VPXL
General Information about VPXL
VPXL is a natural complement that's specially formulated to stimulate the growth of the cells within the penis. It is a blend of natural extracts, vitamins, and minerals that work together to promote the natural development of the cavernous body of the penis. This unique mixture of ingredients is designed to increase the scale of the penis, improve sexual stamina, and improve total sexual efficiency.
In conclusion, VPXL is a protected, efficient, and all-natural answer for men trying to enhance their sexual efficiency and satisfaction. By stimulating the natural growth of cells in the penis, it might possibly improve the scale, girth, and stamina, resulting in a extra fulfilling intercourse life. Give VPXL a try to experience the difference it could make in your sexual health and confidence.
Additionally, VPXL is simple to make use of and requires no prescription. It could be conveniently ordered on-line and discreetly delivered to the doorstep, making it a perfect option for those who might feel embarrassed or uncomfortable discussing their sexual well being with a health care provider.
One of the principle reasons why VPXL stands out from other male enhancement merchandise out there is its all-natural method. Unlike other products which will contain synthetic or chemical components, VPXL makes use of solely the best natural extracts, nutritional vitamins, and minerals which may be secure and haven't any known unwanted effects.
VPXL contains quite lots of natural ingredients which are recognized for his or her capacity to enhance blood circulate, enhance testosterone levels, and enhance sexual efficiency. These elements work collectively to advertise the growth and growth of the cells within the cavernous body, resulting in a bigger and extra powerful erection.
Using VPXL has numerous benefits for males looking to improve their sexual well being and performance. The most evident profit is the increase within the measurement and girth of the penis. This can lead to a big enchancment in sexual pleasure and satisfaction for both companions.
Moreover, VPXL additionally helps to boost sexual stamina, allowing men to last longer in bed and satisfy their partner’s needs. This can result in a lift in confidence and shallowness, as men are in a place to perform at their greatest in the bed room.
VPXL is a revolutionary product that guarantees to boost the size and girth of the male organ, with out the necessity for surgical procedure or any invasive procedures. This all-natural complement is gaining recognition among men on the lookout for a safe and efficient method to improve their sexual efficiency and confidence in the bed room.
The key to VPXL’s effectiveness is its capacity to stimulate the pure development of cells in the cavernous physique of the penis. The cavernous physique is a spongy tissue that runs the length of the penis and is answerable for the engorgement of blood during an erection. As the cells in this tissue multiply and increase, the scale and girth of the penis additionally increase.
After injection of 3 mL (15 mg) erectile dysfunction causes nhs effective vpxl 9 pc, as can be expected, the warmer solution (lower density; hypobaric solution) caused a significantly higher maximum level. Of note, the variability of the spread also was clearly less than with the solution at room temperature (149). Heller and co-workers (150), using sophisticated measurement and mathematic models, calculated isobaric temperatures (temperature at which the local anesthetic is isobaric) for different local anesthetics of different concentrations. To get the advantages of isobaric solution, the temperature of the local anesthetic must be at this isobaric temperature. The baricity of the local anesthetic solution can be changed by adding either glucose (hyperbaric) or distilled water (hypobaric) to it. There are several commercially available hyperbaric solutions that contain glucose 50 to 80 mg/mL. The position of the patient after the injection is important when hyper- or hypobaric solutions are used. In the supine horizontal position, there is a tendency for anesthesia to spread to the level of thoracic kyphosis, which approximates the T4 level. If the hyperbaricity of the bupivacaine solution is decreased (glucose concentration of only 8 mg/mL; baricity of 1. The injection was made at the L3L4 interspace with patients in the sitting position. The range in the spread of anesthesia after the less hyperbaric solution was more limited (T5T9 versus T2T9) and was useful in predicting the spread of the block (152). Hyperbaric solutions are especially practical in small doses for