Zebeta
General Information about Zebeta
Zebeta, also identified by its generic name bisoprolol, is a beta-blocker that works by blocking the motion of certain chemical compounds in the body that may improve blood stress and heart fee. This results in a lower in blood strain, making it an efficient remedy for hypertension. Zebeta is on the market as an oral tablet and is usually taken as quickly as a day with or with out meals.
Like any treatment, Zebeta has a few potential unwanted side effects, though not everybody experiences them. Common unwanted effects include headache, fatigue, dizziness, diarrhea, and nausea. These unwanted side effects are often mild and subside with continued use, but when they persist or turn into bothersome, it's important to tell a physician. Rare however severe unwanted effects embrace issue respiratory, chest pain, and irregular heartbeats. If any of those happen, search immediate medical consideration.
Many people with hypertension have no signs and might solely know their blood strain levels by way of common check-ups with their doctor. If left untreated, high blood pressure can lead to critical health issues similar to heart illness, kidney illness, and stroke. Zebeta should be taken exactly as prescribed by a doctor, and regular monitoring of blood pressure is critical to ensure the medication is working successfully.
High blood strain, also referred to as hypertension, is a common situation that affects hundreds of thousands of individuals worldwide. It is a significant threat factor for cardiovascular diseases such as coronary heart assault and stroke. Therefore, it is very important successfully manage and control high blood pressure to scale back the danger of these life-threatening circumstances. One medicine that has been confirmed to be efficient in treating high blood pressure is Zebeta.
Zebeta is often utilized in combination with other antihypertensive medication to attain better blood stress management. It works nicely with diuretics (water pills), calcium channel blockers, or angiotensin-converting enzyme (ACE) inhibitors. Combining these drugs can have a synergistic impact, resulting in better blood strain administration. However, it is essential to consult a well being care provider earlier than starting any new medication or changing the dosage of current ones.
Aside from treating hypertension, Zebeta has also been found to have other useful results. It is used to prevent chest pain (angina) and to enhance survival after a heart attack. It has additionally proven to be effective in treating coronary heart failure, a situation the place the guts is unable to pump sufficient blood to meet the physique's needs. By slowing down the center price and reducing the workload of the center, Zebeta might help enhance heart perform and symptoms related to these situations.
In conclusion, Zebeta is a extremely effective and secure treatment for treating hypertension. It helps lower blood strain levels and reduce the danger of coronary heart assault, stroke, and other cardiovascular illnesses. It is a well-tolerated treatment, with minimal unwanted effects, and can be utilized together with different antihypertensive drugs for higher blood stress control. However, it's important to take Zebeta as prescribed and to work intently with a well being care provider to watch blood stress ranges and regulate the dosage if necessary. With correct use and administration, Zebeta can significantly enhance the standard of life for individuals with hypertension.
Extrathoracic bypass may have better midterm freedom from graft failure than endovascular intervention blood pressure in spanish cheap zebeta 10 mg online. Endovascular interventions offer tangible benefits regarding cost, level of invasiveness and subjective patient satisfaction. Although the precise indications for endovascular intervention versus operative reconstruction need to be defined, an endovascular first approach is commonly accepted. Durability of endovascular therapy for proximal stenosis of the supra-aortic arteries. Common carotid artery occlusion treatment: Revealing a gap in the current guidelines. Thomas J Takach, George J Reul, Denton A Cooley, J Michael Duncan, James J Livesay, Igor D Gregoric. Brachiocephalic reconstruction I: Operative and long-term results for complex disease. Prevalence and prognosis of asymptomatic vertebral artery origin stenosis in patients with clinically manifest arterial disease. Nonfocal symptoms are more frequent in patients with vertebral artery than carotid artery stenosis. Clinical and hemodynamic significance of innominate artery lesions evaluated by ultrasonography and digital angiography. The value of aortic arch study in the evaluation of cerebrovascular insufficiency. Percutaneous endovascular treatment of innominate artery lesions: A single-centre experience on 77 lesions. Transthoracic reconstruction of the great vessels using minimally invasive technique. The superiority of synthetic arterial