Viramune
General Information about Viramune
Typically, Viramune is utilized in mixture with different HIV medications as a half of antiretroviral therapy (ART). This is as a result of the virus can become resistant to 1 medicine if it is used alone, making mixture remedy necessary for effective therapy. The specific mixture of medicines used will rely upon the individual's medical historical past and viral load (the amount of virus present in the body).
Viramune is on the market in tablet form and is normally taken once or twice a day, with or without food. It is necessary to take this medication precisely as prescribed by a healthcare provider. Skipping doses or not taking the medication as directed can lead to the development of drug resistance and decrease its effectiveness.
In conclusion, Viramune is a vital medicine in the treatment of HIV an infection. Along with other HIV medications, it helps to scale back the viral load and strengthen the immune system. However, it's not a cure for HIV and people ought to proceed to take precautions to prevent the spread of the virus. If you are dwelling with HIV, it could be very important work carefully together with your healthcare supplier to discover out the most effective treatment plan for you.
As with any medication, there are potential unwanted facet effects related to Viramune. These can embody rash, headache, dizziness, upset stomach, and liver issues. In rare cases, extra severe reactions similar to Stevens-Johnson syndrome (a critical pores and skin disorder) and liver failure have been reported. If any of these side effects occur, it is very important search medical attention instantly.
Viramune, additionally recognized by its generic name nevirapine, is a drugs used within the therapy of HIV an infection. HIV, or human immunodeficiency virus, is a virus that attacks the body's immune system, making it more prone to other infections and illnesses. Viramune is an important software within the battle in opposition to HIV, as it works to minimize back the quantity of virus in the physique and sluggish the development of the disease.
It can additionally be necessary to note that Viramune isn't a remedy for HIV infection. It is simply a therapy that helps to regulate the virus and enhance the immune system. Therefore, it is important for people taking this medicine to continue to apply secure intercourse and take different precautions to stop the spread of HIV to others.
Viramune was first accredited by the Food and Drug Administration (FDA) in 1996 for the remedy of HIV infection. It belongs to a category of medications known as non-nucleoside reverse transcriptase inhibitors (NNRTIs). These medications work by blocking the motion of a specific enzyme (reverse transcriptase) that's needed for the virus to copy and spread within the body.
When used in combination with different HIV medicines, Viramune has been shown to considerably scale back the viral load in the body and enhance the variety of CD4 cells. CD4 cells are a kind of white blood cells which are essential in preventing infections. By lowering the viral load and increasing CD4 cell depend, Viramune helps to strengthen the immune system and enhance total well being.
In our experience of operating on our own recurrences as well as other recurranees symptoms hypoglycemia cheap 200 mg viramune with amex, the most common cause was a missed indirect hernia. Bleeding: Blseding is not a common problem as the dissection is generally parformed in a bloodless plane. A preperitoneal repair should be avoided or approached with caution in patients who require aggressive preoperative anticoagulation secondary to other underlying hypercoagulable or thromboembolic conditions (ie. It is themfore advisable that an anterior repair be carried out in these patients so that if bleeding does occur it is obvious and can be addressed immediately. The patient will usually pmsent at the initial postoperative visit complaining of persistence of the hernia. On examination, a smooth slightly tender mass, which is nonreducible and does not change with Valsalva will be identified in the inguinal canal. If obtained, an ultrasound will demonstrate the pmsence of the seroma and we will reassure the surgeon as well as the patient. Unless there are clear signs of infection, no other intervention needs to be or should be taken in regards to the presence of the seroma. Chronic groin pain: Chronic groin pain or inguinodynia is defined as pain within the groin. These nerves are the iliohypogastric, ilioinguinal, genitofemoral, and lateral femoral cutaneous nerves. Because