Zyvox
General Information about Zyvox
While Zyvox is mostly well-tolerated, as with all medicine, it does carry some dangers. Some of the common unwanted aspect effects related to this antibiotic embody headache, nausea, diarrhea, and vomiting. In rare instances, it might additionally cause more severe unwanted facet effects corresponding to allergic reactions, low blood cell rely, and peripheral neuropathy.
Zyvox is not recommended to be used in pregnant or breastfeeding ladies, in addition to those with sure medical circumstances similar to kidney illness or hypertension. It is essential to reveal any underlying medical circumstances to your doctor before beginning treatment with this antibiotic.
It is important to comply with the prescribed dosage and length of remedy when taking Zyvox to avoid any potential unwanted effects. It can be important to inform your physician about another medications you may be taking as they might work together with Zyvox.
Zyvox is often used to deal with infections such as pneumonia, pores and skin infections, bone and joint infections, and certain kinds of food poisoning caused by bacteria. It may be used in combination with other antibiotics to deal with more serious infections.
One of the principle advantages of Zyvox is its capacity to treat infections brought on by multi-drug resistant bacteria. Due to its distinctive mechanism of action, it is ready to successfully fight micro organism that have turn into resistant to different kinds of antibiotics.
This treatment is out there in both oral and intravenous varieties, making it a flexible remedy possibility for a spread of infections. It is usually used in hospital settings to treat bacterial infections that are immune to other forms of antibiotics.
In conclusion, Zyvox is a potent antibiotic that has proven to be efficient in treating cussed bacterial infections caused by Enterococcus and Streptococcus. With its ability to combat multi-drug resistant bacteria, it has turn into an important tool within the fight against bacterial infections. However, it is essential to take this treatment as prescribed and report any unwanted facet effects to your physician for correct management.
Zyvox works by interfering with the production of certain proteins that are essential for the expansion and multiplication of bacteria. By inhibiting this process, the antibiotic is prepared to effectively kill the micro organism and stop the infection from spreading.
Enterococcus is a sort of bacteria commonly discovered within the gastrointestinal tract, as well as within the skin and respiratory tract. Streptococcus is a group of micro organism that can cause a variety of infections, together with strep throat, pneumonia, and pores and skin infections.
Zyvox, also referred to as linezolid, is a strong antibiotic belonging to the oxazolidinones class. It is often used to treat bacterial infections caused by Enterococcus and Streptococcus bacteria.
The authors concluded that there is no difference in efficacy and safety for epinephrine versus norepinephrine plus dobutamine in the management of septic shock virus envelope order zyvox 600 mg amex. Vasopressin is an agent that has both vasoconstriction and antidiuretic properties. Vasopressin constricts vascular smooth muscle directly via V1 receptors and may also increase the responsiveness of the vasculature to endogenous or exogenous catecholamines. Exogenous administration of low-dose vasopressin can have a dramatic hemodynamic response in this scenario, rapidly restoring arterial pressure. The low dose vasopressin was then continued while the norepinephrine was weaned as allowed. This trial was primarily targeted to detect any renal failuresparing effect that vasopressin might offer. There was no difference in mortality or renal failurefree days between the two groups. Phenylephrine may be useful in select patients with severe dysrhythmias associated with catecholamine infusion because it has no -adrenergic effects, as well as in patients with refractory hypotension in the presence of a known high cardiac index. All the patients were receiving conventional vasopressor support (primarily norepinephrine) at the time of enrollment. Maximum doses in any individual patient should be considered based on physiologic response and side effects. Corticosteroids Administering high doses of steroids (30 mg/kg of methylprednisolone) failed to show an outcome benefit in septic shock in large-scale randomized controlled trials in the 1980s. Relative adrenal insufficiency in the context of septic shock may predispose