Yasmin
General Information about Yasmin
What units Yasmin apart from different contraception options is its distinctive combination of hormones. The estrogen element in Yasmin is ethinylestradiol, a sort of synthetic estrogen, and the progestogen part is drospirenone, a fourth-generation progestogen. This mixture is what makes Yasmin a low dose and highly effective contraceptive. Ethinylestradiol permits for effective contraception by suppressing ovulation and thickening the cervical mucus, making it difficult for sperm to succeed in the egg. Drospirenone, on the opposite hand, helps to thin the lining of the uterus, making it much less probably for a fertilized egg to implant and develop.
Yasmin has a 21-pill pack that is taken every day for three weeks, adopted by a 7-day pill-free break when a lady will experience a withdrawal bleed, similar to a interval. After the break, the following pack is started, and the cycle continues. This makes it simple for girls to keep track of their tablet intake and ensures that they obtain the total advantages of the medicine.
Like any treatment, Yasmin additionally has a few possible unwanted facet effects, similar to nausea, breast tenderness, and changes in menstrual bleeding. These unwanted effects usually occur in the first few months of starting the tablet and tend to lower over time. Some women may also experience weight gain, headaches, and temper modifications, however these are not widespread.
One of the reasons why Yasmin is quickly changing into a popular selection among ladies is as a outcome of it is a highly effective contraceptive. When used correctly, Yasmin has a failure rate of less than 1%, making it some of the dependable contraception options available. However, like some other contraception method, Yasmin requires consistency and correct utilization to be effective. It is advised to take the pill on the similar time every day to take care of its effectiveness.
Yasmin is a contraceptive tablet that has been gaining reputation amongst women as a safe and reliable birth control method. It is a combination of two hormones, estrogen and progestogen, which work collectively to stop being pregnant. Yasmin has turn into a preferred selection for so much of girls because of its effectiveness, comfort, and minimal side effects.
It is considered one of the in style and effective contraception choices available available within the market.
In conclusion, Yasmin is a well-liked and highly effective contraception choice out there to girls. Its unique combination of hormones, convenience, and additional well being advantages make it a preferred alternative for lots of. With proper utilization and consistency, Yasmin offers ladies with the peace of thoughts and control over their reproductive well being. However, it's all the time advised to consult a healthcare skilled earlier than starting any birth control methodology to determine the greatest choice for an individual's specific needs.
Apart from being an effective contraceptive, Yasmin additionally has other well being benefits. It can help regulate menstrual cycles, cut back the symptoms of premenstrual syndrome (PMS), and decrease the danger of creating sure kinds of cancers like endometrial and ovarian most cancers. It may enhance pimples and hirsutism, a situation where ladies expertise excessive hair growth on their face and physique. This makes Yasmin not solely a contraceptive but in addition a helpful tool in managing different health points.
One of probably the most vital benefits of Yasmin is its comfort. Unlike different contraception methods similar to condoms or diaphragms, Yasmin doesn't require interruption during intercourse and doesn't intervene with sexual spontaneity. It also doesn't require any motion instantly earlier than or after sex, making it a most popular selection for a lot of ladies.
It is crucial to notice that Yasmin, like other birth control strategies, doesn't shield against sexually transmitted infections (STIs). To prevent STIs, it is recommended to use condoms along with Yasmin or consider different barrier methods of contraception.
