Zenegra
General Information about Zenegra
Zenegra begins working inside half-hour to an hour after ingestion and may last for up to 4 hours. Individual response to the medicine might vary, and some males could expertise longer or shorter effects. It is beneficial to take Zenegra on an empty abdomen, as food can delay its onset of motion.
ED is a typical situation that impacts millions of men worldwide. It is characterized by the lack to get or preserve an erection during sexual activity. Many components can contribute to ED, including bodily and psychological causes. While there are various remedy choices out there, Zenegra is a extensively prescribed treatment for ED because of its effectiveness and safety profile.
In men with ED, this process is disrupted, resulting in difficulties in achieving or maintaining an erection. Zenegra works by inhibiting an enzyme called phosphodiesterase type 5 (PDE-5), which is liable for breaking down a chemical referred to as cyclic guanosine monophosphate (cGMP). cGMP is essential within the erectile course of as it helps to chill out the penile muscles and increase blood circulate to the penis. By inhibiting PDE-5, Zenegra permits for greater ranges of cGMP, resulting in better blood circulate to the penis and a firmer erection.
In conclusion, Zenegra is a well-tolerated and effective medicine for ED. It does not have an effect on the response to sexual stimulation but helps the body respond better to sexual arousal. It works by rising blood circulate to the penis, leading to a stronger and longer-lasting erection. However, it is very important notice that Zenegra isn't a treatment for ED and does not address underlying causes. It solely supplies temporary reduction and should be used as directed by a healthcare skilled.
While Zenegra has proven to be extremely efficient in treating ED, it is not with out potential unwanted effects. Common unwanted aspect effects embody headache, flushing, dizziness, nausea, and abdomen upset. Most of those unwanted aspect effects are delicate and momentary, but when they persist or turn out to be bothersome, it's important to hunt medical advice.
To perceive how Zenegra impacts the response to sexual stimulation, it is important to first understand the physiology of an erection. When a man is sexually aroused, the mind sends indicators to the nerves in the penis, inflicting the muscle tissue within the penis to chill out. This rest permits the arteries in the penis to widen, growing blood move into the erectile tissue. As a result, the penis turns into firm and erect. After ejaculation or when sexual stimulation stops, the muscular tissues contract, and blood move decreases, inflicting the erection to subside.
Zenegra, also recognized by its generic name Sildenafil, is a medication used to treat erectile dysfunction (ED) in men. It works by increasing blood circulate to the penis, allowing for a stronger and longer-lasting erection. However, Zenegra just isn't an aphrodisiac � it doesn't enhance sexual desire or have an effect on the response to sexual stimulation. Instead, it helps to facilitate a pure response to sexual arousal.
It is important to notice that Zenegra does not create an automatic erection. Sexual stimulation continues to be necessary for the medication to work. It acts as a facilitator, helping the body reply better to sexual arousal. Therefore, the efficacy of Zenegra relies on sexual stimulation to stimulate the release of nitric oxide from nerve endings in the penis, which then triggers the manufacturing of cGMP.
Urinary Continence During Abdominal Pressure Increases During voluntarily initiated micturition jacksonville impotence treatment center purchase generic zenegra pills, the bladder pressure becomes higher than the outlet pressure, and certain adaptive changes occur in the shape of the bladder outlet with consequent passage of urine into and through the proximal urethra. One could reasonably ask: Why do such changes not occur with increases in intravesical pressure that are similar in magnitude but that are produced only by changes in intra-abdominal pressure such as straining or coughing First, a coordinated bladder contraction does not occur in response to such stimuli, emphasizing the fact that increases in total intravesical pressure are by no means equivalent to emptying ability. Second, for urine to flow into and through the proximal urethra in an individual who does not have sphincteric incontinence, there must be (1) an increase in intravesical/detrusor pressure that is primarily a product of a coordinated, neurally mediated bladder contraction and that is (2) associated with characteristic tension and conformational changes in the bladder neck and proximal urethral areas. Assuming that the bladder outlet is competent at rest, a major factor required for the prevention of urinary leakage during increases in intra-abdominal pressure is the presence of at least equal pressure transmission to the proximal urethra (the mid-urethra as well in women) during such activity. This phenomenon was first described by Enhorning (1961) and has been confirmed in virtually every urodynamic laboratory since that time. Failure of this mechanism is an invariable correlate of effort-related urinary incontinence in women and men. The urethral closure pressure increases with increments in intra-abdominal pressure, indicating that active muscular function related to a reflex increase in striated sphincter activity or other factors that increase urethral resistance is also involved in preventing such leakage. A more complete description of the factors involved in sphincteric incontinence can be found later in this chapter, in Chapter 110, and in the work of Koelbl et al. Emptying/Voiding Emptying/voiding can be voluntary or involuntary and involves an inhibition of the spinal somatic and sympathetic reflexes and activation of the vesical parasympathetic