grafts over autologous veins in carotid subclavian bypass. Transthoracic repair of innominate and common carotid artery disease: Immediate and long-term outcome for 100 consecutive surgical reconstructions. Cervical reconstruction of the supraaortic trunks: A 16-year experience (discussion). Atherosclerotic innominate artery occlusive disease: Early and long-term results of surgical reconstruction. Aorticorigin reconstruction of the great vessels: Risk factors of early and late complications. Technical principles of direct innominate artery revascularization: A comparison of endarterectomy and bypass grafts. Angioplasty and primary stenting of the subclavian, innominate, and common carotid arteries in 83 patients. Stenting for occlusion of the subclavian arteries: Technical aspects and follow-up results Tex Heart Inst J. Determinants of immediate and long-term results of subclavian and innominate artery angioplasty. Endovascular treatment of atherosclerotic arterial stenoses and occlusions of the supra-aortic arteries: Mid-term results from a single center analysis. Percutaneous transluminal angioplasty of the brachiocephalic vessels: Guidelines for therapy. Carotid axillary artery bypass: An option following failed open and percutaneous procedures. Stenting of vertebrobasilar arteries in symptomatic atherosclerotic disease and acute occlusion: Case series and review of the literature. A heterogeneous group of extracranial carotid arteriopathies, both congenital and acquired, occur relatively infrequently and may produce ischemic central nervous syndromes virtually indistinguishable from those of atherosclerotic origin. The symptomatic loop or coil, carotid kink and spontaneous carotid dissection are among these unusual entities potentially responsible for carotid flow impairment or embolization. This chapter examines the carotid loop or coil, carotid kink and spontaneous dissection, emphasizing anatomic and pathophysiologic details, diagnostic dilemmas and contemporary medical or surgical management controversies. Central to an understanding of the development of the arterial tree is an appreciation of the development and regression of the dorsal aortas, appearing initially as symmetrical and parallel conduits destined to transform into the adult vascular form by as early as the 14 mm embryo stage. The dorsal aortas run parallel to the primitive foregut and fuse with the truncus arteriosus, forming the aortic sac, which contributes branch arteries to each developing pharyngeal arch. The third aortic arch ultimately forms the common carotid artery and the proximal internal carotid artery; the distal internal carotid system is formed by the cranial portion of the dorsal aorta. The external carotid artery sprouts from the third aortic arch, which joins with remaining portions of the first and second arches. Early in development, the communication between the third and fourth aortic arches the carotid duct becomes obliterated, and the extracranial carotid system assumes its adult configuration. These primordial vascular changes and cardiogenesis occur in the cephalad region of the embryonic pharynx. Developmental elongation of the fetal neck subsequently leads to descent of the heart into the mediastinum, with elongation of the innominate and carotid arteries. Maldescent of the heart or persistence of embryonic anatomy is thought responsible for subsequent looping and redundancy of the internal carotid artery. The anomaly is found in approximately 15% of children studied, with the prevalence rising to 25% of adults.
Although it has been proposed that dyspnea associated with ticagrelor was related to direct adenosine-like effects or possibly to inhibition of erythrocyte adenosine uptake hypertension medical definition buy discount zebeta on line, the observations with elinogrel make this unlikely. One speculation is that repeated reversible occupation of P2Y12 stresses and destroys platelets leading to pulmonary sequestration and lung injury similar to transfusion-related acute lung injury. Stimulation of the conformational change from inactive form to the active receptor capable of binding fibrinogen is the key event leading to platelet aggregation and secondary hemostasis. They have similar efficacy profiles and similar risks hemorrhage and therapy-induced thrombocytopenia. Thrombocytopenia, when it does develop, resolves more rapidly in a few days with the reversible inhibitors but may persist for 2 weeks with abciximab. It also binds to Mac-1 receptors on monocytes and neutrophils, leading to impaired monocyte function in vitro. Compared to placebo bolus/infusion, abciximab bolus/ infusion reduced the primary endpoint incidence 35% (from 12. Major bleeding was more common in the group receiving both abciximab bolus and infusion (14%) than either the abciximab bolus alone (11%) or placebo (7%). The study was terminated early, as subjects in the placebo arm experienced an event rate of 11. There was no significant difference