a patient to persistent cardiovascular failure that is refractory to conventional hemodynamic Inotropic Support Inotropic support may be required for patients with septic shock. On the other hand, administration of exogenous steroids could be associated with deleterious effects such as immunosuppression or myopathy. Being a "nonresponder" was a better predictor of death than an initially low cortisol value. In a randomized controlled trial by the same investigators in 2002, 300 severely ill (persistent hypotension despite fluid resuscitation and vasopressor initiation) patients with septic shock were randomly assigned to 7 days of hydrocortisone plus fludrocortisone versus placebo. The 2016 Surviving Sepsis Campaign guidelines suggest against the use of low-dose hydrocortisone (200 mg/day) if fluid resuscitation and vasopressors are able to restore hemodynamic stability. Since the publication of these guidelines a recent New England Journal of Medicine study randomly assigned 3800 mechanically ventilated patients with septic shock to a continuous daily infusion of 200 mg hydrocortisone versus placebo. There was no difference in any of the secondary endpoints with the exception of faster resolution of shock and fewer transfusions in the steroid-treated patients. There was no evidence of increase in secondary infections (bacteremia or fungemia) in the steroid group. It is noteworthy that there was no steroid signal with more severe versus less severe illness or earlier versus later treatment. Patients taking higher doses of catecholamines did have better outcomes in the steroid-treated group compared to patients using lower doses of catecholamines. This large study was stellar in design, execution, and reporting but will unlikely end the debate about utility of steroids in select patients with septic shock. There was an increase in vasopressor-free days in the steroid treatment group as well as increase in hyperglycemia, the latter common to all trials of steroids versus placebo in septic shock. Despite the fact that low-dose steroids do not consistently improve clinical outcome in clinical trials, septic shock patients receiving sustained high doses of norepinephrine or multiple vasopressors may benefit. Modulation of the Host Response the toxin, primary mediator, and secondary mediator cascade thought to drive infection-induced organ dysfunction is elaborate and often redundant. A multitude of studies since the late 1980s have targeted modulation of the host response due to the premise that organ dysfunction and mortality in severe sepsis and septic shock are based on a disorganized host response to microbial toxin. More recently attention has turned toward immune enhancement in select patient populations in whom organ dysfunction and secondary infections may be driven by immune suppression with resultant morbidity and mortality. Efforts continue to unravel the molecular biology of severe sepsis and the potential to leverage that knowledge for patient benefit. Summary the systemic changes seen in sepsis are driven initially by the proinflammatory and procoagulant responses. Septic shock is a composite of hypovolemic, cardiogenic, and vasodilatory shock with the potential for intracellular mitochondrial dysfunction. Management includes restoring intravascular volume losses, both capillary leak (absolute loss) and venodilation (functional loss). Vasopressors may be required if blood pressure is not restored with fluid administration. The balance of fluids and vasopressors to maintain mean arterial pressure is controversial and currently more of an art than a science. Corticosteroids, although controversial, do lead to earlier shock reversal but without proven mortality benefit and may be useful in select patients with more severe shock. Despite failure to date with clinical trials testing novel interventions targeting the sepsis cascade, study continues looking for success in this area. Remarks: Reassessment should include a thorough clinical examination and evaluation of available physiologic variables (heart rate, blood pressure, arterial oxygen saturation, respiratory rate, temperature, urine output, and others, as available) as well as other noninvasive or invasive monitoring, as available. We suggest that dynamic over static variables be used to predict fluid responsiveness, where available (weak recommendation, low quality of evidence). We suggest guiding resuscitation to normalize lactate in patients with elevated lactate levels as a marker of tissue hypoperfusion (weak recommendation, low quality of evidence).