pathways, the organizational center for which is in the rostral brainstem. Initially, there is a decrease in outlet resistance, mediated not only by the cessation of the somatic and sympathetic spinal reflexes but possibly also by a relaxing factor released by parasympathetic stimulation or by some effect of bladder smooth muscle contraction. A highly coordinated, parasympathetically induced contraction of the bulk of the bladder smooth musculature occurs, with shaping or funneling of the relaxed outlet, at least partially because of smooth muscle continuity between the bladder base and the proximal urethra. With amplification and facilitation of the bladder contraction from other peripheral reflexes and from spinal cord supraspinal sources, and in the absence of anatomic or functional obstruction between the bladder and urethral meatus, complete emptying occurs. There are some types of dysfunction that represent combinations of filling/storage and emptying/voiding abnormalities. However, within this scheme these have become readily understandable and detectable, and the treatment dilemmas have been logically described. The system can be easily expanded and made more detailed to include etiologic or specific urodynamic connotations (Box 111. However, the simplified system is perfectly workable and avoids argument in complex situations in which the exact cause or mechanism for a dysfunction cannot be established. Using this concept, all aspects of urodynamic and videourodynamic evaluation can be conceptualized regarding exactly what they evaluate in terms of either bladder or outlet activity during filling/storage or emptying/voiding (Table 111. Treatments can be classified under these broad categories as to whether they facilitate filling/storage or emptying/voiding and whether they do so by acting Sensory Aspects Most of the afferent input from the bladder and urethra reaches the spinal cord through the pelvic nerve and dorsal root ganglia, and some reaches the spinal cord through the hypogastric nerve. Afferent input from the striated muscle of the sphincter and pelvic floor travels in the pudendal nerve. The most important afferents for initiating and maintaining normal micturition are those in the pelvic nerve, relaying to the sacral spinal cord. These convey impulses from tension, volume, and nociceptive receptors located in the serosal, muscle, and urothelial and suburothelial layers of the bladder and urethra. In a neurologically normal adult, the sensation of filling and distention, but not urgency or pain, develops during normal filling/storage and initiates the reflexes responsible for emptying/ voiding (see Chapter 110) (Birder et al. An increase in outlet resistance occurs by means of the striated sphincter somatic guarding reflex. Involuntary contractions (detrusor overactivity) (1) Neurologic disease, injury, or degeneration (2) Bladder outlet obstruction (3) Increased afferent input or sensitivity (4) Inflammation (5) Increased neurotransmitter release (6) Increased sensitivity to transmitter (7) Decreased inhibitory pelvic floor activity (8) Idiopathic b. Decreased compliance (1) Neurologic disease or injury (2) Fibrosis (3) Bladder muscle hypertrophy (4) Idiopathic c. Combination (genuine stress urinary incontinence and intrinsic sphincter deficiency) C. Combination primarily on the bladder or on one or more components of the bladder outlet (Boxes 111. Filling and Storage Failure Absolute or relative failure of the bladder to fill with and store urine adequately results from bladder overactivity (involuntary contraction and/or decreased compliance), decreased outlet resistance, heightened or altered sensation, or a combination. Bladder Overactivity Overactivity of the bladder during filling/storage can be expressed as phasic involuntary contractions, as low compliance, or as a combination. Involuntary contractions are most commonly seen in association with neurologic disease or injury, bladder outlet obstruction, stress urinary incontinence (perhaps because of sudden entry of urine into the proximal urethra, eliciting a reflex contraction), or aging (probably related to neural degeneration), or they may be truly idiopathic. However, they may also be associated with increased afferent input related to inflammation or irritation of the bladder or urethral wall or an increased sensitivity (decreased threshold of activation to a normal amount of transmitter). Excitatory neurotransmitters may be released from the urothelium during filling/storage and activate afferent receptors/ nerves, ultimately resulting, in some individuals, in involuntary contractions or altered (heightened) sensation: a premature sensation of distention or fullness, true urgency (a sudden compelling desire to void, which is difficult to defer), or pain. Decreased compliance during filling/storage may be secondary to neurologic injury or disease, usually at a sacral or infrasacral level but may result from any process that impairs or destroys the viscoelastic or elastic properties of the bladder wall. As such, a compliance abnormality can be seen with increased collagen deposition resulting from longstanding bladder outflow obstruction. Filling and Storage Failure Resulting From Altered Sensation Bladder-related storage failure may also occur in the absence of overactivity because of increased afferent input from inflammation, irritation, other causes of hypersensitivity, and pain. One classic example is termed bladder pain syndrome (also known as interstitial cystitis; see Chapter 57). In this scheme, uroflow and residual urine integrate the activity of the bladder and the outlet during the emptying phase. Outlet Underactivity Decreased outlet resistance may result from any process that damages the innervation of structural elements of the smooth or striated sphincter, or both, or damages or impairs the support of the bladder outlet in women.