of the performance of the Kugel hernia repair in regards to its muscle splitti. In addition, in the Kugel approach, there is no need for fixation within the preperitoneal space that could entrap the lateral femoral cutaneous nerve. In addition, it is not necessary or recommended to skeletonize the external iliac vein, the most medial structure within the vascular bundle. Dissection only needs to be carried out at the level of the lacunar ligament to assure that no femoral hernia exists. Avoidance of this excessive dissection will protect the vessels from dimct exposum with a surface layer of undisturbed tissue. There has been intense medical and legal discussion in mgards to fractured rings within the Kugel patches resulting in bowel injury. This problem has only been reported in Extra Large Composix Kugel products utilized in ventral hernia repairs and never truly verified. No reports of such injuries have been reported in a Ku,gel inguinal repair with the Kugel hernia patch. A fully 96 Part I Open Inguinal Hernia expended and appropriately sized patch, with its semi-rigid ring, is difficult to displace through any hernia defect encountered in the groin. Since the patch is placed without fixation sutures, hydrostatic tissue forces also come in to play in securing the patch in to position. This method of repair provides protection for the entire groin including the femoral canal and the surgical incision itself. It is an ideal approach following prior anterior hernia repair as it avoids most of the associated scar tissue from the prior repair. The disadvantages of this repair are related to obtaining the appropriate visualization of the preperitoneal space, assurance of dissection within the correct preperitoneal space, and confidence on the part of the surgeon in regards to the proper deployment of the mesh in to the appropriate space. Working with an experienced surgeon on several cases before attempting the repair solo allows for the surgeon to gain the confidence in regards to being able to clearly identify the preperitoneal space and its anatomy as well as to recognize when proper deployment of the mesh is achieved. Summary As incidence of recurrence, safety, ease of performance, and shortened disability periods are considered in selection of a hernia repair, the Kugel inguinal hernia repair demonstrates its attractive advantages. Biomaterials for abdominal wall hernia surgery and principles of their application. Minimally Invasive repair of groin and ventral hernias using a self expanding mesh patch. The development of a clinical trial to determine if watchful waiting is an acceptable alternative to routine herniorrhaphy for patients with minimal of no hernia symptoms. Open, preperitoneal hernia repair with the Kugel patch: A prospective, multicentre study of 450 repairs. Patients with femoral hernias are on average older than those with inguinal hernias (63 year vs. This is important because 35% of femoral hernias require emergent surgery due to incarceration or strangulation, compared to 5% of inguinal hernias. Also, 18% of emergent femoral hernia repairs require a bowel resection, as compared to 5% of inguinal hernias. Historically, mortality rates as high as 25% had been reported, and modern day mortality rate for femoral hernia surgery is 3%, which is ten-fold higher than other hernia repairs. Thus, watchful waiting is not advocated for femoral hernias and early elective repair is recommended whenever possible. The hernia has a tendency to migrate anteriorly; thus on examination this bulge may present as a mass above the inguinal ligament and misdiagnosed preoperatively as an incarcerated inguinal hernia. In obese patients, it is common to miss a small incarcerated or strangulated hernia. This will help in planning for surgery, as the surgical approach differs based on the clinical scenario. If a strangulated hernia is diagnosed clinically or radiologically preoperative, the preferred choices of repair include: (1) Open preperitoneal approach, or (2) laparoscopic transabdominal approach. With both of these techniques, the hernia contents may be examined for signs of strangulation and addressed through the same approach while performing the femoral hernia repair. Also, a concomitant inguinal hernia (usually direct) may be diagnosed and repaired. These include: (1) Infrainguinal approach, (2) transinguinal approach, (3) open preperitoneal approach, (4) laparoscopic preperitoneal or transabdominal approach. Femoral hernias may be missed after repair of an inguinal hernia, may occur after repair of a direct hernia, or may be recurrent.