saddle block and unilateral anesthesia. Hypobaric solutions have traditionally been used for rectal and perineal surgery when injected in the lateral decubitus or jack-knife position. There are no commercially available hypobaric solutions, and they must be mixed bedside. This is especially useful in patients who cannot lie on their side due to fractures (155). The hypobaric solutions must be used carefully, because when hypobaric bupivacaine (8 mL; 1. These responses are mediated by the combined effects of autonomic denervation and, with higher levels of neural blockade, the added effects of vagal nerve innervation. Spinal anesthesia always causes some degree of hypotension and reflex bradycardia because of reduction in cardiac output and systemic vascular resistance. Depending on the definition, the frequency of hypotension or bradycardia needing treatment varies; frequencies of hypotension of 8% to 30% and bradycardia of 10% to 15% have been reported. Unfortunately, sometimes these effects may lead to severe hypotension and asystole, leading to morbidity and even mortality in previously asymptomatic patients. In 1988, Caplan and co-workers searched through the insurance claims for major anesthetic mishaps and found 14 cardiac arrests-six of these fatal-occurring after normal spinal anesthesia in healthy patients (160). In a large survey from France from 1997, the incidence of cardiac arrest after spinal anesthesia was 26 in 40,640 cases (6. Later, in another survey from the same group, the incidence was slightly less at 2. A similar frequency was reported in a 20-year report from the Mayo Clinic, where the risk of cardiac arrest during spinal anesthesia was 2. Plasma levels of local anesthetics during spinal anesthesia are below those required to produce direct effects on the myocardium or on peripheral vascular smooth muscles (163), and the generalization that local anesthetics and vasoactive substances administered in small doses intrathecally lack direct cardiovascular effect remains accurate. Sympathetic denervation has great influence in the genesis of cardiovascular changes during spinal anesthesia. The spread of local anesthetic in the intrathecal space depends on the baricity (see chapter 11, Tables 11-2, 11-3). Arterial Circulation Sympathetic denervation produces arterial and, physiologically more important, arteriolar vasodilation, although vasodilation is not maximal. Vascular smooth muscle on the arterial side of the circulation retains a significant degree of autonomous tone following acute, pharmacologically induced sympathetic denervation. Veins and venules, with only a few smooth muscles in their walls, retain no significant residual tone following acute pharmacologic denervation, and so they can vasodilate maximally. Intraluminal hydrostatic pressure on the venous side of the circulation depends on gravity. If denervated veins lie below the level of the right atrium, gravity causes peripheral pooling of blood in these capacitance vessels. If the denervated veins lie above the level of the right atrium, gravity causes the blood to flow back to the heart. Sympathetic Denervation Because the level of sympathetic denervation determines the magnitude of cardiovascular responses to spinal anesthesia, it might be anticipated that the higher the level of neural blockade, the greater the change in cardio-circulatory parameters. However, the relationship is more complicated since, in the presence of partial sympathetic blockade, a reflex increase in sympathetic activity occurs in sympathetically intact areas. The result is vasoconstriction that tends to compensate for the peripheral vasodilation taking place in the sympathetically denervated areas. This can be seen in the changes in arterial pulse wave contours and in cutaneous blood flow in the upper extremities in the presence of low or midthoracic sensory levels of spinal anesthesia (164). During levels of spinal anesthesia high enough to produce total sympathetic denervation, cardiac output remains unchanged in normovolemic subjects as long as they are positioned with the legs elevated above the level of the heart. Heart rate characteristically decreases during spinal anesthesia in the absence of autonomically active drugs and medications. The bradycardia is due in part to blockade of preganglionic cardiac accelerator fibers arising from T1 to T4 during high. Indeed, in prospective studies, the incidence of episodes of bradycardia is increased if the sensory block level is T5 or higher (166,167). The bradycardia is also mediated by significant decreases in right atrial pressure and pressure in the great veins as they enter the right atrium.