Placement of a central catheter is therefore essential in patients with hemorrhage caused by polytrauma or with other forms of acute bleeding antibiotics vs probiotics zyvox 600 mg purchase free shipping. It also allows irritant or hypertonic fluids to be administered, such as parenteral solutions, potassiumenriched solutions, and some therapeutic agents. Central venous lines also can be convenient in patients who need prolonged intravenous therapy when peripheral venous access becomes problematic. The femoral artery can be easily cannulated and gives a better signal, but the presence of a femoral catheter interferes more with patient mobility and warrants concern about infection. This strategy did not result in improved outcomes in three large randomized controlled trials,1012 which included patients who were already resuscitated and already had normal ScvO2 values. The normal value in healthy persons is very low, not exceeding 5 mm Hg in the patient breathing spontaneously. The so-called early goal-directed therapy in septic shock was initially proposed by Rivers et al. In the presence of unilateral pathology, the catheter must be introduced on the affected side. Arterial puncture resulting in a local hematoma is not uncommon, but hematoma formation usually is without major consequences. Bedside ultrasonography can help guide the introduction of the catheter into the vein. Adherence to basic hygiene guidelines can decrease the incidence of catheter-related sepsis. Triple-lumen catheters may be associated with a higher incidence of catheter-related infection,15 primarily as a result of increased catheter manipulation. The use of antimicrobial-coated catheters may decrease the risk of infections,16 but fears remain about the risks of development of resistant organisms. The c wave, caused by closure of the tricuspid valve, follows the a wave and is coincident with the beginning of ventricular systole. The y descent reflects the opening of the tricuspid valve and passive atrial emptying. This is the dicrotic notch characteristic of the pulmonary arterial (and also the systemic arterial) waveform. Nevertheless, a number of steps must be taken to ensure the adequacy of the measurement. The next question is whether the measured pressure is truly a transmural pressure-that is, the pressure difference between the vascular structures and the environmental structures. In other words, will changes in surrounding intrathoracic pressures influence the pressures measured In the case of intrathoracic pressures, the changes in pleural pressure are particularly relevant. Hence, all measurements should be performed at end-expiration, when the pleural pressure is closest to zero. A marked fall in intrapleural pressure, as with a Mueller maneuver (forced inspiration against resistance), may dramatically increase the transmural pressures. However, these assessments of end-diastolic volumes do not provide additional information about the likelihood of fluid responsiveness. In sum, then, a given level of cardiac filling pressures does not provide much information about fluid responsiveness, but monitoring can be very helpful to guide a fluid challenge. The true capillary pressure may be estimated from the measurement of the intersection point of the rapid and slow pressure decay curves recorded after a rapid interruption of the blood flow; such measurements of capillary pressure are possible from the pressure trace. This pressure is well correlated with extravascular lung water in animal experiments. The need to know these values is questionable, however, because the primary goal remains to keep these hydrostatic pressures as low as possible while maintaining adequate cardiac output. It may be lower in patients with aortic regurgitation or higher in the presence of significant tachycardia or mitral valve disease. A stiff, noncompliant ventricle can result in a relatively high end-diastolic pressure for a given enddiastolic volume. An evaluation of end-diastolic volumes can be obtained less invasively with echocardiographic techniques. Likewise, the use of transthoracic thermodilution techniques allows the Cardiac Output the reference method for measurement of cardiac output is use of the Fick equation; however, this equation is difficult to apply in practice. Indocyanine green clearance has been used for many years, but this method is time-consuming and quite difficult to perform. The thermodilution technique developed by Ganz is a convenient technique that today allows the almost continuous measurement of cardiac output. The presence of tricuspid insufficiency is the major limitation to this technique. Other techniques, including transpulmonary and lithium dilution techniques, have been developed but are somewhat less precise. The thermodilution technique estimates cardiac output over several cardiac cycles, whereas other techniques, including those based on pulse contour analysis, may assess beat-to-beat variations. These techniques may be useful for estimating the influence of changes in intrathoracic pressures on the stroke volume variation, an estimate of fluid responsiveness. With knowledge of the stroke volume, it becomes easy to calculate the end-systolic and end-diastolic volumes.
