Zantac
General Information about Zantac
While Zantac is primarily used for the therapy of ulcers, it can additionally be prescribed as a preventative measure for these who may be at risk for developing ulcers. This contains people who're taking non-steroidal anti-inflammatory medication (NSAIDs) corresponding to aspirin or ibuprofen, which can irritate the lining of the abdomen and increase the chance of ulcers.
Zantac belongs to a class of drugs referred to as H2 blockers, which work by decreasing the amount of acid produced in the stomach. This, in flip, helps to guard the fragile lining of the abdomen and intestines, allowing ulcers to heal and preventing new ones from forming.
In conclusion, Zantac is a widely used and effective medicine for the remedy and prevention of ulcers within the stomach and intestines. By lowering acid manufacturing, it helps to alleviate symptoms and allows the body to heal itself. It is necessary to follow a physician's directions and to report any unwanted facet effects experienced while taking this treatment. With correct use, Zantac may help individuals find aid from the discomfort and ache related to ulcers.
The energetic ingredient in Zantac, ranitidine, works by blocking histamine receptors in the abdomen. Histamine is a chemical that stimulates the discharge of acid, so by blocking its results, Zantac successfully reduces acid production. This permits the body's pure therapeutic course of to happen and helps to relieve discomfort and pain associated with ulcers.
Like with any medicine, there are potential side effects associated with Zantac. These might embody headaches, dizziness, diarrhea, or constipation. In rare cases, it may also cause extra severe unwanted side effects such as liver issues or low levels of white blood cells. It is essential to debate any potential unwanted effects with a physician and to comply with the prescribed dosage carefully to attenuate these dangers.
In addition to treating ulcers, Zantac has also been confirmed to be efficient in treating acid reflux disease signs similar to heartburn and indigestion. These circumstances happen when the acid in the stomach travels back up into the esophagus, inflicting a burning sensation. By lowering the quantity of acid in the stomach, Zantac may help to relieve these uncomfortable signs.
Zantac, additionally known by its generic name ranitidine, is a drugs generally prescribed for the remedy and prevention of ulcers in the stomach and intestines. Ulcers are painful sores that may develop in the lining of these organs and can be caused by a selection of factors, together with extreme acid production.
The use of Zantac has been permitted by the U.S. Food and Drug Administration (FDA) since 1983 and is available both over-the-counter and by prescription. It is taken into account a secure and effective selection for the therapy of ulcers, in addition to other conditions similar to gastroesophageal reflux disease (GERD) and Zollinger-Ellison syndrome, which causes extreme acid manufacturing within the stomach.
Zantac is out there in both pill and syrup kind, making it easy to take for people who could have issue swallowing pills. It is usually taken once or twice a day, with or without food, relying on the severity of the condition and the individual's response to treatment. The dosage and duration of remedy could vary relying on the precise situation being handled and the patient's medical historical past.
Blood 2006; 107: 2776-3 deVeber G gastritis diet and exercise quality 150 mg zantac, Andrew M, Adams C, et al; the Canadian Pediatric Ischemic Stroke Study Group Cerebral sinovenous thrombosis in children. Imaging of cerebral venous thrombosis: current techniques, spectrum of findings and diagnostic pitfalls. Congophilic deposits characteristic of associated with large hemorrhages and amyloid angiopathy. It practically detects 100% of hematomas, except when <1 cm, located in the posterior fossa or in those patients with severe anemia (hematocrit <20) [16]. Location Topography considers the epicentre as the site where the hematoma originates. Volume Hematoma volume is an important predictor of mortality, making its measurement necessary. In the hyperacute stage (first 4 hours), the extravasated blood has not yet formed a clot, producing an irregular hyperdense collection within the cerebral parenchyma. In the acute phase (5 to 72 hours), a pre-existing hematoma becomes dense due to clot formation [21]. The sign consists of a small "spot" or "point" inside the hematoma and suggests active bleeding from Charcot microaneurysms or from vessels with vascular damage [22]. Angiography is also recommended in patients with primary intraventricular hemorrhage and in those with perisylvian sulcal or fronto-orbital hemorrhage to dismiss the presence of aneurysms [16,23]. It also helps to evaluate the dam899 Intensive Care in Neurology and Neurosurgery age associated with the hematoma and to define its possible mechanism, for example: arteriovenous malformation (heterogeneous image with empty signals and calcifications), intratumoral bleeding or cavernous angioma [16,23-27]. Lobar microbleeds have been related to amyloid angiopathy, whereas ganglionar microbleeds have been associated with hypertension [28]. Histopathologic Study In all patients with hematoma evacuation or autopsy, it is mandatory to confirm the etiologic diagnosis. Charcot-Bouchard aneurysm evidenced from tissue obtained after putaminal hematoma evacuation. A = lobar B = basal ganglia C = thalamus D = protuberance