The Beijing strains were likely to be resistant to all firstline antituberculous drugs and to ethionamide (Baranov et al birth control pills wikipedia yasmin 3.03 mg purchase with mastercard. Isolates from 45 children with isoniazid-resistant tuberculosis in South Africa, March 2003 to December 2005, were tested for ethionamide cross-resistance. Phenotypic ethionamide susceptibility was evaluated on Middlebrook 7H10 agar medium at a critical concentration of 5. Ethionamide resistance was present in 19 of 39 (49%) of isoniazid-resistant strains. Of the 21 isolates with a katG mutation that does not usually affect susceptibility to ethionamide, 6 (29%) were also ethionamide resistant, presumably due to a second undetected resistance mechanism. This was an important finding in this setting where clinicians rely heavily on ethionamide for children likely to have drug-resistant tuberculosis (Schaaf et al. However, while isolates resistant to thiacetazone are usually still susceptible to ethionamide, isolates resistant to ethionamide have a 70% chance of also being thiacetazone resistant (Crofon, 1969). Resistance to ethionamide (confirmed in the mouse footpad) has been detected in M. However, its structure is asymmetric, with the inner component composed of molecules specific to the family Mycobacteriaceae: arabinogalactan and mycolic acids. As its name suggests, InhA is also the molecular target of activated isoniazid (Banerjee et al. Activation of ethionamide is mediated by a monooxygenase encoded by the gene ethA (DeBarber et al. Another resistance mechanism for ethionamide was identified in the laboratory strain H37Rv linked to mutations in mshA. Although failure to produce mycothiol was non-lethal, these cells are ethionamide resistant. It is assumed that mycothiol production is somehow linked to the activation of ethionamide (Vilcheze and Jacobs, 2007). Ethionamide can be administered with food to avoid gastric irritation; co-administration of pyridoxine is recommended. Patients need to be encouraged to persist with treatment, as nausea and gastric irritation ofen improve with time. Doses and dosing intervals may need to be individualized according to patient acceptance. Pregnant and lactating mothers Ethionamide is rated category C for pregnancy, but most authorities suggest it not be used in pregnant women because of teratogenicity in rats and rabbits (Crofon, 1969; DailyMed, 2015). There are several reports of successful pregnancies despite treatment with regimens that have included ethionamide or prothionamide (Lessnau and Qarah, 2003; Shin et al. One study reported fetal malformations in 7 of 23 neonates whose mothers received ethionamide as part of a tuberculosis regimen during pregnancy, although two neonates also had Down syndrome (Potworowski et al. There are no data regarding the extent to which ethionamide is excreted in breast milk and it is recommended that it be given to lactating mothers only if the likely benefits outweigh the risks. Adults Ethionamide must be prescribed with other drugs known or likely to be active against the infecting strain. The film-coated version gives higher serum levels (DailyMed, 2015; KorthBradley et al. The recommended dose is 1520 mg/kg Only trace amounts of unchanged ethionamide are excreted in urine (DailyMed, 2015; Launay-Vacher et al. Dosage adjustment is not recommended until creatinine clearance falls below 10 ml/hour, and then to half the normal dose (Launay-Vacher et al. Ethionamide is not significantly removed by dialysis although for patients on dialysis, administration afer dialysis is recommended (Launay-Vacher et al. As with isoniazid, caution in patients with hepatic impairment is recommended together with periodic measurement of liver function 5. Ethionamide is contraindicated in patients with severely impaired liver function (DailyMed, 2015). Bioavailability Ethionamide is almost completely absorbed from the gastrointestinal tract, regardless of meals, and is not subject to significant first-pass metabolism. Protein binding is estimated at 30% but this drops significantly in malnourished patients (Holdiness, 1984). The authors commented that multidrug, multiday regimens appear to increase Cmax for prothionamide compared with single-dose measurements. Subgroup analysis showed that Cmax was higher in group 2 compared with group 1, likely due to differences in the effect of the drug distribution or metabolism of moxifloxacin compared with levofloxacin (Park et al. The clinical significance of this difference is uncertain, especially as there is some evidence that prothionamide performs better than ethionamide for leprosy (Fajardo et al. Film-based coated capsules give higher and more stable levels than sugar-coated formulations (Korth-Bradley et al. Ethionamide distributes rapidly and widely to all tissues and fluids, with an apparent volume of distribution of 93. Plasma and tissue levels are similar once steady state is reached (Holdiness, 1984). Ethionamide is detectable in appreciable amounts in alveolar macrophages and epithelial lining fluid (Conte et al. Clinically important pharmacokinetic and pharmacodynamic features Clinical efficacy has been associated with an ethionamide serum drug level of 23 g/ml, which is near Cmax of standard tolerable doses (Kam et al. Doses of prothionamide were either 250 mg twice daily (for body weight < 59 kg) or 500 mg twice daily (for body weight > 50 kg). More than 59% of prothionamide levels measured during this study were below an accepted target concentration of 15 g/ml. The pharmacokinetics of ethionamide in children 3 months13 years undergoing treatment for resistant tuberculosis was studied in Cape Town, South Africa, September 2009 to May 2010.