Enough emphasis cannot be placed on the importance of both a thorough history and physical exam when an examiner first encounters a patient with neuromuscular weakness medicine gabapentin buy viramune with a visa. Once a patient is felt to require inpatient admission, a few simultaneous events should occur. During initial clinical assessment, if the patient demonstrates "paradoxical breathing" (movement of chest outward and abdomen inward), shortness of breath (inability to count beyond 20 in one breath) and/or tachypnoea, the physician in charge should anticipate the probable evolution of a myasthenic exacerbation of a myasthenic crisis. Myasthenic crisis can be defined as a patient who develops respiratory insufficiency that may necessitate mechanical ventilation. In addition to bedside spirometry, further data to be collected are arterial blood gases, continuous pulse oximetry, cardiac telemetry and serial mental status assessment. Cardiac telemetry is also important because arrhythmias are a common cause of death in myasthenic crisis. Serial mental status examination is a useful means to monitor the patient for respiratory compromise and decreasing airway protection. Evaluation for early elective mechanical ventilation will avoid emergency intubations and decrease the risk of aspiration pneumonia. The first choice, non-invasive positive pressure ventilation, may be a viable option in patients without hypercapnia and it may afford enough time for medical therapy to take effect. Especially with a change in mental status, the patient will no longer be able to protect their airway by removing the facemask. One final note regarding mechanical ventilation is to not overlook the importance of discussing with the patient and family members the future possibility of ventilatory support prior to its need. Especially in the elderly or those with advance directives, knowing that intubation during a myasthenic crisis often acts as a temporary bridge, helps patients and their families make fully informed decisions. This also allows the clinician to make an educated decision if respiratory failure occurs in the middle of the night and the patient no longer retains a decision making capacity. Initial concomitant introduction of high-dose steroid therapy is not recommended due to the possibility of exacerbating myasthenic symptoms; however, if the patient begins to improve by day 3, one can consider its addition. Patients who evolve in to a myasthenic crisis or present with one require plasma exchange therapy, which provides slightly more robust results in a shorter time period. With any suspicion of pneumonia or other source of infection, treatment of that infection is equally important. Yet, up to one third of patients may have retained reflexes and cranial nerves are often spared. In a patient with previous spontaneous movements and intact sensation, failure to withdraw to painful stimuli applied to a distal extremity should suggest sensory loss. Often, reflexes are normal or slightly decreased and the sensory exam should remain intact. Whenever evaluating a critically ill patient, it is important to assure that the patient is awake, alert, and understands your commands. Selecting where to biopsy should be based on an area that has not undergone extensive disease because results may be non-diagnostic. In addition, aggressive physical rehabilitation provides the best chance to regain function. Poisoning of the neuromuscular junction can be broadly categorized in to pharmacologic, biologic and environmental. Pharmacologic: Persistent Neuromuscular Blockade Residual neuromuscular blockade has recently increased in incidence as the utilization of neuromuscular blockade has moved beyond intubation and the operating room. Agents for neuromuscular blockade are grouped in to two categories: depolarizing (succinylcholine) and non-depolarizing. Depolarizing agents act by binding to the postsynaptic nicotinic acetylcholine receptor, leading to persistent depolarization. The mechanism of action for this group limits its current use beyond rapid sequence intubation. Non-depolarizing agents bind with postsynaptic nicotinic acetylcholine receptors and prevent acetylcholine from reaching its target, thereby preventing depolarization. Commonly used non-depolarizing agents used and clinical settings where they are applied are summarized in Table 75. Since these medications are used frequently without side effects, concurrent factors have been identified which can increase the risk for neuromuscular weakness due to residual neuromuscular blockade. Advanced age, renal insufficiency (pancuronium, vecuronium and rocuronium), hypermagnesaemia, metabolic acidosis and edematous states which require higher doses for clinical effect are all clinical situations which can prolong neuromuscular blockade. Also, some medications including beta-blockers, calcium channel blockers, aminoglycosides, clindamycin and cyclosporine have been implicated. Furthermore, some data suggest that concurrent corticosteroid and pancuronium or vecuronium use can have myotoxic side effects. If this is not accessible, then the tibialis posterior and the flexor hallucis brevis muscle are also acceptable. ElecCommon agents · Benzylisoquinolinium compounds: Cisatracurium Atracurium · Aminosteroid compounds: Pancuronium Vecuronium Rocuronium · · · · Facilitating mechanical ventilation Shivering protocols in cooled patients Treating malignant elevated intracranial pressure Reduce muscle contraction and oxygen consumption associated with: Tetanus Drug overdose Status epilepticus · Eliminate movements that interfere with beside diagnostic or therapeutic procedures Common clinical settings Table 75. Commonly used non-depolarizing agents used and clinical settings where they are applied. If no neuromuscular blockade is present, all four shocks should result in muscular contraction of the same amplitude (height). Loss of the contraction from the fourth shock equates to a 70% neuromuscular blockade, with subsequent shocks three and two lost equalling up to 100% neuromuscular blockade. Paralysis can be transiently reversed with neostigmine or edprophonium but they should not be used routinely and only as needed. Reported side effects of neostigmine include arrhythmias, bronchospasm and the potential for acetylcholinesterase inhibitor to cause neuromuscular junction desensitization itself. Ultimately, weakness should resolve within a few days after discontinuation of a neuromuscular blockade agent. Ultimately, these compounds act as irreversible cholinesterase inhibitors, specifically for both plasma and acetylcholinesterase inhibitors.