The brachial plexus typically passes between the anterior and middle scalene muscles as it traverses from the neck to the arm in a lateral erectile dysfunction queensland 9 pc vpxl buy free shipping, 45-degree anterior, and caudad trajectory. Portions of the nerve roots occasionally pass directly through the anterior scalene muscle. This relationship provides valuable information if blood is aspirated during the supraclavicular approach. The second part of the axillary artery defines the anatomic positioning of the three cords. Despite some favorable preliminary reports, no extended-release local anesthetic preparation is commercially available (23). Ulnar nerve stimulation results in wrist ulnar deviation, little finger flexion, and thumb adduction. The brachial plexus is surrounded by key connective tissue, plus vascular and muscular structures that play important roles in upper extremity regional anesthesia. The concept of a substantial fascial sheath derived from the prevertebral fascia has become less relevant as information from modern imaging techniques question its importance. The trunks stack vertically and continue along a path that takes them posterior and lateral to the subclavian artery. Arrows denote the brachial plexus without an obvious surrounding sheath structure. Used with permission of the American Society of Regional Anesthesia and Pain Medicine (14). The possibility of compartment syndrome should be determined in consultation with the surgeon, since even analgesic blocks can mask early signs of impaired circulation. Prolonged sensory and especially motor block demand that patients are provided with protective slings and counseled to avoid sources of heat, cold, or trauma that could injure their insensate arm Using proper precautions, patients with anesthetized arms and/or continuous perineural infusions can be discharged home with minimal risk of injury (5,6,24). Most upper extremity surgery is amenable to anesthesia using the intermediate-acting local anesthetics lidocaine and mepivacaine. When prolonged analgesia is desired, bupivacaine generally results in 8 to 14 additional hours of analgesia than mepivacaine, or 2 to 6 more hours as compared with ropivacaine. Plain bupivacaine applied to the brachial plexus for surgical anesthesia is approximately 33% more potent than plain ropivacaine (bupivacaine 0. Thus, the reduction in cardiotoxicity inherent to ropivacaine can be compromised if larger doses of ropivacaine are used in an attempt to mimic the characteristics of a bupivacaine C3 C4 C5 Vertebral a. Needles placed too deeply can gain access to the subarachnoid, subdural, or epidural spaces. Local anesthetic can also enter the epidural space in a retrograde manner or enter the subarachnoid space via long dural root sleeves. Levobupivacaine and racemic bupivacaine share similar anesthetic characteristics when applied to the brachial plexus (27). Local Anesthetic Dosing For neuraxial local anesthetic blockade, total drug mass delivered to the target nerve is the most important factor in determining block effectiveness (28), yet its role is relatively inconsequential for brachial plexus blockade. Based on the studies of Vester-Andersen and colleagues (2932), there is little evidence that brachial plexus block characteristics can be improved by manipulating local anesthetic dosing regimens. Specifically, block onset, quality, and duration are unaffected by increasing the volume, concentration, and/or total dose of local anesthetic. These data imply that many brachial plexus blocks are performed with more local anesthetic than necessary. Because systemic local anesthetic toxicity is related to the total dose delivered (33), and local anesthetic neurotoxicity in animal models is concentration-dependent (34), logic dictates that attempts to enhance brachial plexus block by using a high volume of concentrated local anesthetic not only fails to significantly improve block quality, but conceivably places the patient at increased risk should an unintended intravascular injection or nerve injury occur. Drug mass should be especially reduced in patients with altered local anesthetic metabolism, such as the elderly and those with congestive heart failure or liver disease (33). The practice of alkalinizing local anesthetics to hasten block onset is beneficial in some neuraxial models, but not so for brachial plexus blocks. There is no evidence that alkalinizing local anesthetics improves other measures of block quality (14). Adjuvants A myriad of adjuvants have been proposed to improve block quality in terms of faster onset, denser block, and/or longer analgesia. Clinical evidence suggests that only two adjuvants unequivocally accomplish these goalsepinephrine and clonidine-and that their most dramatic effects occur only in conjunction with the intermediate-acting local anesthetics lidocaine and mepivacaine. This phenomenon is explained by the inherent analgesic duration of longacting local anesthetics being longer than the pharmacokinetic effects of the adjuvant. Epinephrine intensifies block quality, prolongs block duration, decreases systemic uptake of local anesthetic (and thus the rapid rise of plasma levels that is most associated with systemic toxicity), and acts as a marker of intravascular injection. Despite warnings to the contrary, there is no evidence that epinephrine significantly affects blood flow to end arteries, such as those in the fingers (36). Clonidine prolongs anesthesia and analgesia of intermediate-acting local anesthetics by approximately 50%. In the United States, the use of clonidine is somewhat restricted by its expense relative to epinephrine and its inability to act as an intravascular marker. All other adjuvants, including opioids, neostigmine, hyaluronidase, tramadol, and calcium channel blockers (14), and most recently dexamethasone (41) Unintended Local Anesthetic Destinations Intravascular Injection As compared to epidural anesthesia, unintentional intravascular injection during peripheral nerve block is five times more likely to result in seizures (45). This observation is particularly important in brachial plexus anesthesia, because injection into the nearby vertebral, carotid, or subclavian arteries transports local anesthetic directly to the brain. Predictably, seizure is approximately five times more likely to be associated with the interscalene or supraclavicular approaches than with the axillary approach (46). Intraarterial injections are characterized by immediate seizure activity that resolves quickly if the injection is promptly stopped, which emphasizes the importance of using a 1-mL local anesthetic test dose. Neuraxial Anesthesia Unintended neuraxial anesthesia can result from a malpositioned needle during the interscalene approach, although the frequency of this complication may be decreased with technique modification (48,49). The distance from the skin overlying the interscalene groove to the intervertebral foramen can be as little as 25 mm (49), and as little as 35 mm to the neuraxis (50). A needle placed too deeply can thus enter the epidural, subdural, or subarachnoid space.