This information supports the notion that tumor grade is the most important prognostic factor and erectile dysfunction shots zenegra 100 mg purchase mastercard, although stage cannot be directly assessed, noninvasive disease can be expected in most cases of lowgrade tumor. A final concern is whether ureteroscopy promotes progression or spread of disease to other urothelial surfaces or metastatic sites. There have been reports of increased tumor appearance in refluxing ureters of patients with bladder tumors (de Torres Mateos et al. However, Kulp and Bagley (1994) reported on 13 patients who underwent multiple ureteroscopic treatments followed by nephroureterectomy; they found no unusual propagation of cancer in the specimens. Concerns that ureteroscopy may promote metastatic spread were raised by Lim et al. Three general approaches can be used for tumor ablation: bulk excision with ablation of the base, resection of the tumor to its base, and diagnostic biopsy followed by ablation with electrocautery or laser energy sources. Specimens are frequently minute and should be placed in fixative at once and are specially labeled for either histologic or cytologic evaluation (Tawfiek et al. Next, the tumor base is treated with either electrocautery or laser energy sources. This technique is especially useful for low-grade papillary tumor on a narrow stalk. Only the intraluminal tumor is resected, and no attempt is made to resect deep (beyond the lamina propria). Extra care is necessary in the mid-ureter and upper ureter, where the wall is thin and prone to perforation. The tumor is adequately sampled with forceps and sent to the pathology laboratory for diagnostic evaluation. Multiple biopsy specimens are often required when small, flexible 3-Fr biopsy forceps are used. Electrocautery delivered through a small Bugbee electrode (2 or 3 Fr) can be used to fulgurate tumors. However, the variable depth of penetration can make its use in the ureter dangerous, and circumferential fulguration should be avoided because of the high risk of stricture formation. Its shallow penetration may, however, make its use cumbersome with larger tumors, especially in the renal pelvis. The safety margin is significantly lower and can limit its use in the ureter, where the ureteral wall is thin. A ureteral stent is placed for a variable duration to aid with the healing process. Results There are no published series of randomized controlled trials comparing endoscopic therapy and nephroureterectomy, and all are case series (level 4 evidence). Disease Antegrade Nephroureteroscopic the percutaneous approach was first described by Tomera et al. The main advantage of the percutaneous approach is the ability to use larger instruments that can remove a large volume of tumor in any portion of the renal collecting system. The tumor is engaged and removed, with care taken not to avulse the adjacent ureter. With either of these techniques, the base is treated with electrocautery or a laser energy source. The technique differs from the technique for bladder tumors in that only intraluminal tumor is resected. In general, laser energy is preferred because it has more reliable delivery of energy and depth of penetration. The two most commonly used energy sources are holmium:yttrium-aluminum-garnet and neodymium:yttrium-aluminum-garnet. Chapter 99 Surgical Management of Upper Urinary Tract Urothelial Tumors 2215 staging as well as grading is usually possible. In addition, a percutaneous approach may avoid the limitations of flexible ureteroscopy, especially in complicated calyceal systems or areas difficult to access, such as the lower pole calyx or the upper urinary tract of patients with urinary diversion. With a percutaneous approach, the established nephrostomy tract can be maintained for immediate postoperative nephroscopy and administration of topical adjuvant therapy. The main disadvantages are the increased morbidity compared with ureteroscopy and the potential for tumor seeding outside the urinary tract. Establishment of the nephrostomy tract has inherent risks, and the procedure usually requires inpatient admission. Distinct risks related to a percutaneous approach are loss of urothelial integrity and exposure of nonurothelial surfaces to tumor cells. This open system provides the possibility of tumor implantation in the nephrostomy tract. Disease in the renal pelvis and upper ureter is best approached through an upper or middle pole access to allow scope maneuvering through the collecting system and down the ureteropelvic junction. The tract is dilated by either sequential (Amplatz) or balloon 1 A Technique and Instrumentation Establishment of the Nephrostomy Tract. Cystoscopy is performed, and an open-ended ureteral catheter is positioned in the pelvis. If the patient is in the prone split-leg position, a flexible ureteroscope can be passed to the desired area and renal access obtained under direct and fluoroscopic guidance. Position of the nephrostomy is imperative for successful percutaneous resection of transitional cell carcinoma of the renal collecting system and upper ureter and requires careful preoperative evaluation of radiographs for tumor location. Tumors in peripheral calyces (A to C) are best approached by direct puncture as far distally in the calyx as possible. Tumors in the renal pelvis (D) and upper ureter (E) are best approached by puncture to an upper (1) or middle (2) calyx, which allows the scope to be maneuvered in the renal pelvis and down the ureter. Complete nephroscopy is performed with rigid and flexible endoscopes when necessary. After identification, the tumors are removed by one of the following three techniques.