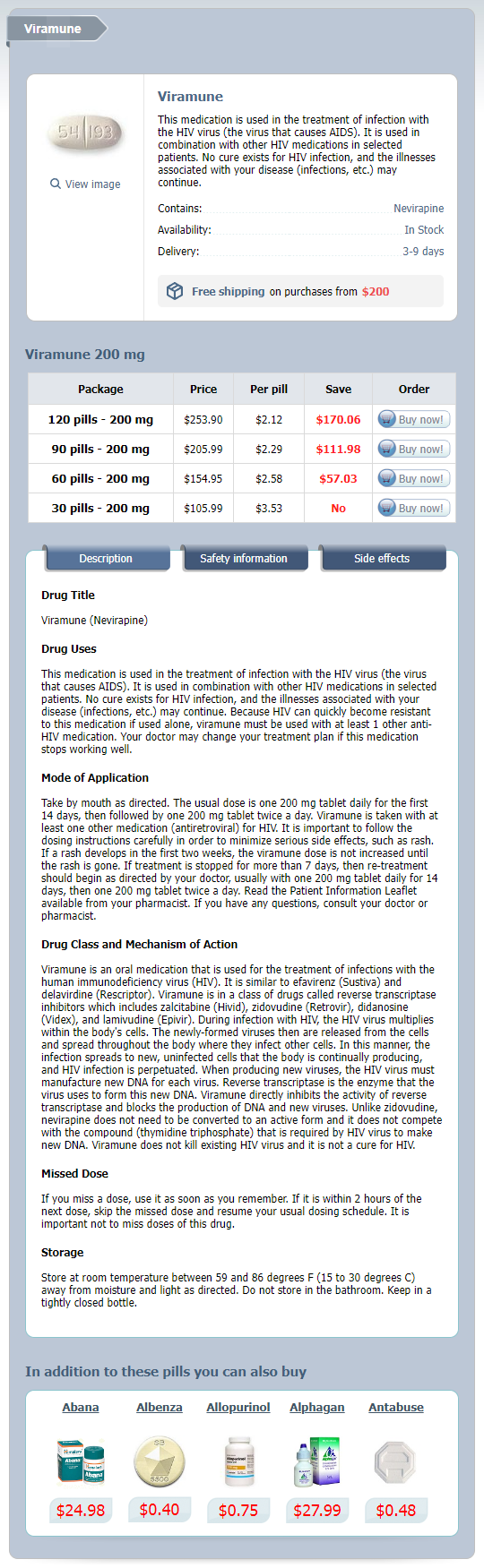
Viramune Dosage and Price
Viramune 200 mg
- 120 pills - $253.90
- 90 pills - $205.99
- 60 pills - $154.95
- 30 pills - $105.99
Establishing a successful immunosuppressive regimen in this setting can be quite difficult symptoms 2015 flu cheap 200 mg viramune with visa, and may require persistent use of the offending agent with an effort to maintain excellent blood pressure control. Patent foramen ovale Approximately 10% of the population has a patent foramen ovale. Though this is generally not of physiologic concern, it may pose a problem during the infusion of stem cells, particularly if a filter is not used. The primary causes of neurologic injury are (1) drug toxicity, (2) infection, (3) toxic metabolic encephalopathy, and (4) hemorrhage. It is convenient to consider neurologic injury occurring early after transplantation and that occurring late after transplantation separately. Early toxicity tends to be related to immediate problems with conditioning regimen effects. Preexisting neurological problems related to malignancy or metabolic encephalopathy are likely to increase the risk of immediate post-transplantation neurologic symptoms. Later events are often related to prolonged immunoincompetence and the effects of calcineurin inhibitors. The most common manifestations are tremor and burning palmar and plantar dysesthesias. However, headache, depression, confusion, somnolence, and nystagmus may also be observed. It is often observed in association with the new onset of hypertension, suggesting that there is cerebral edema due to abnormalities of pressure regulation in the posterior circulation. Many of the radiologic manifestations are similar to those seen in hypertensive encephalopathy. The most common pattern is white matter edema in the posterior circulation, which may or may not persist despite continued use of the drug. Although there are reports to the contrary, most clinicians believe that cyclosporine and tacrolimus are cross-reactive; 172 Neurologic complications 173 therefore, substitution of one for the other may not be useful. These microangiopathies are associated with evidence of hemolysis; typically, schistocytes are observed on the blood smear and there is a reduction in haptoglobin. Because of renal vascular involvement, hypertension and azotemia are generally concomitantly observed. Supportive medications · the use of narcotics, benzodiazepines, antihistamines, and antiemetics, often in combination, is probably the most frequent cause of altered mental status or seizures. Angioinvasive molds such as Aspergillus and Mucor may spread to the brain via hematogenous routes or by direct invasion from the sinuses. Malignancy · Leukemic or lymphomatous meningitis that occurs before the transplantation increases the risk