E = cerebellum 900 Diagnosis and Treatment of Intracerebral Hemorrhage the most common sites for arteriolar damage are the bifurcation of penetrating vessels such as the lenticulostriatal, the thalamic perforating arteries, and the brainstem penetrating arterioles. When all diagnostic procedures are negative, the etiology is considered cryptogenic or idiopathic. Irruption of blood in to the brain destroys the parenchymal tissue, alters intracerebral homeostasis, triggers an increase in local pressure with mass effect, leading to displacement of vectors and distortion of intracranial structures. In addition, the hemorrhage by itself is the source of three other deleterious events: cellular death by necrosis and apoptosis, inflammation and vasogenic edema [32-42]. In 38% of patients, hematoma continues to grow after the initial event in the first 3 hours, which is associated with neurological deterioration and poor prognosis. Other risk factors or conditions contributing to hematoma growth are issues of meticulous analyses, both in clinical and molecular scenarios, and they represent an opportunity area for therapeutic interventions. Alcohol abuse, hyperglycemia, reduced prothrombin activity, hypofibrinogenemia and liver diseases have all been associated with this phenomenon [43,46]. It appears after 24 hours around the hematoma and reaches its major expression at the fourth day, before slowly decreasing [32,33,35-37,39-42,45]. For surgical approaches, patient age and co-morbidities are important issues, as are the neurological status at emergency room arrival, hematoma location and volume, displacement of midline structures, ventricular irruption, hydrocephalus, etiology and patient or family end-of-life preferences [1,12,23]. The decision whether to institute endotracheal intubation is based on clinical judgment, since its delay aggravates the pre-existing neurological damage and increases morbidity and mortality as a result of the secondary insult from hypoxemia, hypercapnia or aspiration pneumonia [11,39,43,44,51-59]. Hypotension needs to be immediately corrected with iso- or hypertonic fluids, colloids and amines such as phenylephrine, dopamine or norepinephrine to maintain adequate cerebral perfusion pressure. The electrocardiogram and chest x-ray are useful to evaluate cardiovascular function in patients with or without a history of arterial hypertension in the preoperative work-up, and also to detect early non-neurological complications (arrhythmias, pneumonia) [23]. Under no condition should an unstable patient be transferred for complementary studies. It is recommended to establish a central venous route, high calibre peripheral pathways and an arterial line. The advantages of this approach are that it allows for the precise monitoring of volemia and average arterial tension for easy se- 904 Diagnosis and Treatment of Intracerebral Hemorrhage rial extraction of blood samples without the need for extra procedures on the patient; it also helps when volume expanders are required, colloids, mannitol, plasma or total blood without interfering with the simultaneous administration of sedatives, analgesics, antihypertensives or other drugs. Under no circumstances (except in hypoglycemia) should hypotonic solutions such as dextrose or Ringer´s lactate be given because they worsen the cerebral edema, promote the synthesis of neurotoxic neurotransmitters such as glutamate, produce local tissue acidosis (a powerful stimulator of cerebral vasodilatation), and increase cerebral blood volume with elevation of intracranial pressure [23,51,58]. Fever must be aggressively treated because of its deleterious effects on neurons and the blood-brain barrier: stimulation of the production of free radicals and elevation of excitatory amino acid levels. Fever also increases the cerebral metabolic demands of oxygen, with repercussions on intracranial pressure, in addition to decreasing the seizures threshold [60]. The authors recommend its management by physical means, thermal blankets, and the administration of acetaminophen in doses of up to 2 g daily when rectal temperature exceeds 37. This practice is in line with recent results of a multicenter study on acetaminophen in stroke [63]. If a tracheotomy is created, independently of the time at which it is indicated, it should be done by the percutaneous route. Additionally, and despite recent controversies, the head should be maintained 30 degrees from the horizontal plane in a "neutral" position, i. Other equally important measures [58] include the use of artificial eye drops and frequent eyewashes, frequent oral hygiene with clorhexidine or other similarly effective mouthwashes. Stress ulcer prophylaxis can be achieved with H2 blockers, proton pump inhibitors or contact antacids such as sucralfate. Deep venous thrombosis prophylaxis can be achieved by using elastic bandages or pneumatic sleeves with sequential compression. Specific Measures Normoglycemia the strict control of glycemia levels is associated with multiple benefits, including the prevention of osmotic diuresis, maintenance of neutrophil and macrophage function, reduced free radicals production, increased nitric oxidase production and improved erythropoiesis [44,54,55,58]. Godoy and his group recommend strict glycemia monitoring and treatment with current insulin therapy if glycemia >150 mg/ dl levels [64-66]. Management should never be delayed while waiting for coagulation tests, the combined use of all available therapeutic tools being frequent in daily practice.