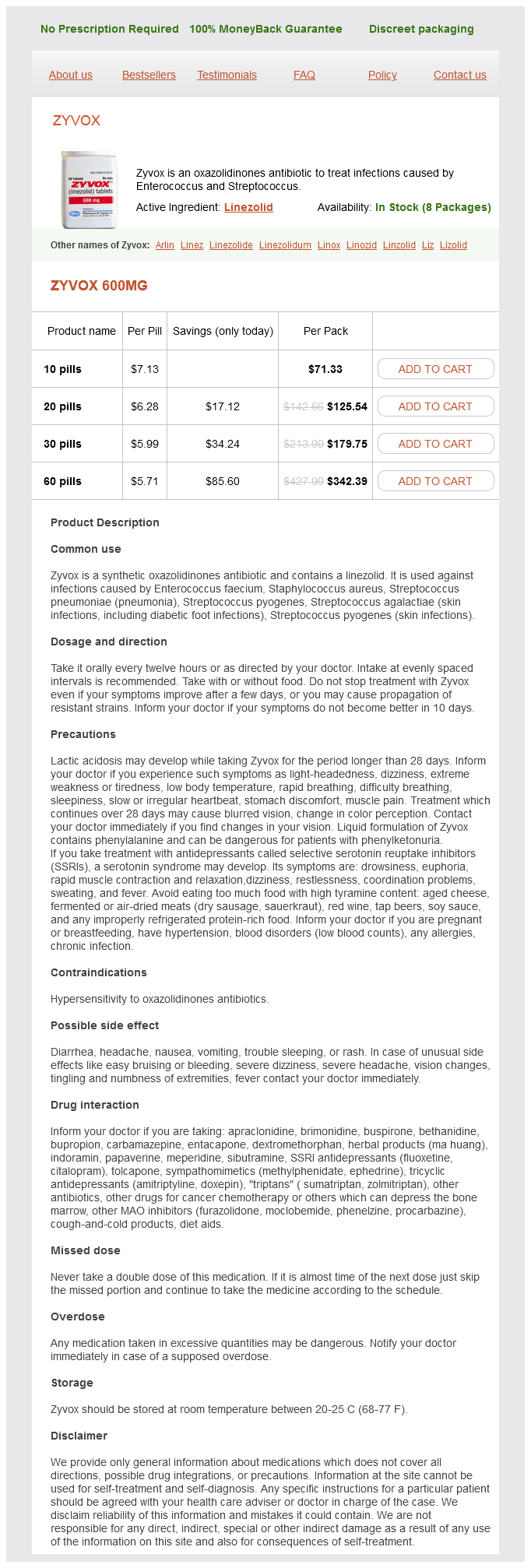
Zyvox Dosage and Price
Zyvox 600mg
- 10 pills - $71.33
- 20 pills - $125.54
- 30 pills - $179.75
- 60 pills - $342.39
The result of this "misread" can be dangerous virus news proven 600 mg zyvox, as placement of chest tube into a large bullae will result in a large bronchoatmospheric fistula that will likely need surgical control to seal. Drainage Systems the original drainage system was a single-bottle system consisting of a water seal and drainage bottle. As demonstrated, chest radiography alone can confuse clinicians as to a potential diagnosis of pneumothorax with ensuing complication of large bronchopleural fistula if a chest tube is mistakenly inserted in the belief that the bullae is a pneumothorax. The modernization of this three-chamber system is found in single compartmentalized boxes such as those made by Atrium (Atrium Medical Corp. Both allow connection to various degrees of suction that can be manipulated on the side of the device. The factory setting is -20 mm Hg, which corresponds to a negative pressure generated with a 20-cm column of water in the original three-bottle system. Proponents argue that these devices lead to earlier chest tube removal and decreased hospitalization. Finally, water sealequivalent options exist for patients with prolonged air leak, defined as leak persisting longer than 5 days after intervention, who can be discharged home with adequate control of the pleural space. Optimal Chest Tube Size for Drainage Chest drains are usually divided into two size categories: largebore (>20F) or small-bore (20F). The Fanning equation (= 2r5P/fl, were is the flow, r is the radius, l is the length, P is the pressure, and f is the friction factor) determines the flow of the moist gas (such as in a pneumothorax) or liquid with turbulent flow through the tube. These function similarly and utilize the principles of the three bottle collection system. If the diameter of the tube is doubled, flow increases by a factor of 16, implying that a small increase in the size of the drainage tubes would result in substantial improvements in the flow rates. The internal diameters (bore) and the length of the tube, which may vary according to the manufacturer, are obviously key determinants for the successful drainage of pleural collections. However, equally important are the characteristic of the drained material, its formation rate, the ability of the tube to remain patent, and for all or the majority of the collection being drained to be in communication with the tube. However, review of the published literature suggests that small-bore tubes are at least as effective as large tubes for most indications. Furthermore, small-bore tubes are easier to insert, they cause less pain for the patient both during insertion and while in place, and they appear to have a lower risk of complications. Small-bore catheters may also complement larger tubes that have drained most of the chest but have left small residual pockets, which would be difficult to access blindly with large, less flexible tubes. Technique of Chest Tube Insertion Small-Bore Tube Thoracostomy Small-bore chest tubes (<20F) are inserted using a catheter system such as the catheter-over-needle