted with the Port-A-Cath, but no randomized trials have compared complications associated with the three devices. Selection of an appropriate length Huber needle and securing the needle to the chest wall with tape or a transparent occlusive dressing can provide some protection against dislodgment. If infusion pumps are used, attention must be paid to minimizing tension between the needle and the infusion tubing. Bolus thrombolytic therapy has reopened occluded catheters in 85% to 90% of episodes, and removal of the catheter is not usually required. Streptokinase is not commonly used because of its antigenic properties and associated allergic and anaphylactic reactions. Urokinase is available in recombinant form and has demonstrated efficacy for lysis of intraluminal thrombosis. Alteplase is available for catheter clearance in a 2 mg/2 mL vial, a volume sufficient to fill most catheter lumens. High-dose streptokinase therapy is effective but expensive and is associated with a high incidence of bleeding. It is not recommended for patients with bleeding risks such as thrombocytopenia or mucositis. Infusion of urokinase for 24 to 72 hours restored catheter patency in 74% of patients (81% of those with clots present less than 7 days, and 56% of those with clots present more than 7 days). Infusion into the superficial venous circulation of the involved extremity was not effective. Although a low infusion concentration was used (5000 international units/hour of streptokinase or 500 to 2000 international units/kg/hour of urokinase), a systemic lytic state was documented.
The vinca alkaloids, most notably vincristine, are neurotoxic, but they are not always associated with painful neuropathy erectile dysfunction injection test 100/60mg viagra with dapoxetine buy overnight delivery. Thalidomide, lenalidomide, bortezomib, cisplatin, oxaliplatin, and paclitaxel are all commonly used agents that carry a significant risk of causing painful peripheral neuropathy. The major manifestations are burning paresthesias of the hands and feet and loss of reflexes. Paclitaxel also causes a motor neuropathy, which predominately affects proximal muscles. Studies have evaluated numerous agents for prevention of painful peripheral neuropathy, although there have not been any magic bullets. Amifostine and leukemia-inhibitory factor do not prevent neurotoxicity induced by these agents. Magnesium and calcium infusions have been shown to prevent neurotoxic symptoms associated with oxaliplatin without affecting its antitumor activity. Glutathione at doses of 1500 mg/m2 administered before each dose of oxaliplatin for 12 cycles prevented grade 2 to 4 toxicities compared with placebo with no effect on response rate. Vitamin E has been shown to prevent neurotoxicity associated with cisplatin in small open-label evaluations. Glutamine 10 g three times daily for 4 days has had positive results as a neuroprotective agent in paclitaxeltreated patients. Acetyl-L-carnitine 1 g three times daily has been reviewed in the treatment of cisplatin- and paclitaxel-induced peripheral neuropathy, although no randomized studies have been done. Treatment of chemotherapy-induced painful peripheral neuropathy includes the usual agents used for patients with neuropathic pain from any etiology. In addition to treating these painful symptoms of neuropathy, the doses of the chemotherapy often require reduction or even discontinuation of therapy. Sickle Cell Anemia Patients with sickle cell anemia have chronic and episodic pain despite optimal medical therapy, and 60% of patients with sickle cell anemia will have an episode of severe pain each year. Chronic arthritic pain can be treated with physical therapy and full doses of antiarthritic medication, but some patients require low doses of chronic opioid therapy to maintain independent functioning. Several studies have confirmed the safety and efficacy of long-term opioids in the treatment of pain of nonmalignant origin. When a patient with sickle cell anemia experiences pain, it is important to attempt to define the precise cause of the pain before attributing it to a vaso-occlusive crisis. Acute vaso-occlusive pain may occur along with the chronic pain caused by the long-term complications of compression fractures, avascular necrosis, arthropathies, fractures, avascular necroses, and leg ulcers. Using short-acting analgesics on an "as-needed basis" exposes the patient to periods of insufficient analgesia, anticipation, and anxiety. Their repeated requests for medication to relieve their ongoing pain may be mistakenly interpreted as "drug-seeking behavior," and they may be unfairly stigmatized. When adequate analgesia is obtained, a long-acting opioid, or a sustainedrelease opioid may be initiated with intermittent use of rescue medication. In adult patients with frequent episodes of painful crisis, the use of long-acting opioid medications reduced visits to the emergency department and hospitalizations and shortened the lengths of stay in hospital. Meperidine should be avoided in this population and has been associated with seizures in 1% to 12% of these patients. Problems of Elderly Patients Pain management in elderly patients is a highly prevalent problem. It is complicated by difficulties in pain assessment and by the altered pharmacokinetics of opioids and of psychotropic adjuvant medications. The effective doses for these patients are half to one-fourth of those needed in younger patients. Patients should be monitored carefully for the development of sedation or confusion, especially if they are receiving antihistaminic agents. Neuropathic pain syndromes are common in older adults, and the adjuvant analgesics gabapentin and pregabalin are often used. Common side effects include somnolence and ataxia that can be problematic in the geriatric population. Treatment should be initiated at 100 mg of gabapentin or 50 mg of pregabalin at bedtime, and close monitoring for side effects should occur before dose escalation. The intestinal involvement that usually causes the most physical pain includes abdominal cramping and voluminous diarrhea. Addition of octreotide continuous infusion at 50 to100 µg/hr intravenously or intermittent dosing at 500 µg subcutaneously every 8 hours may be effective in decreasing the volume of diarrhea and level of abdominal pain. The starting dose of nortriptyline should be low (usually 10 mg at bedtime), and the dose should be slowly increased as tolerated. Treatment of opioid-related urinary retention may include generic Proscar (5 mg/day) in patients with benign prostatic hypertrophy and bethanechol (10 to 50 mg three times daily) to help increase bladder smooth muscle tone. The vast majority of patients can expect complete control of vomiting29 (see box on Combination Antiemetic Regimens), and most patients also are free of nausea. The vestibular system activates the vomiting center when stimulated by motion or disease. Histamine (H1) and acetylcholine M1 receptors are present on vestibular afferents. Endogenous or exogenous bloodborne toxins may activate chemoreceptors in the area postrema of the floor of the fourth ventricle via dopamine type 2 receptors. In addition, there may be direct activation of H1 receptors in the meninges secondary to increased intracranial pressure. The means by which chemotherapy agents induce vomiting are still incompletely understood, but the most likely mechanism is believed to include stimulation of the chemoreceptor trigger zone. Cognitive therapy, as well as antianxiety and amnesic agents, may provide effective antiemesis.