N Engl J Med 2008; 5: 2447-56 585 31 A Critical Point of View in the Management of Intracranial Hypertension: Are All Therapeutic Tools Evidence Based Thomas Lescot 1 gastritis symptoms back pain trusted 300 mg zantac, Lamine Abdennour 1, Louis Puybasset 1 1 Neurosurgical Unit, Department of Anesthesiology and Critical Care Pitié-Salpêtrière Hospital, Assistance Publique, Hôpitaux de Paris, Université Pierre et Marie Curie, Paris, France 31. A large, prospectively collected database study published in 1991 by Marmarou et al. After trauma, the traumatised brain is characterised by a marked pathophysiological heterogeneity: ischemic areas (cytotoxic edema) coexists with areas with blood-brain barrier disruptions (vasogenic edema), contusions, and normal brain parenchyma. Benzodiazepines, especially midazolam, are administered in combination with morphine or derivatives such as sufentanil. While they are particularly suitable in the neurological intensive care unit, they are unable to depress brain electrical activity even at high doses, present a long duration of action and a plateau effect. However, the potential risk with using propofol is the feared propofol infusion syndrome. This syndrome, characterized by multiorgan failure, has a high incidence in sepsis or septic shock, which are therefore contraindications to propofol administration. It is mandatory to stop propofol in case of metabolic acidosis (with or without lactates), hyperkalemia, renal insufficiency, rhabdomyolysis or triglyceride level >5 mmol/l [10]. The occurrence of refractory brain hypertension during the first days following the onset of head trauma often requires therapeutic escalation with such therapeutics as neuromuscular blockers, hypothermia and thiopental, all of which have a high potential to deteriorate lung status further through mechanical effects or direct immunosuppressive effects. The authors concluded that barbiturate therapy significantly improved clinical outcome on the assumption that their patients would have otherwise died. Continuous barbiturate infusion is also known to produce immunosuppression by inhibiting lymphocyte function [14], affecting neutrophil function and depressing humoral immune response through a decrease in immunoglobulin production [15]. The use of barbiturates is, by itself, a statistical predictor of an increased risk of pneumonia [11]. Such a decrease in cerebral blood volume also occurs when the mean arterial pressure is increased. It is likely that local pH rather than local carbon dioxide is the mediator of tone regulation. The mediator cascade that links extracellular pH to cerebral vascular tone is complex and interrelated, the final mediator being intracellular calcium. Acute hypocapnia significantly decreased PbrO2, indicating the risk of secondary ischemic damage during hyperventilation in severely head-injured patients. The most recent guidelines of the Joint Committee on Trauma and Critical Care of the American Association of Neurologic Surgeons indicate that aggressive or prophylactic hyperventilation must be avoided in patients with severe head trauma [19]. This 589 Intensive Care in Neurology and Neurosurgery therapy is simple, cost effective and overrides the often serious systemic complications related to drug or physical therapies, especially those induced by barbiturates and hypothermia. Drain placement might be technically difficult, and can be complicated by cerebral contusion or ventriculitis [21]. As a result, it could be proposed to reserve the use of osmotic agents for patients presenting a small volume of contusion. There is current evidence to support the concept that hypotension is deleterious for the traumatised brain. This discrepancy could be linked to the presence of contusions: preserved autoregulation is more frequently observed in patients with few contusions [32]. Outcome after hypothermia can be optimised when proper indications, techniques for implementation, as well as management procedures and their enforcement are followed. A rigorous