and the catheter-over-guidewire (Seldinger) technique. The procedure begins with patient positioning after explaining the procedure and obtaining informed consent. Several positions are used; the most important issue is accommodating overall comfort of patient and operator. Patients could be positioned to sit on the bed with their back straight and upright with arms resting on a pillow placed on a table in front of them. The general teaching approach is that insertion should be attempted one interspace below the spot where tactile fremitus is lost and the percussion note becomes dull. One must recognize, however, that the position of the diaphragm in the supine and lateral decubitus positions can be as high as the fourth intercostal space. In case of a pneumothorax, the catheter is inserted in the second anterior intercostal space, mid-clavicular line. Pleural ultrasonography is a safe and simple noninvasive technique for determining the presence of pleural fluid and identifying the insertion site. It can be performed at the bedside and can provide information about the quantity and the quality of pleural fluid, including the presence of loculations and the precise location of loculated pockets. Studies have shown that complications are decreased with ultrasound guidance, including in patients receiving antiplatelet agents. The selected site is cleaned thoroughly with antiseptic solution and sterile draping is applied. It is essential to anesthetize the skin, intercostal space, and the parietal pleura with a satisfactory amount of local anesthetic. A short 25-gauge needle is used to raise a small wheal with 1% lidocaine at the selected site. Then a long 22-gauge needle is advanced through the wheal directly over the rib with gentle aspiration. Lidocaine is injected every 2 to 4 mm as the needle is advanced until a small amount of fluid or air comes up into the syringe, at which point the needle is then removed. Depicted are two common positions: (A) with arm across body and (B) with arm in abduction. Clinicians must be familiar with the type of tube and deployment system used to allow for safe tube thoracostomy. In case of a pneumothorax, the catheter is directed toward the apex, whereas in case of pleural effusion, it is directed inferiorly and posteriorly into the costal diaphragmatic recess. When the Seldinger technique is used, an 18-gauge hollow needle is advanced until fluid is obtained and then a guidewire is passed through the needle into the space. After removal of the needle, a small incision is made and then a dilating catheter is threaded over the guidewire and advanced using a twisting movement. A third technique for insertion uses a chest tube mounted on a sharp-tipped trocar. The whole unit is advanced until parietal pleurae are reached and then the catheter is advanced while the trocar is held in place. Pneumovac canister After obtaining consents and prepping and draping the patient, we routinely identify and mark the fifth intercostal space at the mid to anterior axillary line. The scapula is shown at the top of the screen, as are the posterior and anterior axillary lines along with the sixth intercostal space (which was used for this particular chest tube insertion).