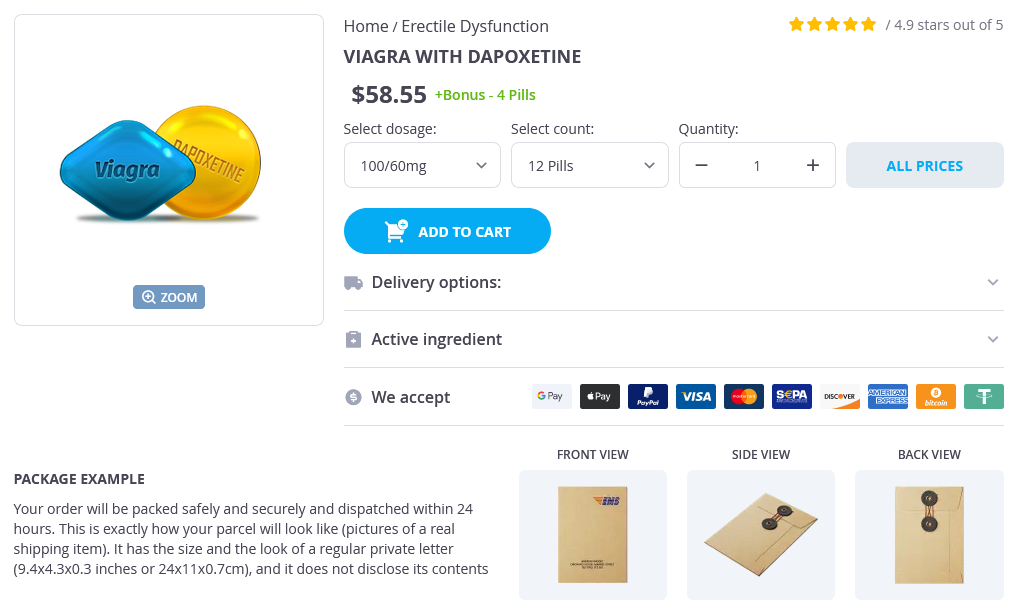
Viagra with Dapoxetine Dosage and Price
Viagra with Dapoxetine 100/60mg
- 12 pills - $65.05
- 20 pills - $97.08
- 32 pills - $135.07
- 60 pills - $232.04
- 90 pills - $325.09
- 120 pills - $429.08
- 180 pills - $567.03
- 270 pills - $793.01
- 360 pills - $975.06
Viagra with Dapoxetine 50/30mg
- 30 pills - $74.78
- 60 pills - $132.17
- 120 pills - $246.96
- 240 pills - $476.52
- 300 pills - $591.30
The vast majority of patients will have lowpositive IgG antibody titers 6 months after the acute infection erectile dysfunction zurich buy viagra with dapoxetine 100/60mg lowest price. To determine the approximate time of infection in IgG-positive adults, specific IgM antibody determinations should be performed. Detectable T gondii specific IgM antibodies can indicate recent infection, chronic infection, or a false-positive reaction. Enzyme immunoassays are the most sensitive tests for IgM, and indirect fluorescent antibody tests are the least sensitive tests for detecting IgM. Immunoglobulin Mspecific antibodies can be detected 2 weeks after infection (IgGspecific antibodies are usually negative during this period), achieve peak concentrations in 1 month, decrease thereafter, and usually become undetectable within 6 to 9 months. However, in some people, a positive IgM test result may persist for years without apparent clinical significance. In adults, a positive IgM test should be followed by confirmatory testing at a laboratory with special expertise in Toxoplasma serology when determining the timing of infection is important clinically (eg, in a pregnant woman). The presence of high-avidity IgG antibodies indicates infection occurred at least 12 to 16 weeks prior. The presence of low-avidity antibodies is not a reliable indication of more recent infection, and treatment may affect the maturation of IgG avidity and prolong the presence of low-avidity antibodies. Tests to detect IgA and IgE antibodies, which decrease to undetectable concentrations sooner than IgM antibodies do, are also useful for diagnosis of congenital infections and infections in pregnant women, for whom more precise information about the duration of infection is needed. T gondiispecific IgA and IgE antibody tests are available in Toxo plasma reference laboratories but, generally, not in other laboratories. Polymerase chain reaction assay and T gondii specific immunoperoxidase staining can be attempted with virtually any body fluid or tissue, depending on the clinical scenario. Essentially any tissue can be stained with T gondiispecific immunoperoxidase; the presence of extracellular antigens and a surrounding inflammatory response are also diagnostic of toxoplasmosis. Isolation of the parasite by mouse or tissue culture inoculation can also be attempted from amniotic fluid. Serial fetal ultrasonographic examinations can be performed in cases of suspected congenital infection to detect any increase in size of the lateral ventricles of the central nervous system or other signs of fetal infection, such as brain, hepatic, or splenic calcifications. Some states routinely screen all newborns for the presence of antibody to T gondii. Postnatal Congenital toxoplasmosis should be considered in neonates born to women suspected of having or who have been diagnosed with primary T gondii infection during gestation, women infected shortly before conception (eg, within 3 months of conception), immunocompromised women with serologic evidence of past infection with T gondii, or any neonate with clinical signs or laboratory abnormalities suggestive of congenital infection. Infected newborns can have any combination of positive or negative IgM and IgA antibodies. Although placental leak can occasionally lead to false-positive IgM or IgA reactions in the