in major bleeding between groups, although minor bleeding was more frequent in subjects receiving abciximab and standard-dose heparin. It was stopped early due to a higher incidence of 30-day ischemic events in the placebo arm (15. All three studies showed the same pattern, fewer periprocedural ischemic complications associated with an increased risk for bleeding with abciximab compared to placebo. It was one of the first drugs whose development can be traced to pharmacophore-based virtual screening in which libraries of small molecules have their binding affinity to a protein active assessed by purely computational methods. Its plasma halflife is approximately 2 hours, but the platelet-binding halflife is very short, such that its effects on platelet function dissipate within 48 hours. The incidence of the composite endpoint was significantly higher with tirofiban than abciximab (6. This led to a marked decrease in clinical use and the sale of the drug by Merck to another company and further changes in ownership through 2006, when it was acquired by Medicure. The overall results showed equivalence to abciximab and eptifibatide, but with significantly higher rates of thrombocytopenia with abciximab. Initially, two dose regimens for eptifibatide after 180 g/kg bolus administration (1. Overall bleeding was higher in the eptifibatide group, with moderate or severe bleeding occurring in 12. Subjects were treated with aspirin and loaded with clopidogrel or ticlopidine prior to stenting. Follow-up at 1 year showed maintenance of the benefit; the incidence of the composite endpoint was 22. Recommended dosing is to initially load with two bolus doses (180 g/kg) 10 minutes apart followed by infusion of 2 g/kg/min. Inhibition of platelet aggregation falls to less than 50% 4 hours after stopping infusion; bleeding times remain elevated for more than 6 hours. All three drugs are equally recommended as they are regarded as similar in efficacy and the risks of bleeding. Another compound, atopaxar, has been evaluated in phase 2 clinical trials but is not approved. Despite being a reversible antagonist, due to a prolonged effective half-life of 34 days and terminal half-life of 8 days, continued inhibition of thrombininduced aggregation >50% is seen up to 4 weeks, making zorapaxar the longest-acting platelet inhibitor currently marketed. With a median follow-up of 502 days, life table analysis showed the risk of the primary endpoint at 2 years was 19. Subjects were allowed concomitant treatment with aspirin alone or a thienopyridine alone or both. Vorapaxar significantly reduced the composite endpoint when compared to placebo regardless of planned thienopyridine therapy (planned thienopyridine odds ratio 0. Moderate or severe bleeding risk was increased with vorapaxar and was not significantly altered by planned thienopyridine use (odds ratio 1. While receptor antagonism may be more specific, interference with cytoplasmic signal pathways may induce broader effects that suppress activation independent of the initial stimulus. The terminal half-life is about 1012 hours and a wide variability in plasma levels has been observed at standard doses. Some reports indicate that standard oral dose regimens (100 mg four times daily or 200 mg extended release formulations twice daily) do not achieve adequate plasma levels to induce significant inhibit platelet function93 although platelet survival is definitely prolonged in patients with prosthetic heart valves94 indicating some degree of inhibition of platelet activation. Neither the degree of inhibition of platelet activity induced by dipyridamole nor the influence of the wide heterogeneity in plasma levels found with various dose regimens has been studied in relation to clinical outcomes. The most common side effects were dizziness, which possibly is related to effects on blood pressure. Bleeding was no greater in frequency with warfarin plus dipyridamole than with warfarin alone. It is unclear, however, whether warfarin plus dipyridamole is better than warfarin plus aspirin. The subsequent European Stroke Prevention Study 2 followed 6302 subjects for 2 years assigned to one of four treatment arms: placebo, aspirin (25 mg twice daily), dipyridamole (extended release 200 mg twice daily) or combined aspirin and dipyridamole. Compared to placebo, the combined risk for stroke and death was reduced 13% with aspirin (p = 0. Headache was more common with dipyridamole and the primary cause of study discontinuation. During the trial, 34% of the aspirin and dipyridamole group discontinued therapy due to adverse events or side effects (primarily headache) compared to 13% on aspirin alone.
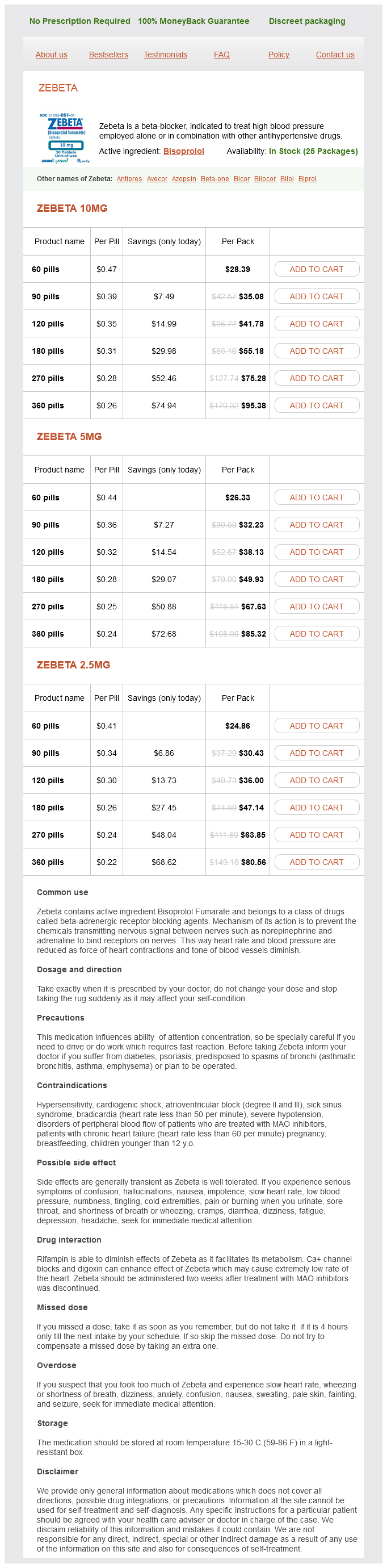
Zebeta Dosage and Price
Zebeta 10mg
- 60 pills - $28.39
- 90 pills - $35.08
- 120 pills - $41.78
- 180 pills - $55.18
- 270 pills - $75.28
- 360 pills - $95.38
Zebeta 5mg
- 60 pills - $26.33
- 90 pills - $32.23
- 120 pills - $38.13
- 180 pills - $49.93
- 270 pills - $67.63
- 360 pills - $85.32