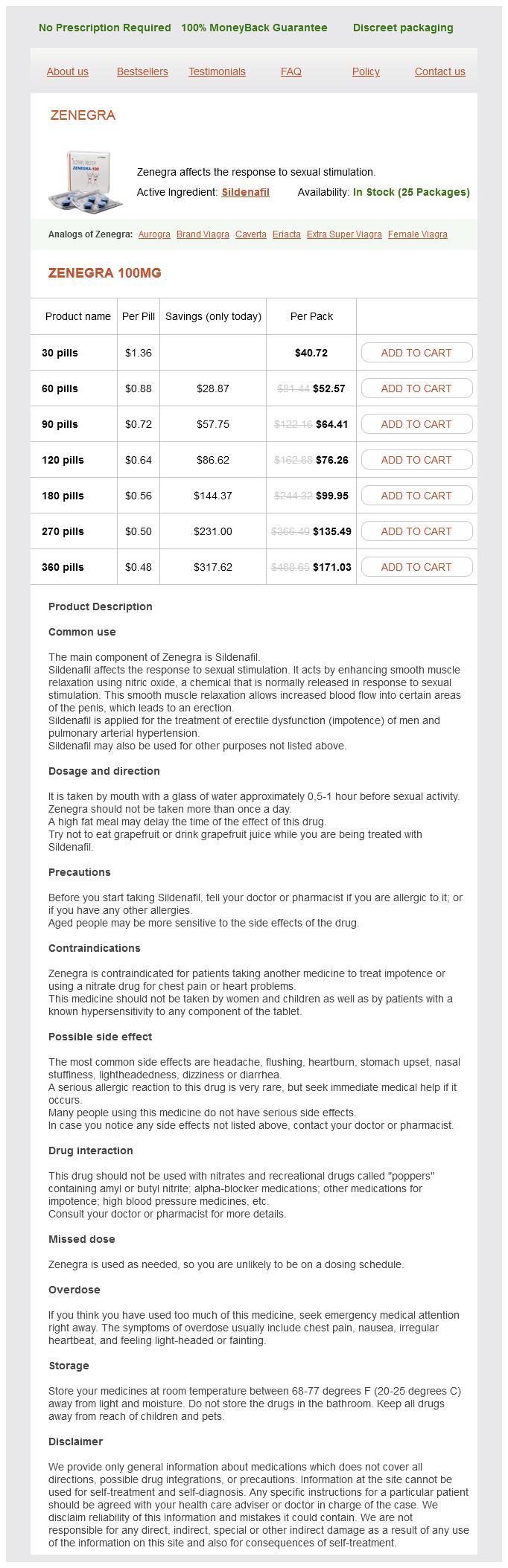
Zenegra Dosage and Price
Zenegra 100mg
- 30 pills - $40.72
- 60 pills - $52.57
- 90 pills - $64.41
- 120 pills - $76.26
- 180 pills - $99.95
- 270 pills - $135.49
- 360 pills - $171.03
Some women habitually void by Valsalva erectile dysfunction specialist order discount zenegra, believing that they need to bear down to push urine out and empty the bladder. Patients with dysfunctional voiding need to understand that pushing is not necessary and may be counterproductive. Actively contracting the muscles demonstrates the sensations associated with muscle tension and assists patients to discriminate and contrast it with the sensations of relaxation. Once they are able to feel the muscle release and relax, the patient can begin coordination of muscle relaxation following a contraction. Fluid Management Fluid intake plays a role in the prevention of several urinary system diseases, and adverse effects on the urinary system can result from insufficient hydration. Excessive fluid intake can be a problem when large-volume intake triggers symptoms of urgency, frequency, or incontinence (Segal et al. In a study of healthy young men, those with excessive fluid intake had not only significantly increased urine volume and frequency but also significantly elevated bladder pressure on ambulatory urodynamics (Schmidt et al. Some people increase their fluid intake deliberately in an effort to "flush" their kidneys or lose weight. In practice, it is more common to see inadequate fluid intake, because people with bladder problems often restrict their intake in an effort to control symptoms. Working women also report limiting fluid intake as strategies to avoid urinary symptoms (Fitzgerald et al. Fluid intake should be regulated to 6 to 8 8-ounce glasses or 30 cc/kg body weight per day with a 1500 mL/day minimum at designated times unless contraindicated by a medical condition. The Institute of Medicine issued a report (2005) with guidelines for total water intake for healthy people. This food versus fluid component has been a source of confusion for the public and professionals, with a misperception of fluid source as only deriving from beverage intake. Although overall fluid restriction is not a good strategy, it can be very helpful to restrict fluids at particular times when toilet access will be limited, such as before a social outing. Patients using temporary fluid restriction should be encouraged to keep their total daily fluid intake optimized, by making up the missed fluids earlier or later. Avoiding excessive fluid intake in the evening hours can also be helpful for reducing nocturia. In patients who retain fluid during the day and have nocturia resulting from mobilization of fluid during sleep, behavioral interventions focus on managing daytime accumulation of fluid. Patients are advised to wear support stockings to prevent accumulation of edema fluids or to elevate the lower extremities in the late afternoon to mobilize the fluid well before bedtime. In