Reinoso-Martín C birth control pills kinds best purchase for yasmin, Schüller C, Schuetzer-Muehlbauer M, Kuchler K (2003) the yeast protein kinase C cell integrity pathway mediates tolerance to the antifungal drug caspofungin through activation of Slt2p mitogenactivated protein kinase signaling. A Ser678Pro substitution in Fks1p confers resistance to echinocandin drugs in Aspergillus fumigatus. Phagocytosis by human neutrophils is stimulated by a unique fungal cell wall component. Pharmacokinetics and safety of caspofungin in neonates and infants less than 3 months of age. Safety of the concomitant use of caspofungin and cyclosporin A in patients with invasive fungal infections. New semisynthetic pneumocandins with improved efficacies against Pneumocystis carinii in the rat. Combination of voriconazole and caspofungin as primary therapy for invasive aspergillosis in solid organ transplant recipients: a prospective, multicenter, observational study. Pathobiology of Pneumocystis pneumonia: life cycle, cell wall and cell signal transduction. Combination therapy with amphotericin B lipid complex and caspofungin acetate of disseminated zygomycosis in diabetic ketoacidotic mice. A Candida biofilm-induced pathway for matrix glucan delivery: implications for drug resistance. Development of caspofungin resistance following prolonged therapy for invasive candidiasis secondary to Candida glabrata infection. Efficacy of caspofungin addition to trimethoprim-sulfamethoxazole treatment for severe pneumocystis pneumonia in solid organ transplant recipients. A randomized doubleblind study of caspofungin versus amphotericin for the treatment of candidal esophagitis. A randomized doubleblind study of caspofungin versus fluconazole for the treatment of esophageal candidiasis. Elevated chitin content reduces the susceptibility of Candida species to caspofungin. Caspofungin treatment of Aspergillus fumigatus results in ChsG-Dependent upregulation of chitin synthesis and the formation of chitin-rich microcolonies. Pharmacokinetics, safety, and tolerability of caspofungin in children and adolescents. Systematic review and meta-analysis of the tolerability and hepatotoxicity of antifungals in empirical and definitive therapy for invasive fungal infection. Caspofungin is less nephrotoxic than amphotericin B in vitro and predominantly damages distal renal tubular cells. Dynamic, morphotypespecific Candida albicans beta-glucan exposure during infection and drug treatment. Pharmacodynamics of caspofungin in a murine model of invasive pulmonary aspergillosis: evidence of concentration-dependent activity. Attenuation of the activity of caspofungin at high concentrations against candida albicans: possible role of cell wall integrity and calcineurin pathways. Caspofungin dose escalation for invasive candidiasis due to resistant Candida albicans. Lack of response in severe pneumocystis pneumonia to combined caspofungin and clindamycin treatment: a case report. A prospective, multicenter study of caspofungin for the treatment of documented Candida or Aspergillus infections in pediatric patients. Similar to other echinocandin compounds approved for clinical use (caspofungin and anidulafungin), the addition of a modified N-linked acyl lipid side-chain to the cyclic hexapeptide nucleus improves antifungal potency, likely through anchoring the compound to the phospholipid bilayer of the fungal cell membrane. Depletion of this integral glucan polymer leads to osmotic instability, cell lysis, and cell death. Micafungin is primarily effective against Candida and Aspergillus species, with marginal activity against other molds and basidiomycetes likely due to differences in the structural components of the fungal cell wall or compensatory mechanisms in these species. Routine susceptibility A summary of the in vitro activity of micafungin against various fungi is shown in Table 147. The clinical significance of this intrinsically reduced susceptibility is questionable, as clinical trial data suggests patients infected with these strains can be treated successfully with standard doses. As such, care should be taken when utilizing micafungin for treatment of these species. Micafungin lacks clinically meaningful activity against basidiomycetes, including Trichosporon, Cryptococcus neo formans, and Cryptococcus gattii, even though they possess a beta-glucan synthase enzyme which is sensitive to echinocandin inhibition (Maligie and Selitrennikoff, 2005). The inherent resistance observed in these fungi is thought to be a result of compensatory stress response pathways. However, micafungin monotherapy should not be considered a viable treatment option for infections caused by these species. This differential activity is likely explained by changes in beta-1,3-glucan content of the fungal cell wall that occurs between these two states. Micafungin Fungi Yeasta Candida albicans Candida parapsilosis Candida glabrata Candida tropicalis Candida krusei Candida guillermondii Candida lusitaniae Candida dubliniensis Candida kefyr Candida famata Cryptococcus neoformans Endemic fungi (yeast form)b H. In animal models, all echinocandins are effective at improving survival in otherwise lethal models of aspergillosis, even though high counts of Aspergillus can be cultured from tissue (Petraitis et al. These data are in accord with echinocandins possessing fungistatic activity against Aspergillus species (Denning, 2003). Data regarding the efficacy of micafungin in experimental models of infection are scarce. However, as caspofungin has been shown to be only marginally effective against Coccidioides immitis and Histoplasma capsulatum in experimental animal models, monotherapy with echinocandins should not be considered for the treatment of dimorphic fungal infections (Gonzalez et al. The limited treatment efficacy of echinocandins can be explained by the fact that glucan synthase target for echinocandin activity is expressed only during the cystic but not during the trophic life cycle of Pneumocys tis, thus limiting the rate of fungal clearance (Schmatz et al.