Zebeta 2.5mg
- 60 pills - $24.86
- 90 pills - $30.43
- 120 pills - $36.00
- 180 pills - $47.14
- 270 pills - $63.85
- 360 pills - $80.56
General anaesthesia is usually employed although cervical plexus block arteria vesicalis superior order zebeta 10 mg free shipping, as for carotid endarterectomy, has been described. Two factors favour aggressive management: the inability to predict which tumours are, or will become, malignant and the significant reduction in complication rates with modern surgery. Preoperative tumour embolization and radiotherapy are employed in some centres and are worthy of discussion. It is possible that reports describing the efficacy of radiotherapy are subject to either selection. Nonetheless, results from several small series are broadly comparable to those of surgery: One series of 10 cases (1 post-operative) demonstrated no tumour growth or metastasis after a mean follow-up of 8 years. It is unsurprising that these have led others to conclude that radiation therapy is best reserved for inoperable or recurrent tumours. These include embolization with a variety of materials (Onyx, coils) or deployment of a covered stent in the external carotid artery to occlude the ascending pharyngeal artery. This is limited to cases where its origin is not Other cervical paragangliomas 567 local metastasis. However, if identification of lymph node spread is required, octreotide scintigraphy is likely to be more accurate and avoids lymphadenectomy. Also at risk are the facial and accessory nerves and the cervical sympathetic trunk. Baroreflex failure after excision of the carotid body or vagus nerve can be a serious complication, precipitating hyper- or hypotension and/or orthostatic tachycardia. Clonidine can be used to manage such cases, however, this only reduces the frequency of attacks, and many patients have lifelong problems. Resection is facilitated by using bipolar dissecting scissors to enhance haemostasis. Meticulous attention is paid to identifying and preserving the hypoglossal, glossopharyngeal and recurrent laryngeal nerves. This technique allows the tumour to be pulled forward, allowing ligation of posterior feeding vessels. The tumour is then separated from the carotid bifurcation in the sub-adventitial plane. The author reported a significant reduction in blood loss and cranial nerve injury in a non-randomized trial. Further, the technique may be helpful in cases where the tumour involves part or all of the carotid bifurcation making identification of a dissection plane difficult. In a small proportion of patients, when the bifurcation is encased by tumour, en bloc resection may be required. On these occasions, an appropriate length of great saphenous vein (circa 10 cm) should be harvested for vascular reconstruction before the resection commences. Further, since histological examination of the tumour offers little insight as to whether it is malignant, routine post-operative radiotherapy is not recommended. Further, the slow-growing nature of the tumour suggests that the interval between post-operative assessments is unlikely to be critical. Finally, when genetic profiling of a resected tumour is positive, first-degree relatives of affected individuals should be offered counselling and screening. Glomus jugulare tumours arise from the jugular foramen of the temporal bone and glomus tympanicum from the middle ear. Both typically present with tinnitus or hearing loss and usually present 568 Carotid body tumours to otorhinolaryngologists. However, invasion of the jugular vein or internal carotid artery may prompt vascular referral. Glomus vagale are the least common cervical paraganglioma and are tumours of the vagal nerve. Again, involvement of vascular structures will necessitate a multidisciplinary approach to treatment. Reconstruction of internal carotid artery in a patient with intermittent attacks of hemiplegia. Surgical resection of carotid body tumours: Long term survival, recurrence and metastasis. Neurological complications in carotid body tumors: A 6-year single-center experience. Genetic testing should be offered to relatives of patients who have positive tests. Patients should be followed up for at least 5 years and this should include an annual ultrasound scan. Carotid body tumors in inhabitants of altitudes higher than 2000 meters above sea level. A comparison between the treatments of functional and nonfunctional carotid body tumors. Bilateral carotid body tumour: the role of fine needle aspiration biopsy in the preoperative diagnosis. Muhm M, Polterauer P, Gstottner W, Temmel A, Richling B, Undt G, Niederle B, Staudacher M, Ehringer H. Martinelli O, Irace L, Massa R, Savelli S, Giannoni F, Gattuso R, Gossetti B, BenedettiValentini F, Izzo L. Radiotherapy in the management of chemodectomas of the carotid body and glomus vagale. Transfemoral transarterial onyx embolization of carotid body paragangliomas: Technical considerations, results, and strategies for complication avoidance.