and effective application cannot be conceived outside specialized units with experienced teams. A decrease in brain metabolism associated with anti-inflammatory effects is the main mechanism of action attributed to hypothermia treatment. Kalemia must be strictly controlled during the ascending and descending changes in body temperature. Of note is that the implementation of hypothermia has been recently facilitated with the availability of automatic cooling blankets and specially designed catheters. Increase sedation and add propofol (measure pH daily and serum triglycerides every 48 h stop propofol infusion if metabolic acidosis, hyperkalemia, renal insufficiency, rhabdomyolysis or triglyceride level >5 mmol/l). Contusion volume >20 ml · Methylprednisolone 120 mg every 12 h (3 days) · Consider albumin administration 5. In a model of ischemia-reperfusion in an isolated guinea pig heart model, albumin more effectively prevented fluid extravasation than crystalloid or artificial colloid. The main flaws of this study were the a posteriori analysis and the slight imbalance between the two groups. After trauma, the traumatised brain is characterised by pathophysiological heterogeneity. One and the same therapy for the various different types of brain trauma is not efficient. Effect of intracranial pressure monitoring and aggressive treatment on mortality in severe head injury. Risk factors for pneumonia and fatality in patients receiving continuous mechanical ventilation. Prolonged thiopentone infusion for neurosurgical emergencies: usefulness of therapeutic drug monitoring. Regional cerebral plasma volume response to carbon dioxide using magnetic resonance imaging. The use of hyperventilation in the treatment of plateau waves in two patients with severe traumatic brain injury: contrasting effects on cerebral oxygenation. Resolution of brain edema in severe brain injury at controlled high and low intracranial pressures. J Neurosurg 1985; 63: 43-8 594 A Critical Point of View in the Management of Intracranial Hypertension 24. Effects of mannitol bolus administration on intracranial pressure, cerebral extracellular metabolites, and tissue oxygenation in severely head-injured patients.
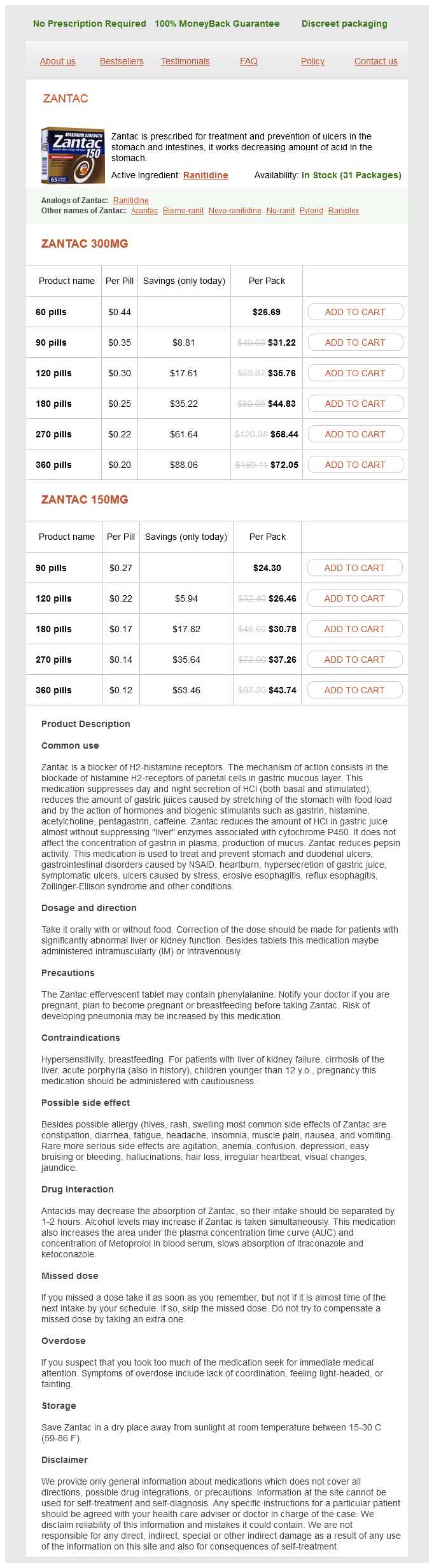
Zantac Dosage and Price
Zantac 300mg
- 60 pills - $26.69
- 90 pills - $31.22
- 120 pills - $35.76
- 180 pills - $44.83
- 270 pills - $58.44
- 360 pills - $72.05
Zantac 150mg
- 90 pills - $24.30
- 120 pills - $26.46
- 180 pills - $30.78
- 270 pills - $37.26
- 360 pills - $43.74
Although some authors suggest random basal cortisol levels <25 µg/dl or 36 µg/dl gastritis diet japan cheap zantac 300 mg fast delivery, a cortisol concentration <15 µg/dl (410 nmol/l) are acceptable as a diagnostic value for adrenal insufficiency in critically ill brain-injured patients. In patients lower values and clinical findings consistent with adrenal insufficiency, there is no need for further stimulation testing in routine clinical practice. As mentioned, differentiation between primary and secondary adrenal failure is not warranted in critically ill brain-injured patients in routine clinical practice. The recommended value of 25 µg/dl (690 nmol/l) seems more realistic as a cut-off higher than that used in an outpatient setting because the peaks achieved during this test are, on average, higher than in patients without stress or severe illness. Algorithm for the management of adrenal insufficiency in brain-injured patients in the acute phase. But a recent study showed no positive correlation between this criterion and survival. Therefore, we do not recommend using this criterion in the diagnosis of adrenal insufficiency in patients with acute brain injury. Measurement of free cortisol has been suggested as a more accurate assessment of adrenal output. Several research groups have recently investigated the use of salivary cortisol concentration as a surrogate marker for serum free cortisol levels. Salivary cortisol measurement is simple to obtain and easy to measure in most laboratories. The