of both relapse after the transplantation and the risk of nonspecific injury such as leukoencephalopathy. Therapy · Treatment of neurologic complications requires establishment of the correct diagnosis and specific management. Furthermore, there is reluctance to use carbamazepine, phenytoin, and some of the other anticonvulsants, because of concerns about their effects on incipient marrow recovery. Levetiracetam (Keppra), benzodiazepines, and gabapentin may be more useful because of their limited drug interactions and low risk of marrow toxicity. Late post-transplant period · Once the graft is functioning acceptably and the patient has recovered, the causes of neurologic injury shift. Early diagnosis and aggressive appropriate antiviral therapy such as acyclovir, ganciclovir, or foscarnet is often effective and can result in complete resolution of the infection. Varicella zoster virus reactivation can result not only in the well-known cutaneous manifestations but also (especially in severely immunocompromised patients) in severe abdominal pain without dermatomal vesicles. Highdose acyclovir can itself result in a reversible encephalopathy in susceptible patients. Post-herpetic neuralgia is occasionally observed and may be ameliorated with agents such as amitriptyline and gabapentin. Epstein Barr virus may be reactivated and result in lymphoproliferative disorders that have a predilection to extranodal dissemination, including the brain. Computed tomography scan and magnetic resonance imaging usually show the typically ring-enhancing lesions when the infection occurs late, in contrast to the less definitive appearance of these scans in the early post-transplant period. Some reports have demonstrated improvement with purine analog therapy, but there is no consistently valuable therapy for this disease. Efforts to improve muscle strength involve the use of supplemental immunosuppressants to allow dose reduction in corticosteroids. These can occur in almost any muscles, although the lower extremities and hands are the most common. The spasms may or may not be painful, and they are often triggered by muscular activity such as writing or typing. Typically, therapeutic trials with quinine, baclofen, valium, high-dose vitamin E, magnesium replacement, and potassium replacement are tried. Some manipulations seem to work for some people, but there is no consistently useful approach. Cystitis that occurs early (days 1 to 14) is usually caused by the conditioning agents, and is generally related to high-dose cyclophosphamide. The incidence of early cystitis is reduced with the use of aggressive hydration with forced saline diuresis or the administration of mesna for uroprotection. Mesna binds to an inactive metabolite of cyclophosphamide, acrolein, preventing urothelial inflammation.