newborn, repeat testing at approximately age 10 days can help confirm the diagnosis because the half-life of these immunoglobulins is short and the titers in a neonate who is not infected should decrease rapidly. The sensitivity of T gondiispecific IgM as determined by an immunosorbent agglutination assay is 87% in newborns born to mothers not treated during gestation; sensitivity for IgA antibodies is 77%; and when both are taken into consideration, the sensitivity increases to 93%. The indirect fluorescent assay or enzyme immunoassay for IgM should not be relied on to diagnose congenital infection. Congenital infection is confirmed serologically by persistently positive IgG titers beyond the first 12 months of life. Conversely, in an uninfected infant, a continuous decrease in IgG titer before 12 months without detection of IgM or IgA antibodies will occur. Transplacentally transmitted IgG antibody usually becomes undetectable by 6 to 12 months of age. Immunocompromised patients should be tested for T gondiispecific IgG before commencing immunosuppressive therapy or as soon as their status of immunosuppression is diagnosed to determine whether they are chronically infected with T gondii and at risk of reactivation of latent infection. Active disease in immunosuppressed patients may or may not result in seroconversion and a 4-fold increase in IgG antibody titers; consequently, serologic diagnosis in these patients is often difficult. Toxoplasmic encephalitis can be diagnosed presumptively on the basis of characteristic clinical and radiographic findings. Magnetic resonance imaging usually reveals the presence of multiple brain-occupying and ringenhancing lesions. In these patients, other organisms, such as invasive mold infections and nocardiosis, should be considered before beginning an empiric anti-T gondii therapy. Ocular Toxoplasmosis Toxoplasmic chorioretinitis is usually diagnosed on the basis of characteristic retinal lesions in conjunction with a positive serum T gondiispecific IgG test result. All patients with eye disease should have an IgM test performed; if a positive IgM test result is confirmed at a reference laboratory and eye lesions are consistent with toxoplasmic chorioretinitis, ocular disease is the result of an acute T gondii infection rather than reactivation of a chronic infection. When indicated (eg, chorioretinitis, significant organ damage), the combination of pyrimethamine and sulfadiazine, with supplemental leucovorin (folinic acid) to minimize pyrimethamine-associated hematologic toxicity, is the regimen most widely accepted for children and adults with acute symptomatic disease. For symptomatic and silent congenital infections, pyrimethamine combined with sulfadiazine (supplemented with folinic acid) is recommended as initial therapy. However, the optimal dosage and duration are not established definitively and should be determined in consultation with an infectious diseases specialist. Maternal therapy may decrease the severity of sequelae in the fetus once congenital toxoplasmosis has occurred. Cysts are usually spherical in the brain but more elongated in cardiac and skeletal muscles. They may be found in various sites throughout the body of the host but are most common in the brain and skeletal and cardiac muscles. Within a myocyte is a pseudocyst containing numerous tachyzoites of Toxoplasma gondii. Several myocardial contraction bands and scattered inflammatory cells are visible. His computed tomography scan demonstrated hydrocephalus and periventricular calcification, suggestive of congenital infection, such as toxoplasmosis, rubella, cytomegalovirus, or herpes simplex. Toxoplasma serology was positive and the neonate was treated for congenital toxoplasmosis with pyrimethamine, sulfadiazine, and folinic acid.