some patients, a mid- to late afternoon loop diuretic is useful to complete diuresis before bedtime. For patients who are already taking a loop diuretic, nocturia can often be improved by altering the timing of the diuretic (so that most of the effect has occurred before bedtime). Loop diuretics are also known to aggravate incontinence by increasing the rate of bladder filling and producing sudden urges. Such effects can sometimes be avoided by discontinuing the diuretic, changing to a non-loop diuretic, or altering the timing of administration. An example is taking the loop diuretic in the later afternoon or after coming home from work so that diuresis can be accomplished during the evening, but before bedtime. Although fluid management is widely used in clinical practice, there is little scientific evidence on fluid intake related to bladder health. When patients decreased their fluid input by 25%, there was a significant reduction in daytime frequency (23%), urgency (34%), and nocturia (7%). Increasing fluid input by 25% and 50% resulted in a worsening of daytime frequency but had no effect on urgency, nocturia, or urgency incontinence. In a study of women with urodynamically confirmed idiopathic detrusor overactivity (n = 30), decreasing fluid intake significantly decreased voiding frequency and urgency incontinent episodes (Swithinbank, Hashim, and Abrams, 2005). Caffeine Reduction Caffeine plays a role in symptoms of urgency, frequency, and urgency incontinence partly because it is a diuretic and partly because it is a bladder irritant for many people. The consumption of caffeinated beverages, foods, and medications is easily underestimated. Caffeine is found in many foods and drinks that people consume daily, particularly coffee and tea. Caffeine is consumed regularly by more than 85% of adults in the United States (Mitchell et al. Approximately 73% of children consume caffeine on a given day, and coffee and energy drinks represent a greater proportion of caffeine intake than soda intake, which has declined (Branum et al. Urodynamic studies have shown that caffeine increases detrusor pressure (Creighton and Stanton, 1990) and is a risk factor for detrusor overactivity (Arya et al. Similarly, daily administration of oral caffeine (150 mg/kg) resulted in detrusor overactivity and increased bladder sensory signaling in the mouse (Kershen et al. Women who had increased coffee intake by at least 2 servings/ day had 64% higher odds of progression of urgency. There is also evidence that reducing caffeine intake can help to reduce episodes of stress and urgency incontinence (Bryant et al. Other Dietary Irritants Although data are scarce, there are a number of other substances that are thought to irritate the bladder, including sugar substitutes (aspartame), citrus fruits, highly spiced foods, and tomato products. There are innumerable clinical cases in which these substances appear to be aggravating urgency and incontinence, and reducing them has provided clinical improvement.