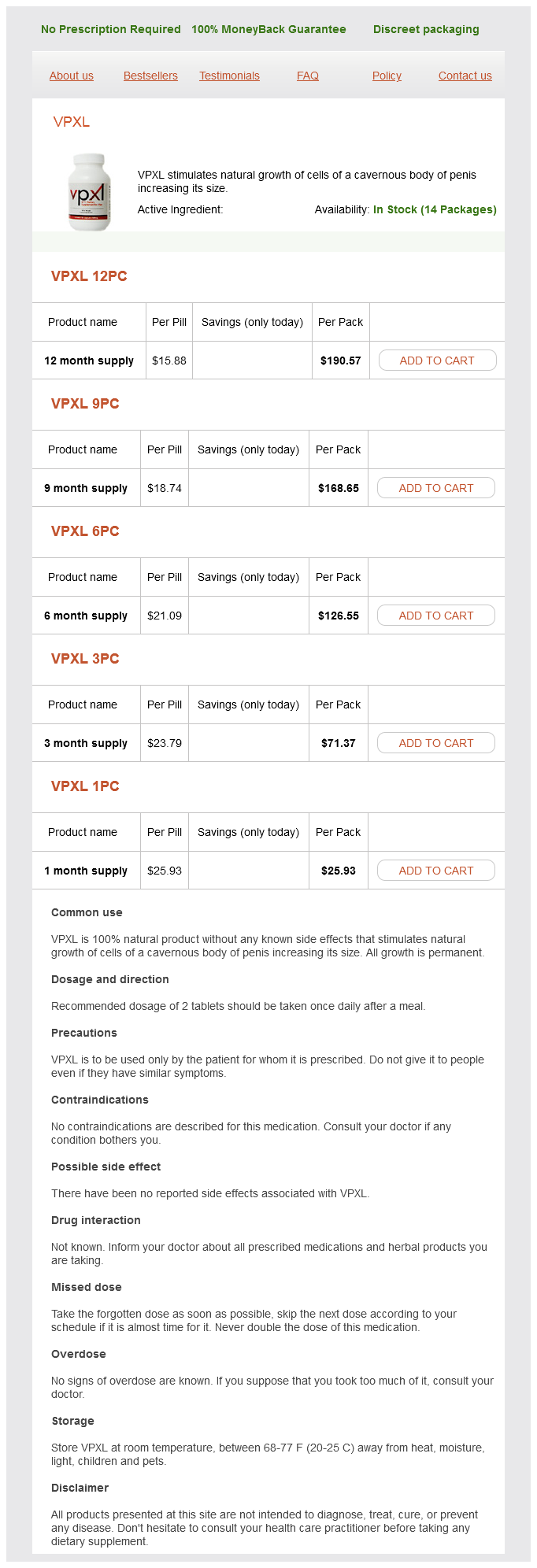
VPXL Dosage and Price
VPXL 12pc
- 12 month supply - $190.57
VPXL 9pc
- 9 month supply - $168.65
VPXL 6pc
- 6 month supply - $126.55
VPXL 3pc
- 3 month supply - $71.37
VPXL 1pc
- 1 month supply - $25.93
Scalp infiltration with bupivacaine plus epinephrine or plain ropivacaine reduces postoperative pain 28 erectile dysfunction operation purchase 6 pc vpxl amex. Incidence of shunting during carotid endarterectomy: Regional versus general anesthesia. General anaesthesia versus cervical block and perioperative complications in carotid artery surgery. Regional Block: A Handbook for Use in the Clinical Practice of Medicine and Surgery, 4th ed. Prospective, randomized comparison of deep or superficial cervical plexus block for carotid endarterectomy surgery. A comparison of superficial versus combined (superficial and deep) cervical plexus block for carotid endarterectomy: A prospective, randomized study. Superficial vs combined cervical plexus block for carotid endarterectomy: A prospective, randomized study. Superficial and deep cervical plexus block for carotid artery surgery: A prospective study of 1000 blocks. Baroreceptor control after cervical epidural anesthesia in patients undergoing carotid artery surgery. A comparison of two techniques for cervical plexus blockade: Evaluation of efficacy and systemic toxicity. Carotid endarterectomy using single injection posterior cervical paravertebral block. Incidence and clinical significance of hemidiaphragmatic paresis in patients undergoing carotid endarterectomy during cervical plexus block anesthesia. Incidence of dysphagia in patients undergoing carotid endarterectomy using deep and superficial cervical plexus block anesthesia. Bilateral vocal cord palsy during carotid endarterectomy under cervical plexus block. Acute respiratory failure after deep cervical plexus block for carotid endarterectomy as a result of bilateral re- 84. Clonidine decreases stress response in patients undergoing carotid endarterectomy under regional anesthesia: A prospective, randomized, double-blinded, placebo-controlled study. Mandibular nerve block in addition to cervical plexus block for carotid endarterectomy. Ciba Collection of Medical Illustrations, Volume I: the Nervous System, Part 1: Anatomy and Physiology. A comparison of anesthetic techniques for awake intubation in neurosurgical patients. Combined nebulization and