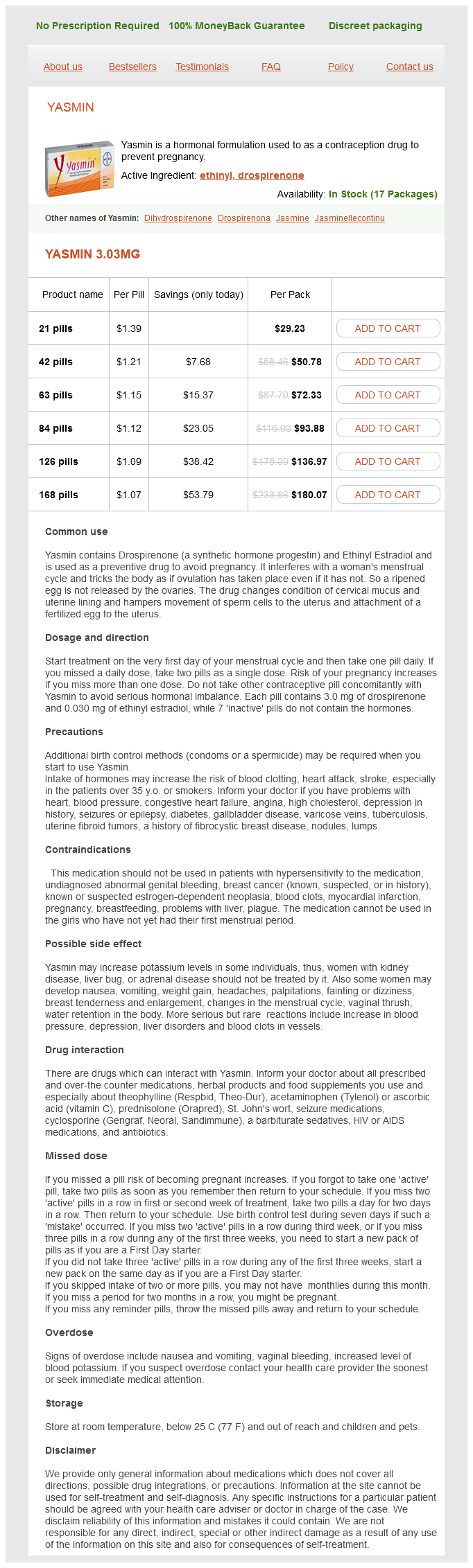
Yasmin Dosage and Price
Yasmin 3.03mg
- 21 pills - $29.23
- 42 pills - $50.78
- 63 pills - $72.33
- 84 pills - $93.88
- 126 pills - $136.97
- 168 pills - $180.07
Importantly birth control for women over 40 who smoke 3.03 mg yasmin fast delivery, population-based studies have shown that diabetics receiving moxifloxacin have a significant risk of some dysglycemia (Chou et al. This, however, was thought not to be clinically significant (Stass and Kubitza, 2001b). A single case of hyponatremia in an elderly patient receiving moxifloxacin has also been reported (Mussig et al. Exclusion criteria consisted of any previous diagnosis of uveitis or a uveitis-associated systemic illness. The hazard of a uveitis diagnosis after a fluoroquinolone prescription compared with a beta-lactam prescription was assessed using multivariate regression with Cox proportional hazards models. Thus this study did not support an association between oral fluoroquinolone use and uveitis. Instead, the authors identified an association between oral fluoroquinolone use and the risk for uveitisassociated systemic illnesses, which is a possible source of bias that could explain the findings of previous studies (Sandhu et al. Other clinical indications in which moxifloxacin may be considered for use include diabetic foot infections, intraabdominal sepsis, pelvic inflammatory disease, and tuberculosis. Acute bacterial sinusitis Although it remains difficult to determine which patients should receive antimicrobial therapy, antibacterials are considered to be beneficial for the treatment of known or suspected bacterial episodes of sinusitis. The fluoroquinolones have excellent activity against the most common organisms causing acute bacterial sinusitis: H. Although fluoroquinolones should not be used as first-line therapy in acute bacterial sinusitis, they appear to be highly effective as second-line agents. Moxifloxacin 400 mg daily was compared with cefuroxime axetil 250 mg twice daily in 542 patients with acute bacterial sinusitis (radiographic evidence plus signs and symptoms for > 7 days and < 4 weeks). After 10 days the response rate for moxifloxacin and cefuroxime axetil was 90% and 89%, respectively (Burke et al. Ophthalmic toxicity Case reports have suggested that systemic moxifloxacin use may lead to uveitis (Hinkle et al. The authors assessed cohorts from ambulatory care centers across the United States, which 7. Clinical uses of the drug 2095 the same drug regimens, success rates for moxifloxacin were significantly higher than for those receiving cefuroxime axetil: 96. Moxifloxacin (400 mg daily) has also been compared with amoxicillinclavulanate (875 mg bid). Clinical cure at the test-of-cure visit (1421 days after therapy) was reported for 85% versus 82% of patients, respectively (Rakkar et al. Similarly, 575 patients with acute bacterial sinusitis were randomized to receive oral moxifloxacin (400 mg for 7 days) or amoxicillinclavulanate (500/125 mg three times daily for 10 days). This study also showed equivalence, with clinical success and bacteriological eradication for moxifloxacin and amoxicillinclavulanate of 93. In a pooled analysis of two clinical open-label sinusitis trials, the efficacy of moxifloxacin against penicillin-susceptible and penicillin-resistant