data on the utility of salivary cortisol in critically ill brain-injured patients are currently insufficient. It is generally agreed, however, that therapy should be provided for patients with confirmed hypoadrenalism in whom clinical circumstances, such as hypotension, hyponatremia and hypoglycemia, warrant intervention. In patients with adrenal insufficiency as determined according to previously discussed criteria. Dexamethasone or methylprednisolone at equivalent hydrocortisone doses could be used as alternatives. It is important to note that dexamethasone does not have any mineralocorticoid activity. Addition of a mineralocorticoid is not usually required, but may be considered when hyponatremia is significant and the patient has proven primary adrenal failure. The Thyroid Axis Several changes in circulating thyroid hormone concentrations occur in acute critical illnesses including brain injury. The conversion of T4 (thyroxine) to T3 (triiodothyronine) in peripheral tissues is dramatically reduced and an altered form of T3, reverse T3 (rT3), is generated. These changes appear immediately after brain injury, 473 Intensive Care in Neurology and Neurosurgery can persist for at least 2 weeks and may normalize after the acute illness has resolved. True "central" hypothyroidism occurs in 4 to 15% of patients following brain injury. In critically ill burn or medical patients, acute thyroid hormone replacement therapy was not shown to produce short-term improvement. Therefore, based on current evidence we do not recommend thyroid hormone replacement in the acute phase of brain injury. In a recent randomized, prospective, double blind, placebo controlled study by Hatton et al. The magnitude of the decline in testosterone was correlated with head trauma severity in some studies but not in others. The current data suggest that these changes in the gonadotropic axis in the acute phase of brain injury are adaptive and transient; therefore, gonadotropin replacement is not recommended in the acute phase. Although the mechanism and the effects are not known, this response is thought to be adaptive. In critically ill patients, the main clinical findings are increased daily urinary volume (>3 litres) and hypernatremia. If volume is significantly reduced, hypernatremia may cause weakness, altered mental status, seizures and coma. The urine is inappropriately diluted for the degree of serum osmolality, usually urine osmolality < 200 mOsm/kg and specific gravity < 1005 with plasma osmolalite >295 mOsm/kg. The effectiveness of the treatment is established by measuring urinary volume and plasma sodium concentration. Early diagnosis and treatment of posterior pituitary dysfunction after brain injury is important for maintaining water homeostasis and electrolyte balance in critically ill patients. Rotational acceleration-deceleration can cause shearing injury of axons, as commonly seen in the midline structures of the brain. In nontraumatic brain injury, evidence for the possible mechanisms of pituitary dysfunction is lacking; however, vascular injury seems to be the most possible cause in the pathogenesis of nontraumatic brain injury. The exact mechanisms of acute hormonal response and pituitary dysfunction due to brain injury remain to be elucidated and further clinical and experimental studies are warranted. Clinical findings consistent with a cortisol concentration < 15 µg/dl (410 nmol/l) are accepted as a diagnostic value for adrenal insufficiency. At a later stage deficiency of any and multiple anterior pituitary hormones can occur, a problem that can be difficult to recognize and may only be identified with specific endocrine testing. These axes will be discussed in turn focussing on the prevalence and consequences of dysfunction both early and later in the course of acute cerebral injury. In conditions that directly damage the adrenal, the response to this test is poor due to direct impairment of cortisol production. Anesthetics can impair these responses even if the pathways are anatomically intact.