spray-as-you-go topical local anaesthesia of the airway. British Thoracic Society Bronchoscopy Guidelines Committee, a Subcommittee of Standards of Care Committee of British Thoracic Society. Anatomical study applied to anesthetic block technique of the superior laryngeal nerve. A new application for superior laryngeal nerve block: Treatment or prevention of laryngospasm and stridor. A new application for superior laryngeal nerve block: Transesophageal echocardiography. Successful transesophageal echocardiography in an unsedated critically ill patient with superior laryngeal nerve blocks. Dissection tonsillectomy: Pattern of post-operative pain, medication and resumption of normal activity. Postoperative tonsillectomy pain in pediatric patients: Electrocautery (hot) vs cold dissection and snare tonsillectomy: A randomized trial. Tonsillectomy and adenoidectomy pain reduction by local bupivacaine infiltration in children. The effect of pre-incisional infiltration of tonsils with bupivacaine on the pain following tonsillectomy under general anesthesia. The effects of peritonsillar infiltration on the reduction of intraoperative blood loss and post-tonsillectomy pain in children. Tonsillectomy: A clinical study comparing the effects of local versus general anesthesia. A randomised controlled trial of the effect of regional nerve blocks on immediate post-tonsillectomy pain in adult patients. Remarks of certain dangers associated with the operation for the removal of tonsils and adenoids. Life-threatening upper airway obstruction after glossopharyngeal nerve block: Possibly due to an inappropriately large dose of bupivacaine Recent trends in utilization of procedures in otolaryngology-head and neck surgery. Operative times, postanesthesia recovery times, and complications during sinonasal surgery using general anesthesia and local anesthesia with sedation. Nasal fracture manipulation: A comparative study of general and local anaesthesia techniques. Efficacy of external fixation following nasal manipulation under local anaesthesia. Objective and subjective assessment of nasal obstruction in patients undergoing endoscopic sinus surgery. Effect of infraorbital nerve block under general anesthesia on consumption of isoflurane and postoperative pain in endoscopic endonasal maxillary sinus surgery. The tumescent facial block: Tumescent local anesthesia and nerve block anesthesia for full-face laser resurfacing.