S. This study found a clinical and bacteriological success at test-of-cure visit (2137 days after therapy completion) of 93. Another study comparing moxifloxacin and trovofloxacin revealed equivalent clinical outcomes; however, dizziness was significantly more common in the trovofloxacin group (Baz et al. In a recent large prospective, noncontrolled, multicenter observational cohort study of patients with acute sinusitis, moxifloxacin was an effective and well-tolerated treatment option (Mosges et al. Thus moxifloxacin is effective for the treatment of acute bacterial sinusitis, but clinicians must use this and other fluoroquinolones judiciously and appropriately to avoid the unnecessary emergence of resistance among common pathogens. Acute bacterial exacerbations of chronic obstructive pulmonary disease In a multinational, randomized double-blind study involving 750 patients, the safety and efficacy of a 5-day course of moxifloxacin (400 mg daily) was compared with that of a 7-day course of clarithromycin (500 mg orally twice-daily). This study showed clinical equivalence of the two regimens, but moxifloxacin was bacteriologically superior to clarithromycin, with bacteriological response rates at 7 days post treatment of 77% and 62%, respectively (Wilson et al. Moxifloxacin (400 mg daily for 5 days) has been compared with azithromycin (500 mg qd for 1 day, then 250 mg qd for 4 days) in a randomized, controlled trial involving 567 patients. Moxifloxacin was found to be clinically and bacteriologically equivalent to azithromycin, with eradication rates at test-of-cure for H. Clinical success (resolution and improvement) was equivalent with moxifloxacin versus standard therapy (88% and 83%) at 710 days after the end of therapy. However, moxifloxacin was associated with a superior rate of clinical cure (resolution of symptoms to baseline) compared to standard therapy (71% vs. Furthermore, all subgroup analyses revealed a statistically significant reduction of 1825% in time to recovery with moxifloxacin compared with comparators (Miravitlles et al. Moxifloxacin (400 mg daily for 5 days) has also been compared with levofloxacin (500 mg daily for 7 days) in a prospective, randomized, double-blind clinical trial. In this study of 563 patients, moxifloxacin was found to be clinically and bacteriologically equivalent to levofloxacin (clinical success and bacterial eradication of moxifloxacin and levofloxacin 91% vs. Eradication rates were 75% with moxifloxacin versus 30% with placebo at 2 weeks (p = 0. Bacterial persistence at 8 weeks was still higher (not significantly) in the placebo arm (5/20 [25%] vs. Patients were randomized to moxifloxacin 400mg daily for 5 days or placebo, and the treatment was repeated every 8 weeks for a total of six courses. Intermittent pulsed therapy reduced the 2096 Moxifloxacin odds of exacerbation in the intention-to-treat population by 20%, by 25% in the per-protocol population, and by 45% in patients who had mucopurulent sputum at baseline. Significantly, large increases in antibiotic resistance were seen in all treatment groups, and most adverse events were reported in the moxifloxacin arm (Brill et al. Community-acquired pneumonia Moxifloxacin displays excellent activity against the most important respiratory pathogens, including Gram-negative bacilli, S.